Professional Documents
Culture Documents
2016 Importance of Wide Re-Resection in Adult Spermatic
Uploaded by
nelsonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2016 Importance of Wide Re-Resection in Adult Spermatic
Uploaded by
nelsonCopyright:
Available Formats
THE JOURNAL OF UROLOGY
Vol. 195, No. 4S, Supplement, Monday, May 9, 2016
e843
PD34-12
IMPORTANCE OF WIDE RE-RESECTION IN ADULT SPERMATIC
CORD SARCOMAS: REPORT ON ONCOLOGIC OUTCOMES AT A
SINGLE INSTITUTION
Katie Murray*, Emily Vertosick, Massimiliano Spaliviero,
Joseph Mashni, Daniel Sjoberg, Harry Herr, Paul Russo,
Jonathan Coleman, New York, NY
Source of Funding: None
PD34-11
CLINICOPATHOLOGIC FEATURES AND PROGNOSTIC FACTORS
IN PATIENTS WITH PENILE CANCER WHO UNDERWENT
INGUINAL LYMPHADENECTOMY WITH HISTOLOGICALLY
NEGATIVE LYMPH NODES
^nio Zequi, Gustavo Guimara
~es,
Giuliano Aita*, Teresina, Brazil; Ste
~o Paulo, Brazil
Walter da Costa, Isabela Cunha, Fernando Soares, Sa
INTRODUCTION AND OBJECTIVES: The presence and
extent of involvement of inguinal lymph nodes (LN) are the most
important prognostic factor for the survival of patients with penile cancer
(PC). However, despite the fact that the patients tested negative LN
suggests a quite favorable evolution comparing to those with positive
LN, the absence of lymph node metastasis is not an absolute guarantee
of treatment success. A portion of these patients had locoregional
recurrence or even tumor progression. The inuence of the factors
related to the primary tumor in the evolution of patients with histologically negative LN in PC is unknown. This study aims to study the clinicopathologic characteristics of this population or their respective
primary tumors and prognostic factor for overall survival (OS), cancer
specic survival (CSS) and disease-free survival (DFS).
METHODS: A retrospective analysis of medical records of 279
patients with PC treated at the Department of Pelvic Surgery, Hospital
~o Paulo - SP) between 1953 and 2012 underwent
AC Camargo ( Sa
amputation and histologically- negative LN ( pN0 group, 165 patients) or
clinically-negative and followed for a period minimum of 3 years (cN0
group, 96 patients). The pathological material was reviewed by expert
pathologists. The clinicopathological variables in addition to the standard invasive front according to the criteria and modied by Anneroth
and Bryne.
RESULTS: 67 deaths occurred during the follow-up in cN0
Group, 6 of them occurred by cancer. The 10 year-OS, CSS and DFS
were respectively 59.7%, 96.4% and 95.2%. In this group (cN0), the
presence of high grade tumor was independent risk factor of death by
cancer (hazard ratio (HR) 2.05; p0,006) and risk of cancer recurrence
(HR 1.44; p0,01). 44 deaths occurred during follow-up in pN0 group,
12 of them occurred by cancer. The 10 year-OS, CSS and DFS were
respectively 52.7%, 87.1% and 86%. The front invasion inltrating was
associated with a lower CSS ( p 0.027 ) and lower DFS (p 0.019 ) in
pN0 group in univariate analysis.
CONCLUSIONS: In patients with histologically negative LN the
pattern of invasion inltrating was associated with increased tumor
recurrence and cancer-specic mortality. The presence of high-grade
tumor was an independent unfavorable prognostic factor for DFS and
for CSS in patients with clinically negative LN. The cN0 patients had
better 10-year-OS, CSS and DFS than the pN0 ones and tended to
present more favorable demographic, clinical and pathological
characteristics.
Source of Funding: None
INTRODUCTION AND OBJECTIVES: We report on a single
cancer centers 30-year experience with the rare disease of sarcoma of
the spermatic cord. The objective of this study was to evaluate the
outcomes of surgery, including surgery with adjuvant radiation, on
survival.
METHODS: We reviewed records of 81 consecutive patients
treated between 1981 and 2011 at Memorial Sloan Kettering Cancer
Center for spermatic cord sarcoma. We found that 72 patients were
evaluable after excluding those with metastatic disease and those not
undergoing surgical intervention. Recurrence-free and cancer-specic
survival was calculated for patients who underwent wide surgical reresection within 5 months of diagnosis. Univariate Cox regression
models were constructed to assess the relationship of age, tumor size,
tumor histology, adjuvant radiation, and wide surgical re-resection with
recurrence and death. The Kaplan-Meier method was used to estimate
recurrence and survival probabilities.
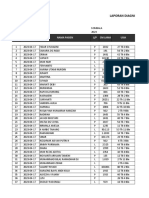
RESULTS: Median patient age at rst surgery was 60 years
(IQR 50e68). High-grade tumors were evident in 46 patients (64%).
Wide surgical re-resection was performed in 67% (48) of patients within
5 months of diagnosis. A signicant improvement in recurrence-free
survival was identied in those undergoing wide surgical re-resection
(HR 0.16, 95% CI 0.07e0.37; p <0.0001), shown in Figure 1. After
examining possible sources of bias, we found that patients receiving
wide re-resection had higher grade disease but still received an RFS
benet from wide re-resection. Positive surgical margin status at wide
re-resection was strongly associated with both disease recurrence (HR
5.56, 95% CI 1.14, 27.11, p0.034) and death from cancer (HR 6.16,
95% CI 1.25, 30.29, p0.025). We did not observe a signicant difference in recurrence-free or cancer-specic survival between patients
who received adjuvant radiation therapy and those who did not (p0.4
and p0.9).
CONCLUSIONS: A wide surgical re-resection with negative
margins is effective in the management of patients with spermatic cord
sarcoma and leads to improved recurrence-free survival.
Source of Funding: Sidney Kimmel Center for Prostate and
Urologic Cancers
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Angel NicoleDocument4 pagesAngel NicoleNicole FranciscoNo ratings yet
- Intensive Nursing Practicum: Bachelor of Science in NursingDocument7 pagesIntensive Nursing Practicum: Bachelor of Science in NursingMichelle Gliselle Guinto MallareNo ratings yet
- CBR - Role of PT & Physiotherapist (Ankita 1)Document39 pagesCBR - Role of PT & Physiotherapist (Ankita 1)Akshay Bangad50% (2)
- Nursing PresentationDocument74 pagesNursing PresentationHalima IliyasuNo ratings yet
- 5 Reptile Medicine and Surgery - Mader - 2nd EditionDocument1,258 pages5 Reptile Medicine and Surgery - Mader - 2nd EditionJoão Gabriel M. Alkmim100% (1)
- The Power of Mental Toughness Building The Foundation For SuccessDocument129 pagesThe Power of Mental Toughness Building The Foundation For Successcontact.iptvviewNo ratings yet
- Centering Before SessionDocument9 pagesCentering Before SessionJuanaNo ratings yet
- Feeding ProgramDocument20 pagesFeeding ProgramAnalyn DominguezNo ratings yet
- DraftRajasthan State Women PolicyDocument29 pagesDraftRajasthan State Women PolicyAADYA SHARMANo ratings yet
- Irc CVDocument4 pagesIrc CVEmbay AmareNo ratings yet
- DOH Administrative Order No 2021 0044Document17 pagesDOH Administrative Order No 2021 0044yy4wbgcq9cNo ratings yet
- El Exprime Hombres 2Document11 pagesEl Exprime Hombres 2Carlos GonzalezNo ratings yet
- MIE Safety Audit Checklists ReviewDocument16 pagesMIE Safety Audit Checklists ReviewjuvytimbalNo ratings yet
- 5 Page Essay ExampleDocument11 pages5 Page Essay ExampleToniNo ratings yet
- 5.1 Enzymes - Igcse Cie Biology - Ext Theory QPDocument11 pages5.1 Enzymes - Igcse Cie Biology - Ext Theory QPGaurang GargNo ratings yet
- Ebook Ekg Plain and Simple 4Th Edition Ellis Test Bank Full Chapter PDFDocument30 pagesEbook Ekg Plain and Simple 4Th Edition Ellis Test Bank Full Chapter PDFalexandercampbelldkcnzafgtw100% (6)
- My first crush, a production storyboardDocument9 pagesMy first crush, a production storyboardRonald Cristian Gamba Lozano100% (1)
- Peat 1Document42 pagesPeat 1Steve Colbert100% (3)
- Laporan Diagnosa Pasien Harian: Puskesmas: TanggalDocument9 pagesLaporan Diagnosa Pasien Harian: Puskesmas: TanggalRamlawatiNo ratings yet
- Plant and Equipment Risk Assessment Fgoc - NewDocument12 pagesPlant and Equipment Risk Assessment Fgoc - Newmajid khanNo ratings yet
- TINFC-2020-03 paragraph structure practiceDocument3 pagesTINFC-2020-03 paragraph structure practiceMuchamad SolehNo ratings yet
- Parcare Assessment MaxillofacialDocument22 pagesParcare Assessment Maxillofacialqta omerNo ratings yet
- Gambaran Dan Lesi Rahang Pada Radiograf: Border Periosteal ReactionDocument6 pagesGambaran Dan Lesi Rahang Pada Radiograf: Border Periosteal ReactionI Dewa Ayu SavitriNo ratings yet
- Hospital ListsDocument20 pagesHospital ListsErebius PtolemyNo ratings yet
- Chapter 47Document11 pagesChapter 47Aziil LiizaNo ratings yet
- EmpyemaDocument11 pagesEmpyemaJoha_AdeNo ratings yet
- Chemical Feed ProblemsDocument6 pagesChemical Feed ProblemsPowerbomb JonesNo ratings yet
- Sensory Processing DisorderDocument6 pagesSensory Processing Disorderapi-643181689No ratings yet
- Toxic Responses of The BloodDocument10 pagesToxic Responses of The BloodM. Joyce100% (2)
- Case Presentation ON Accelerated HypertensionDocument30 pagesCase Presentation ON Accelerated HypertensionJigeesha LakshmiNo ratings yet