Professional Documents
Culture Documents
Obesity TOG
Uploaded by
princessmeleana6499Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Obesity TOG
Uploaded by
princessmeleana6499Copyright:
Available Formats
TOG11_1_25-31-Stewart
24/12/08
The Obstetrician & Gynaecologist
04:20 PM
Page 25
10.1576/toag.11.1.25.27465 www.rcog.org.uk/togonline
2009;11:2531
Review
Review Obesity: impact on
obstetric practice and outcome
Authors Frances M Stewart / Jane E Ramsay / Ian A Greer
Key content:
Prepregnancy obesity is increasingly common.
More than half of all women who died from direct or indirect causes in the
200305 report, Saving Mothers Lives, were overweight or obese.
Obese mothers have an increased risk of complications.
Learning objectives:
To learn about the increased incidence of miscarriage, congenital malformation
and metabolic complications.
To learn about the increased risks of intrapartum complications.
Ethical issues:
Should medical assistance to conceive be withheld until BMI!35?
More of the healthcare budget should be spent on prevention rather than
treatment of obesity.
Keywords congenital abnormality / deep vein thrombosis / gestational diabetes
mellitus / hypertension / perinatal mortality
Please cite this article as: Stewart FM, Ramsay JE, Greer IA. Obesity: impact on obstetric practice and outcome . The Obstetrician & Gynaecologist 2009;11:2531.
Author details
Frances M Stewart MD MRCOG
Consultant, Obstetrics and Gynaecology
Antrim Area Hospital, Bush Road, Antrim,
County Antrim BT41 2RL, UK
Email: francesstewart1@hotmail.com
(corresponding author)
Jane E Ramsay MD MRCOG
Consultant in Obstetrics and Gynaecology
Ayrshire Maternity Unit, Crosshouse Hospital,
Kilmarnock KA2 OBE, UK
2009 Royal College of Obstetricians and Gynaecologists
Ian A Greer MD MRCP(UK) FRCP FRCPI FFFP
FMedSci FRCOG
Consultant in Obstetrics and Gynaecology
Hull York Medical School, University of York,
Heslington,
York YO10 5DD, UK
25
TOG11_1_25-31-Stewart
24/12/08
Review
04:20 PM
Page 26
2009;11:2531
The Obstetrician & Gynaecologist
Introduction
The 200305 report of the Confidential Enquiries
into Maternal Deaths in the United Kingdom1
highlighted obesity as a significant risk for
maternal death. More than half of all women who
died from direct or indirect causes were either
overweight or obese.
For the mother, obesity increases the risk of
obstetric complications during the antenatal,
intrapartum and postnatal period, as well as
contributing to technical difficulties with fetal
assessment (Box 1). The offspring of obese mothers
also have a higher rate of perinatal morbidity and
an increased risk of long-term health problems.
The epidemiology of obesity
The prevalence of obesity, defined as a body mass
index (BMI) "30 kg/m2, has significantly increased
during the last three decades, both in the USA and
other countries in the developed world.American
trends are now seen among the European population.
In a health survey of England,2 the Department of
Health reported that 32% of women aged 3564 years
are overweight (BMI 2530) and 21% are obese
(BMI #30). In a British Womens Heart and Health
Study,3 one-quarter of the 4000 participants in
England, Scotland and Wales were found to be
clinically obese. One-fifth of the women were inactive
and two-fifths did not eat one portion of fresh fruit a
day. The Department of Health has predicted that, if
current trends continue, by 2010, 6 million women in
England will be obese.2 In line with this, a large
Scottish maternity hospital has observed a two-fold
increase in the proportion of women with a booking
BMI #30 over the last decade.4 Obesity amongst
women is of worldwide concern, as shown in
Australia by Callaway et al.5 in 2006. They noted that
35% of Australian women aged 2535 years were
overweight or obese. Obesity accounts for #280 000
deaths annually in the USA and will, if current trends
continue, soon overtake smoking as the primary
preventable cause of death.6
Antenatal health issues
Obesity is associated with an increased risk of first
trimester and recurrent miscarriage and fetal
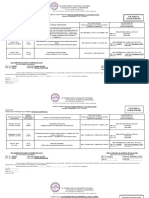
Box 1
Complications that are more
prevalent among obese women
before and during pregnancy
26
Prepregnancy
Menstrual disorders, infertility
Early pregnancy
Miscarriage, fetal anomalies, difficult and
less accurate ultrasound examination
Antenatal
Pregnancy-induced hypertension,
pre-eclampsia, gestational diabetes,
venous thromboembolism
Intrapartum
Induction of labour, shoulder dystocia,
caesarean section, operative
anaesthetic difficulties
Postpartum
Haemorrhage, infection, venous
thromboembolism
Fetal
Macrosomia, fetal distress, perinatal
morbidity and mortality, birth injury
anomaly, in both women with polycystic ovary
syndrome and those with normal ovarian
morphology. A meta-analysis7 of 13 studies looking
at gonadotrophin-induced ovulation in women
with normogonadotrophic anovulatory infertility
found obesity and insulin resistance to be the most
clinically useful predicting factors for poor clinical
outcome. The incidence of spontaneous miscarriage
has been reported to rise as insulin resistance
increases.8 It has been suggested that insulinsensitising agents, such as metformin, also reduce
miscarriage rates.9 One potential mechanism for
this observation is an increased production of
inflammatory and prothrombotic agents produced
by adipose tissue or released from endothelium
secondary to stimulation by adipocyte-derived
factors. It has been suggested that plasminogen
activator inhibitor-type 1 (PAI-1) is associated with
increased rates of miscarriage in association with
maternal obesity. Treatment with metformin
appears to reduce PAI-1 and miscarriage rates.10,11
Several studies have shown up to a two-fold
increase in risk for neural tube defects where there
is prepregnancy maternal obesity. The greater the
maternal BMI, the higher the risk of congenital
malformation.12 It is well recognised that maternal
diabetes is a risk factor for the development of
congenital abnormality, including central nervous
system defects. A cumulative effect on the risk of
central nervous system birth defects when maternal
obesity and gestational diabetes coexist has also
been highlighted. Anderson et al.13 evaluated an
American population in a case control study
(n$477). After adjusting for maternal ethnicity,
age, education, smoking, alcohol use and
periconceptional vitamin use, obese women still
had substantially increased risks of delivering
offspring with anencephaly (odds ratio [OR] 2.3,
95% CI 1.24.3), spina bifida (OR 2.8, 95% CI
1.74.5) and isolated hydrocephaly (OR 2.7, 95%
CI 1.55.0). When gestational diabetes was
examined in isolation, the only anomaly seen more
frequently was holoprosencephaly.
The mechanisms that link obesity and congenital
anomaly are not fully understood. Several possible
hypotheses have been suggested, one being the
prevalence of undiagnosed type II diabetes or
significant insulin resistance without frank glucose
dysregulation. Epidemiological data from both the
USA and Europe have suggested that 3050% of
adults with type II diabetes are undiagnosed. Some
studies suggest that prepregnancy diagnosis of
diabetes may permit appropriate intervention prior
to conception and that obese women planning a
pregnancy should be screened and offered a highdose folic acid supplement. One could postulate
that weight reduction and tight glycaemic control
could help reduce the rates of congenital
abnormality in this high-risk group.
2009 Royal College of Obstetricians and Gynaecologists
TOG11_1_25-31-Stewart
24/12/08
04:20 PM
Page 27
The Obstetrician & Gynaecologist
Ultrasound and obesity
Obstetric ultrasound is widely practised
throughout the developed world. Initially, its major
indications were pregnancy dating and detection of
multiple pregnancy and fetal growth restriction.
With improved resolution the detection of fetal
anomaly has become possible. The limitations of
obstetric ultrasound as a screening test are dictated
by the expertise of the clinician, the quality of the
equipment and the habitus of the woman. By
absorbing the associated energy, adipose tissue can
significantly attenuate the ultrasound signal.
Therefore, a high-frequency, higher-resolution
signal would be more significantly absorbed at a
lesser depth, sacrificing image quality and depth of
field. A worrying consequence of maternal obesity,
consequently, is the reduced sensitivity of
ultrasound as a screening test for fetal anomaly. In
1990, Wolfe et al.14 examined the efficacy of
scanning the obese pregnant population. They
showed that scans performed on women with a
BMI greater than the 90th centile during the second
and third trimester had a 14.5% reduction in
visualisation of organs compared with lean women.
This reduction was most marked when visualising
the fetal heart, umbilical cord and spine.
Hypertension
Independent of pregnancy, hypertensive disorders
are more prevalent in obese women than in their
lean counterparts. Elevated prepregnancy BMI is an
independent risk factor for the development of
pregnancy-induced hypertension.15 Even when the
degree of excess body fat is moderate, the incidence
of hypertension and pre-eclampsia is significantly
higher in comparison with control patients.16 Most
published work suggests a two- to three-fold
increase in the risk of pre-eclampsia with a
BMI #30. Waist circumference has also been
reported to be a sensitive predictive marker of
possible pregnancy hypertensive complications.
Sattar et al.17 examined early pregnancy body
composition data from 1142 pregnant women.
Odds ratios were calculated for risk of hypertensive
complications of pregnancy in association with a
waist circumference #80 cm at %16 weeks of
gestation. The risk of pregnancy-induced
hypertension was approximately doubled (OR 1.8,
95% CI 1.12.9) and of pre-eclampsia tripled
(OR 2.7, 95% CI 1.16.8) in association with
central obesity.
OBrien et al.16 identified 13 cohort studies,
comprising nearly 1.4 million women. The risk of
pre-eclampsia typically doubled with each
57 kg/m2 increase in prepregnancy BMI. This
relationship persisted in studies that excluded
women with chronic hypertension, diabetes
mellitus and multiple gestation, or after
adjustment for other confounding factors. A recent
systematic review by Cnossen et al.18 aimed to
2009 Royal College of Obstetricians and Gynaecologists
2009;11:2531
Review
determine the accuracy of maternal BMI in
predicting pre-eclampsia and to explore the
clinical potential for selecting women for
treatment with low-dose aspirin. A total of 36
studies, testing 1 699 073 pregnant women (60 584
with pre-eclampsia) were included. They found
that among women with a BMI #35 as the only
risk, the incidence of pre-eclampsia was only 3%,
resulting in 714 women needing treatment to
prevent one case of pre-eclampsia. When a woman
with a BMI #35 also had other risk factors,
however, such as primigravidity or diabetes, the
risk was greatly elevated and the number needed to
treat in order to prevent one case of pre-eclampsia
was only 37.18 This is a very useful paper for clinical
practice and it highlights the importance of
holistic evaluation of risk at booking for antenatal
care. Most studies within the literature conclude
that pregnancies amongst the obese population
should be considered high risk and appropriate
antenatal care provided. The need for
prepregnancy counselling and advice for this
group of women is highlighted repeatedly.
The mechanism of effect
As stated, obesity is a risk factor for many maternal
obstetric complications, including pre-eclampsia
and gestational diabetes. The mechanisms involved
are complex but one possible unifying hypothesis is
that there may be a syndrome of insulin resistance,
low-grade inflammation, dyslipidaemia and an
alteration in systemic microvascular function. This
metabolic and vascular derangement mirrors that
of the metabolic syndrome observed among those
with coronary heart disease and/or diabetes,
particularly in later life. In a prospective study,
Stewart et al.19 demonstrated that obese women
have a pro-inflammatory phenotype, with
impaired microvascular function, from early in
pregnancy. In lean women, inflammatory features
were acquired in later pregnancy. The excessive
inflammatory burden seen in the obese pregnant
woman may fuel this process, explaining some of
the increased association of obesity with preeclampsia and gestational diabetes.
Gestational diabetes mellitus and obesity
Gestational diabetes mellitus affects about 5% of all
pregnancies.20 In the NICE consultation
document21 on diabetes and pregnancy, a BMI #30
is considered a risk factor for the development of
gestational diabetes. The policy has changed from
offering no screening for gestational diabetes
mellitus to targeted screening in the healthy
maternal population, using clinical risk factors
(Box 2).
Striking data from a large prospective populationbased Swedish study,22 which included 151 025
women, warns of the implications of
interpregnancy weight gain. This study shows that
27
TOG11_1_25-31-Stewart
24/12/08
Review
Box 2
Criteria meriting antenatal
screening for gestational diabetes21
04:20 PM
Page 28
2009;11:2531
BMI # 30
Previous gestational diabetes
Previous macrosomic baby "4.5 kg
Family history of diabetes (first-degree relative with type 1
diabetes)
Belonging to a high-risk ethnic group, including:
South Asian (Indian, Pakistani, Bangladeshi)
Black Caribbean
Chinese
if an increase in maternal BMI of 12 units occurs
between pregnancies, the risk of gestational
diabetes rises by 2040%. If a woman weighs 63 kg
and is 1.65 m tall (BMI 23) and gains 3 kg before
her second pregnancy, her BMI rises by 1 unit and
her risk of gestational diabetes rises by #30%. If she
gains 6 kg and, therefore, becomes overweight
(gaining 2 BMI units), her risk of gestational
diabetes rises by 100%. If she becomes obese, her
risk of gestational diabetes rises by 200%.22
Effective treatment of gestational diabetes does
reduce the risk of macrosomia. Instrumental and
operative delivery rates, however, are increased even
in the absence of fetal macrosomia.23 Crowther
et al.24 conducted a randomised clinical trial to
determine whether treatment of women with
gestational diabetes mellitus reduced the risk of
perinatal complications. The rate of serious
perinatal complications was significantly lower
among the infants of subjects in the intervention
group than among the infants of the women in the
routine care group (1% versus 4%, P$0.01).24
If gestational diabetes mellitus is diagnosed, tight
metabolic control should be achieved through diet
and, when indicated, insulin therapy. Insulin
therapy is required more often in obese women
with gestational diabetes mellitus than in lean
women.25 Treatment using insulin reduces maternal
and fetal morbidity.26 Mothers who develop
gestational diabetes have a 50% higher risk of
developing diabetes during their lifetime27 and this
risk may be greatest in obese woman.28 For the
obese individual with gestational diabetes,
pregnancy offers an ideal opportunity to give them
future lifestyle advice in terms of exercise and
weight loss and, therefore, to reduce the potential
for vascular disease in the long term.
Intrapartum issues
Obesity and diabetes are independently associated
with adverse pregnancy outcomes. Rosenberg
et al.29 undertook a large population-based study.
Data were collected from the 1999, 2000 and 2001
New York City birth files for 329 988 singleton
births, containing information on prepregnancy
weight and antenatal weight gain. During
pregnancy, obese women are at increased risk of
several adverse perinatal outcomes, including
28
The Obstetrician & Gynaecologist
anaesthetic, perioperative and other maternal and
fetal complications.30 Obese women have higher
rates of induction of labour31 and failed induction
(7.9% versus 10.3% versus 14.6% with increasing
BMI).32 Caesarean section rates in nulliparous obese
women are higher than in lean women (20.7% in
the control group versus 33.8% in the obese group
and 47.4% in the morbidly obese group; P # 0.01).33
A higher rate of obstetric complications among
obese women has been reported, including
operative vaginal delivery (8.4% versus 11.4% and
17.3% with increasing BMI; P % 0.001), shoulder
dystocia (1% versus 1.8% and 1.9% with increasing
BMI; P % 0.021) and third/fourth-degree
lacerations (26.3% versus 27.5% and 30.8% with
increasing BMI; P % 0.001) compared with the
normal BMI group.32 The frequency of both elective
(8.5% versus 4%) and emergency caesarean section
(13.4% versus 7.8%) is almost doubled for very
obese women compared with the normal BMI
group.34 When other factors such as macrosomia,
nulliparity, induction or diabetes were accounted
for, maternal obesity was still found to influence the
mode of delivery independently.35 In another study
of 126 080 deliveries,36 after excluding women with
diabetes and hypertensive disease, there was a threefold increased risk of failure to progress in the first
stage and almost a trebling of caesarean section rate
from 10.8% to 27.8% (OR 3.2) among obese
women when compared with lean.
From the anaesthetic perspective, the risks of failed
epidurals, increased aspiration during general
anaesthesia and difficulty with intubation are the
most commonly cited compucations. Increased
rates of caesarean delivery, macrosomia, shoulder
dystocia, difficulty obtaining peripheral
intravenous access and inaccurate or difficult blood
pressure monitoring are also reported.37 Common
operative complications include loss of landmarks,
making vascular access difficult, and increased risk
of respiratory complications, such as aspiration and
pneumonitis. Increased retention of lipid-soluble
agents, increased drug distribution and more rapid
desaturation have also been reported.
The anaesthetist plays an important role in
preventing serious complications and must be
aware of the many potential hazards. Extra
vigilance is required to guide these women safely
through the perioperative period. There are very
few trials in the literature on the use of epidural and
spinal anaesthesia in the obese woman. Many case
reports exist on the difficulty of technique and
reductions in drug dosage requirements.
Postpartum issues
It is now recognised that adipose tissue produces a
variety of bioactive peptides, collectively termed
adipokines. Alteration of adipose tissue mass in
2009 Royal College of Obstetricians and Gynaecologists
TOG11_1_25-31-Stewart
24/12/08
04:20 PM
Page 29
The Obstetrician & Gynaecologist
obesity affects the production of most adiposesecreted factors: there is an increase in several
adipokines. Increased levels of angiotensinogen
have been implicated in hypertension; PAI-1 in
impaired fibrinolysis; and acylation-stimulating
protein, tumour necrosis factor-alpha, interleukin-6
and resistin in insulin resistance.38 Pregnancy is a
prothrombotic state, secondary to an increase in
activity of coagulation factors XII, X and VIII, as
well as fibrinogen.39 In the puerperium, deep
venous thrombosis, endometritis, postpartum
haemorrhage, prolonged hospitalisation and
wound infection and dehiscence are also seen with
increased frequency in obese women.37
The leading cause of maternal mortality remains
venous thromboembolism and the postpartum
period is the time of greatest risk, secondary to
vascular damage at childbirth. The coagulation
cascade is activated by inflammatory cytokines
causing endothelial activation and this is further
increased with obesity. Several studies have shown
that obese patients have higher plasma
concentrations of all prothrombotic factors
(fibrinogen, von Willebrand factor [VWF] and
factor VII), compared with non-obese controls,
with a positive association with central fat.40 It has
been proposed that the secretion of interleukin-6
by adipose tissue, combined with the actions of
adipose tissue-expressed tumour necrosis factoralpha in obesity, could underlie the association of
insulin resistance with endothelial dysfunction,
coagulopathy and coronary heart disease.40
Implications for the fetus of
the obese mother
Short-term
Lower Apgar scores have been reported in the
neonates of obese mothers compared with those of
lean mothers.41 Prepregnancy BMI is a strong
positive predictor of birthweight. In fact, the odds
ratio for an obese mother delivering a large-fordates infant is 1.418.41 Macrosomia increases the
risk of shoulder dystocia, birth injury and the
incidence of low Apgar scores and perinatal death.
A recent 3-year retrospective analysis42 examined
the mode of delivery of infants weighing #4000 g.
The incidence of caesarean section among the
macrosomic group was 25.8%, compared with
13.1% (P%0.0001) for the general population
during the study period.
Infants born to obese mothers are more likely to
require admission to a neonatal intensive care unit
(NICU). In a retrospective study carried out in
France,43 the percentage of infants requiring
admission to a NICU was 3.5 times higher when
maternal obesity was present. The higher incidence
of diabetes mellitus and gestational diabetes in the
obese population may contribute to this effect, with
2009 Royal College of Obstetricians and Gynaecologists
2009;11:2531
Review
an increased risk of neonatal admission to the NICU
for glycaemic control. The increased incidence of
macrosomia and consequent birth trauma may also
contribute to increased rates of perinatal morbidity
in the offspring of obese mothers.
One cohort study carried out in Denmark42
examined the relationship between maternal
prepregnancy BMI and the risk of stillbirth and
neonatal death. Maternal obesity was associated
with almost a three-fold increased risk of stillbirth
(OR 2.8, 95% CI 1.55.3) and neonatal death (OR
2.6, 95% CI 1.25.8) compared with women of
normal weight. Adjustment for maternal cigarette
smoking, alcohol and caffeine intake, maternal age,
height, parity, gender of the child, years of
schooling, working status and cohabitation with
the partner did not change the conclusions, nor did
exclusion of women with hypertensive disorders or
diabetes mellitus. No single cause of death
explained the higher mortality in children of obese
women but more stillbirths were either
unexplained intrauterine deaths or associated with
fetoplacental dysfunction among obese compared
with normal weight women.42
Long-term
Barkers hypothesis44 describes a theory of
intrauterine programming, which suggests that
babies who are small at birth or during infancy,
secondary to maternal starvation during
pregnancy, have increased rates of cardiovascular
disease and type 2 diabetes in adult life. Forsn
et al.45 examined the association between maternal
BMI and the risk of coronary heart disease in the
next generation. Men whose mothers had a high
BMI in pregnancy had an increased risk of
coronary heart disease. The highest death rates
were, therefore, in men who had a low birthweight
and a low placental weight but whose mothers had
a high BMI during pregnancy. The effects were
large and highly significant. While undernutrition
is uncommon in the developed world, obesity and
cardiovascular disease are common. The direct
effects of maternal obesity on fetal programming
are under-researched. The concept of fetal
programming being related to the quality of
nutrition, rather than the quantity, needs to be
addressed. One may hypothesise that, in addition to
maternal malnutrition secondary to famine,
malnutrition secondary to an inappropriate diet of
highly processed, high-fat food lacking in essential
vitamins and nutrients, i.e. the modern Western
diet, may contribute to long-term adult ill health of
offspring through fetal programming.
Cost implications
In 2000, a prospective study46 examined the cost of
care of 435 women seen consecutively within their
obstetric service. The average cost in terms of
29
TOG11_1_25-31-Stewart
Review
24/12/08
04:20 PM
Page 30
2009;11:2531
antenatal care and duration of hospital stay was five
times higher for women who had a higher
prepregnancy BMI compared with normal weight
controls and duration of hospital stay was 3.9 to
6.2fold higher among the overweight mothers.
The overall financial burden of obesity on the
National Health Service is difficult to determine. The
implications of rising rates of maternal obesity for
maternity services include increased medicalisation
of labour and delivery and greater pressure on
neonatal services and antenatal and postnatal beds.
Conclusion and
recommendations
It is essential that obstetricians have guidelines for
management of the obese woman. Obesity is a risk
factor for both gynaecological and obstetric
complications. A multidisciplinary approach to
management is necessary to decrease the risks of
morbidity and mortality. There are a number of
recommendations for clinical management prior to
and during pregnancy:
Provide prepregnancy counselling for morbidly
obese women (in primary care/subfertility/
recurrent miscarriage/diabetic clinics).
Consider high doses of folic acid (5 mg).
A healthy diet and exercise are important in
pregnancy: refer to a dietician, advise to avoid
excessive weight gain, consider screening for
diabetes.
Provide an early booking visit to plan pregnancy
management.
Prescribe low-dose aspirin in the presence of
additional clinical risk factors for pre-eclampsia.
Consider antenatal thromboprophylaxis if there
are additional clinical risk factors for venous
thromboembolic disease.
Recommend a detailed anomaly scan and serum
screening for congenital abnormality.
Consider glucose tolerance testing at 28 weeks,
with the potential for repeating it in later pregnancy.
This group of women requires both primary and
secondary care intervention if we are to limit or
even reverse the epidemic of obesity within Western
society.
References
1 Confidential Enquiry into Maternal and Child Health. Saving Mothers
Lives: Reviewing Maternal Deaths to Make Motherhood Safer
20032005. The Seventh Report of the Confidential Enquiries into
Maternal Deaths in the United Kingdom. London: CEMACH; 2007.
2 Department of Health. Health Survey for England 2002Latest Trends.
London: DH; 2003 [www.dh.gov.uk/en/PublicationsAndStatistics/
PublishedSurvey/HealthSurveyForEngland/HealthSurveyResults/
DH_4001334].
3 Lawlor DA, Bedford C, Taylor M, Ebrahim S. Geographical variation in
cardiovascular disease, risk factors, and their control in older women:
British Womens Heart and Health Study. J Epidemiol Community Health
2003;57:13440. doi:10.1136/jech.57.2.134
4 Kanagalingam MG, Forouhi NG, Greer IA, Sattar N. Changes in booking
body mass index over a decade: retrospective analysis from a Glasgow
Maternity Hospital. BJOG 2005;112:14313.
doi:10.1111/j.14710528.2005.00685.x
30
The Obstetrician & Gynaecologist
5 Callaway LK, Prins JB, Chang AM, McIntyre HD. The prevalence and
impact of overweight and obesity in an Australian obstetric population.
Med J Aust 2006;184:569.
6 Manson JE, Bassuk SS. Obesity in the United States: a fresh look at its
high toll. JAMA 2003;289:22930. doi:10.1001/jama.289.2.229
7 Mulders AG, Laven JS, Eijkemans MJ, Hughes EG, Fauser BC. Patient
predictors for outcome of gonadotrophin ovulation induction in women
with normogonadotrophic anovulatory infertility: a meta-analysis. Hum
Reprod Update 2003;9:42949. doi:10.1093/humupd/dmg035
8 Dale PO, Tanbo T, Haug E, Abyholm T. The impact of insulin resistance on
the outcome of ovulation induction with low-dose follicle stimulating
hormone in women with polycystic ovary syndrome. Hum Reprod
1998;13:56770. doi:10.1093/humrep/13.3.567
9 Glueck CJ, Phillips H, Cameron D, Sieve-Smith L, Wang P. Continuing
metformin throughout pregnancy in women with polycystic ovary
syndrome appears to safely reduce first-trimester spontaneous abortion:
a pilot study. Fertil Steril 2001;75:4652.
doi:10.1016/S0015-0282(00)01666-6
10 Glueck CJ, Wang P, Goldenberg N, Sieve L. Pregnancy loss, polycystic
ovary syndrome, thrombophilia, hypofibrinolysis, enoxaparin, metformin.
Clin Appl Thromb Hemost 2004;10:32334.
doi:10.1177/107602960401000404
11 Glueck CJ, Sieve L, Zhu B, Wang P. Plasminogen activator inhibitor
activity, 4G5G polymorphism of the plasminogen activator inhibitor 1
gene, and first-trimester miscarriage in women with polycystic ovary
syndrome. Metabolism 2006;55:34552.
doi:10.1016/j.metabol.2005.09.008
12 Martinez-Frias ML, Frias JP, Bermejo E, Rodriguez-Pinilla E, Prieto L, Frias
JL. Pre-gestational maternal body mass index predicts an increased risk
of congenital malformations in infants of mothers with gestational
diabetes. Diabet Med 2005;22:77581.
doi:10.1111/j.1464-5491.2005.01492.x
13 Anderson JL, Waller DK, Canfield MA, Shaw GM, Watkins ML, Werler MM.
Maternal obesity, gestational diabetes, and central nervous system birth
defects. Epidemiology 2005;16:8792.
doi:10.1097/01.ede.0000147122.97061.bb
14 Wolfe HM, Sokol RJ, Martier SM, Zador IE. Maternal obesity: a potential
source of error in sonographic prenatal diagnosis. Obstet Gynecol
1990;76:33942.
15 Erez-Weiss I, Erez O, Shoham-Vardi I, Holcberg G, Mazor M. The
association between maternal obesity, glucose intolerance and
hypertensive disorders of pregnancy in nondiabetic pregnant women.
Hypertens Pregnancy 2005;24:125136. doi:10.1081/PRG-200059853
16 OBrien TE, Ray JG, Chan WS. Maternal body mass index and the risk of
preeclampsia: a systematic overview. Epidemiology 2003;14:36874.
doi:10.1097/00001648-200305000-00020
17 Sattar N, Clark P, Holmes A, Lean ME, Walker I, Greer IA. Antenatal waist
circumference and hypertension risk. Obstet Gynecol 2001;97:26871.
doi:10.1016/S0029-7844(00)01136-4
18 Cnossen JS, Leeflang MM, de Hann, Mol BW, Van der Post JA, Khan KS,
et al. Accuracy of body mass index in predicting pre eclampsia; bivariate
meta-analysis. BJOG 2007;114:147785.
doi:10.1111/j.1471-0528.2007.01483.x
19 Stewart FM, Freeman DJ, Ramsay JE, Greer IA, Caslake M, Ferrell WR.
Longitudinal assessment of maternal endothelial function and markers of
inflammation and placental function throughout pregnancy in lean and
obese mothers. J Clin Endocrinol Metab 2007;92:969-75.
doi:10.1210/jc.2006-2083
20 Cypryk K, Pertynska-Marczewska M, Szymczak W, Zawodniak-Szalapska
M, Wilczynski J, Lewinski A. [Overweight and obesity as common risk
factors for gestational diabetes mellitus (GDM), perinatal macrosomy in
offspring and type-2 diabetes in mothers.] Przegl Lek 2005;62:3841.
21 National Institute for Health and Clinical Excellence. Diabetes in
Pregnancy: Management of Diabetes and its Complications from Preconception to the Postnatal Period. NICE Clinical Guideline 63. London:
NICE; 2008 [www.nice.org.uk/Guidance/CG63].
22 Villamor E, Cnattingius S. Interpregnancy weight change and risk of
adverse pregnancy outcomes: a population-based study. Lancet
2006;368:116470. doi:10.1016/S0140-6736(06)69473-7
23 Sermer M, Naylor CD, Farine D, Kenshole AB, Ritchie JW, Gare DJ, et al.
The Toronto Tri-Hospital Gestational Diabetes Project. A preliminary
review. Diabetes Care 1998;21 Suppl 2:B3342.
24 Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS.
Effect of treatment of gestational diabetes mellitus on pregnancy
outcomes. N Engl J Med 2005;352:247786.
doi:10.1056/NEJMoa042973
25 Comtois R, Sguin MC, Aris-Jilwan N, Couturier M, Beauregard H.
Comparison of obese and non-obese patients with gestational diabetes.
Int J Obes Relat Metab Disord 1993;17:6058.
26 Langer O, Rodriguez DA, Xenakis EM, McFarland MB, Berkus MD,
Arrendondo F. Intensified versus conventional management of
gestational diabetes. Am J Obstet Gynecol 1994;170:103646.
27 Linn Y, Barkeling B, Rssner S. Natural course of gestational diabetes
mellitus: long term follow up of women in the SPAWN study. BJOG
2002;109:122731. doi:10.1046/j.1471-0528.2002.01373.x
28 Schranz AG, Savona-Ventura C. Long-term significance of gestational
carbohydrate intolerance: a longitudinal study. Exp Clin Endocrinol
Diabetes 2002;110:21922. doi:10.1055/s-2002-33070
29 Rosenberg TJ, Garbers S, Lipkind H, Chiasson MA. Maternal obesity and
diabetes as risk factors for adverse pregnancy outcomes: differences
among 4 racial/ethnic groups. Am J Public Health 2005;95:154551.
doi:10.2105/AJPH.2005.065680
2009 Royal College of Obstetricians and Gynaecologists
TOG11_1_25-31-Stewart
24/12/08
04:20 PM
Page 31
The Obstetrician & Gynaecologist
30 Perlow JH, Morgan MA. Massive maternal obesity and perioperative
caesarean morbidity. Am J Obstet Gynecol 1994;170:5605.
31 Usha Kiran TS, Hemmadis S, Bethel J, Evans J. Outcome of pregnancy in
a woman with an increased body mass index. BJOG 2005;112:76872.
doi:10.1111/j.1471-0528.2004.00546.x
32 Kabiru W, Raynor BD. Obstetric outcomes associated with increase in
BMI category during pregnancy. Am J Obstet Gynecol 2004;191:92832.
doi:10.1016/j.ajog.2004.06.051
33 Weiss JL, Malone FD, Emig D, Ball RH, Nyberg DA, Comstock CH, et al.
Obesity, obstetric complications and caesarean delivery ratesa
population based screening study. Am J Obstet Gynaecol
2004;190:10917. doi:10.1016/j.ajog.2003.09.058
34 Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, et al.
Maternal obesity and pregnancy outcomes; A study of 287 213 women in
London. Int J Obes Relat Disord 2001;25:117582.
doi:10.1038/sj.ijo.0801670
35 Ehrenberg HM, Durnwald CP, Catalano P, Mercer BM. The influence of
obesity and diabetes on the risk of caesarean delivery. Am J Obstet
Gynecol 2004;191:96974. doi:10.1016/j.ajog.2004.06.057
36 Sheiner E, Levy A, Menes TS, Silverberg D, Katz M, Mazor M. Maternal
obesity as an independent risk factor for caesrean section delivery.
Paediatr Perinat Epidemiol 2004;18:196201.
doi:10.1111/j.1365-3016.2004.00557.x
37 Stephansson O, Dickman PW, Johansson A, Cnattingius S. Maternal
weight, pregnancy weight gain, and the risk of antepartum stillbirth. Am J
Obstet Gynecol 2001;184:4639. doi:10.1067/mob.2001.109591
2009 Royal College of Obstetricians and Gynaecologists
2009;11:2531
Review
38 Guerre-Millo M. Adipose tissue and adipokines: for better or
worse. Diabetes Metab 2004;30:1319.
doi:10.1016/ S1262-3636(07)70084-8
39 Hellgren M, Blomback M. Studies on blood coagulation and fibrinolysis in
pregnancy, during delivery and in the puerperium. I. Normal condition.
Gynecol Obstet Invest 1981;12:14154.
40 De Pergola G, Pannacciulli N. Coagulation and fibrinolysis abnormalities
in obesity. J Endocrinol Invest 2002;25:899904.
41 Edwards LE, Hellerstedt WL, Alton IR, Story M, Himes JH. Pregnancy
complications and birth outcomes in obese and normal-weight women:
effects of gestational weight change. Obstet Gynecol 1996;87:38994.
doi:10.1016/0029-7844(95)00446-7
42 Kristensen J, Vestergaard M, Wisborg K, Kesmodel U, Secher NJ. Prepregnancy weight and the risk of stillbirth and neonatal death. BJOG
2005;112:4038. doi:10.1111/j.1471-0528.2005.00437.x
43 Galtier-Dereure F, Montpeyroux F, Boulot P, Bringer J, Jaffiol C. Weight
excess before pregnancy: complications and cost. Int J Obes Relat
Metab Disord 1995;19:4438.
44 Barker DJ, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson
JS. Fetal nutrition and cardiovascular disease in adult life. Lancet
1993;341:938-41. doi:10.1016/0140-6736(93)91224-A
45 Forsn T, Eriksson JG, Tuomilehto J, Teramo K, Osmond C, Barker DJ.
Mothers weight in pregnancy and coronary heart disease in a cohort of
Finnish men: follow up study. BMJ 1997;315:83740.
46 Galtier-Dereure F, Boegner C, Bringer J. Obesity and pregnancy:
complications and cost. Am J Clin Nutr 2000;71 Suppl 5:1242S8S.
31
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 101 Questions To Ask About Your LifeDocument18 pages101 Questions To Ask About Your LifeKika Spacey RatmNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- MCQ'S FOR Obstetrics and GynaecologyDocument330 pagesMCQ'S FOR Obstetrics and Gynaecologywhoosh200887% (108)
- Mcqs For Mrcog Part 1 - Richard de CourcyDocument118 pagesMcqs For Mrcog Part 1 - Richard de Courcyprincessmeleana6499No ratings yet
- 29 - Abnormal Uterine ActionDocument31 pages29 - Abnormal Uterine Actiondr_asaleh94% (18)
- Pathophysiology of Incomplete Abortion: Risk Factors and ManagementDocument3 pagesPathophysiology of Incomplete Abortion: Risk Factors and ManagementClaire Nimor Ventulan50% (4)
- Doh Health Programs (Maternal)Document47 pagesDoh Health Programs (Maternal)Wilma Nierva Beralde100% (1)
- Unit I - Introduction-to-Midwifery-Obstetrical-NursingDocument43 pagesUnit I - Introduction-to-Midwifery-Obstetrical-NursingN. Siva100% (8)
- Legal MandatesDocument39 pagesLegal MandatesMarkGuirhem100% (1)
- C-S & VbacDocument54 pagesC-S & VbacDagnachew kasayeNo ratings yet
- FSRH Ukmec Full Book 2017Document178 pagesFSRH Ukmec Full Book 2017A KNo ratings yet
- 10 Things Every Physician Needs To Know About BurnoutDocument5 pages10 Things Every Physician Needs To Know About Burnoutprincessmeleana6499No ratings yet
- AsthmaDocument5 pagesAsthmaprincessmeleana6499No ratings yet
- OHSSDocument5 pagesOHSSprincessmeleana6499No ratings yet
- Tog 12091Document4 pagesTog 12091princessmeleana6499No ratings yet
- BoulderIng For BeginnersDocument42 pagesBoulderIng For BeginnersmeersonNo ratings yet
- Rules of The Road Eng PDFDocument264 pagesRules of The Road Eng PDFprincessmeleana6499No ratings yet
- Mirena Jaydess Differentiation Booklet Sept15Document12 pagesMirena Jaydess Differentiation Booklet Sept15princessmeleana6499No ratings yet
- LR ProtocolDocument159 pagesLR ProtocolJeevan VelanNo ratings yet
- Trial LabourDocument3 pagesTrial Laboursujinaranamagar18No ratings yet
- Partograph: (Use This Form For Monitoring Active Labour)Document1 pagePartograph: (Use This Form For Monitoring Active Labour)Omar Khalif Amad PendatunNo ratings yet
- Course Information For Current Semester/Term: Maklumat Kursus Untuk Semester/Penggal SemasaDocument5 pagesCourse Information For Current Semester/Term: Maklumat Kursus Untuk Semester/Penggal SemasaNurul IrhamnaNo ratings yet
- Gestational Trophoblastic DiseaseDocument22 pagesGestational Trophoblastic DiseaseBright KumwendaNo ratings yet
- The Impact of Teenage Pregnancy On Maternal, Fetal and Neonatal OutcomesDocument8 pagesThe Impact of Teenage Pregnancy On Maternal, Fetal and Neonatal Outcomesjacque najeraNo ratings yet
- Pengaruh Pemberian Aromaterapi Lemon (Citrus Lemon) Terhadap Mual Muntah Pada Ibu Hamil Trimester IDocument7 pagesPengaruh Pemberian Aromaterapi Lemon (Citrus Lemon) Terhadap Mual Muntah Pada Ibu Hamil Trimester IMei SuriyatiNo ratings yet
- Pregnant Teen Case ManagementDocument22 pagesPregnant Teen Case Managementapi-171781702100% (1)
- Obstetrics and Gynecology Module 1 Hevinkumar PatelDocument12 pagesObstetrics and Gynecology Module 1 Hevinkumar PatelhevinpatelNo ratings yet
- Klasifikasi Plasenta PDFDocument9 pagesKlasifikasi Plasenta PDFTedi MulyanaNo ratings yet
- Preterm Rupture of MembranesDocument13 pagesPreterm Rupture of Membranesjoyrena ochondraNo ratings yet
- Association of Third Trimester Body Mass Index and Pregnancy Weight Gain in Obese Pregnant Women To Umbilical Artery Atherosclerotic Markers and Fetal OutcomesDocument7 pagesAssociation of Third Trimester Body Mass Index and Pregnancy Weight Gain in Obese Pregnant Women To Umbilical Artery Atherosclerotic Markers and Fetal OutcomesMahida El shafiNo ratings yet
- Sample PRC RequirementsDocument4 pagesSample PRC RequirementsRodney Beltran SubaranNo ratings yet
- Water Birth: Benefits and SafetyDocument21 pagesWater Birth: Benefits and SafetyudupisonyNo ratings yet
- Clinical Embryology (CH 1-7) (KLM) : TrisomyDocument4 pagesClinical Embryology (CH 1-7) (KLM) : Trisomykamran_zarrarNo ratings yet
- Prophylactic Cervical Cerclage (Modified Shirodkar Operation) For Twin and Triplet Pregnancies After Fertility TreatmentDocument8 pagesProphylactic Cervical Cerclage (Modified Shirodkar Operation) For Twin and Triplet Pregnancies After Fertility TreatmentAiraNo ratings yet
- Maternal and Child HealthDocument15 pagesMaternal and Child Healthgamal attamNo ratings yet
- Molar PregnancyDocument15 pagesMolar Pregnancyapi-3705046No ratings yet
- Retained PlacentaDocument2 pagesRetained PlacentaAmiraah MasriNo ratings yet
- Jurnal Kukerta Terintegrasi AbdimasDocument5 pagesJurnal Kukerta Terintegrasi AbdimasholaNo ratings yet
- Keep Calm and Wait for Labor: Why Going to Full Term Is Best for Mom and BabyDocument1 pageKeep Calm and Wait for Labor: Why Going to Full Term Is Best for Mom and BabyGururaj kulkarniNo ratings yet
- PPH Guideline 2015Document87 pagesPPH Guideline 2015Diksha chaudharyNo ratings yet
- Tabel JurnalDocument31 pagesTabel JurnalAlfNo ratings yet