Professional Documents
Culture Documents
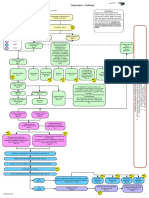
Medicamentosa MDD
Uploaded by
mieraelOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medicamentosa MDD
Uploaded by
mieraelCopyright:
Available Formats
Various types of antidepressants are available:
A. Selective Serotonin Reuptake Inhibitors (SSRIs)
B. Serotonin norepinephrine reuptake inhibitors (SNRIs)
C. Monoamine oxidase inhibitors (MAOIs)
D. 5-HT2 Antagonists
E. Bupropion
A. SSRSIs
a. Agents: Fluoxetine (Prozac), paroxetine, sertraline, fluvoxamine,
Citalopram, & Escitalopram (s-citalopram)
b. Clinical uses:
i. Major Depression: the primary indication Obsessive-compulsive
disorder (OCD) (fluvoxamine, clomipramine)
ii. Panic disorder
iii. Generalized anxiety disorder
iv. Posttraumatic stress disorder (Sertraline and paroxetine)
v. Social anxiety disorder (SAD): fluvoxamine, venlafaxine
vi. Premenstrual dysphoric disorder (fluxetine & sertraline)
vii. Bulimia nervosa (only fluoxetine)
viii. Premature ejaculation
c. Repeated treatment leads to gradual down-regulation
d. no affinity for cholinergic, -adrenergic or histamine receptors and do
not interfere with cardiac conduction
e. adv. Effect:
i. GIT: nausea, GIT upset, diarrhea.
ii. Sexual dysfunction: loss of libido, delayed orgasm, or
diminished arousal.
iii. CNS: Sleep disturbances. For this reason, fluoxetine is usually
administered in the morning after breakfast
iv. Weight gain particularly paroxetine
v. SSRIs have also been associated with extrapyramidal side
effects, especially those with Parkinsons disease
B. SNRIs
a. Agents: venlafaxine, desvenlafaxine, and duloxetine & milnacipran*
b. All SNRIs bind the serotonin (SERT) and norepinephrine (NET)
transporters
c. At dosages <150 mg/day, venlafaxine is a potent inhibitor of serotonin
reuptake and, at medium to higher doses, is an inhibitor of
norepinephrine re-uptake
d. Duloxetine inhibits serotonin and norepinephrine reuptake at all doses
e. Clinical uses:
i. Depression: in patients in whom SSRIs are ineffective
ii. chronic joint and muscle pain: duloxetine
iii. Fibromyalgia: milnacipran
f.
SNRIs have many of the serotonergic adverse effects associated with
SSRIs
g. In addition, SNRIs may also have noradrenergic effects, including
increased blood pressure and heart rate, and CNS activation, such as
insomnia, anxiety, and agitation
C. TCA
a. The TCAs were the dominant class of antidepressants until the
introduction of SSRIs in the 1980s and 1990s
b. Agents: imipramine (the prototype drug), amitriptyline, clomipramine,
doxepin , trimipramine, desipramine, nortriptyline, and protriptyline
c. inhibition 5HT and NE reuptake
d. TCAs also block serotonergic, -adrenergic, histaminic, and muscarinic
receptors
e. Clinical uses:
i. Depression: that is unresponsive to more commonly used
antidepressants )SSRIs or SNRIs)
ii. Panic disorder
iii. Control bed-wetting in children (older than 6 years) by causing
contraction of the internal sphincter of the bladder (Imipramine) 1
iv. Treatment of migraine headache and chronic pain syndromes for
which the cause of the pain is unclear (Amitriptyline)
f. Adverse effects:
i. Antimuscarinic SEs: dry mouth ,constipation, urinary retention,
blurred vision, and confusion
ii. Life-threatening arrhythmias: The TCAs are class 1A
antiarrhythmic agents
iii. Sedation (H1 antagonism)
iv. weight gain
v. Sexual dysfunction
D. MAOIs
a. Agents: selegline, phenelzine, and tranylcypromine
b. Adverse effects:
i. Orthostatic hypotension, weight gain, edema, and sexual
dysfunction are common during MAOI therapy
ii. Sexual SEs: highest rates are associated with the irreversible
nonselective MAOIs (phenelzine and tranylcypromine)
iii. Hepatotoxicity is likely to occur with isocarboxazid or phenelzine
E. 5-HT2 Antagonist
a. Agents: Nefazodone, Trazodone, mirtazapine and mianserin (not
marketed in the U.S.)
b. Inhibition of 5-HT2A receptors in both animal and human studies is
associated with substantial antianxiety, antipsychotic, and
antidepressant effects
c. Clinical uses:
i. Depression: Mirtazapine can be advantagous in patients with
depression having sleep difficulties
d. Adverse effects:
i. Sedation (trazodone & mirtazapine)
ii. weight gain (mirtazapine)
iii. Nefazodone has been associated with hepatotoxicity, including
rare fatalities and cases of hepatic failure requiring
transplantation
F. Buproprion
a. It acts as a weak dopamine and norepinephrine reuptake inhibitor to
alleviate the symptoms of depression
b. Bupropion has virtually no direct effects on the serotonin system
c. Unlike the SSRIs, bupropion does not cause sexual side effects
d. It does not block muscarinic, histaminergic, or adrenergic receptors
e. Clinical uses:
i. Depression
f. Bupropion is approved as a treatment for smoking cessation
g. The mechanism by which bupropion is helpful in this application is
unknown, but the drug may mimic nicotine's effects on dopamine and
norepinephrine and may antagonize nicotinic receptors
h. Side Effects
i. Bupropion is occasionally associated with CNS stimulations
(agitation, insomnia, and anorexia)
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Antidepressant ChartDocument7 pagesAntidepressant Chartinher1tance100% (4)
- Psychopharmacology 2 AntidepressantsDocument7 pagesPsychopharmacology 2 AntidepressantsBea Samonte100% (2)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Psychotropic Drugs: By: Rheajane Aguilar-RosalesDocument77 pagesPsychotropic Drugs: By: Rheajane Aguilar-Rosalesjean samson100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Psychotropic MedicationDocument28 pagesPsychotropic Medicationrmconvidhya sri2015No ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- AntidepressantsDocument59 pagesAntidepressantsanon_189054600100% (2)
- Depression Care PathwayDocument267 pagesDepression Care PathwaydwiNo ratings yet
- Drugs For Psyciatric DisordersDocument19 pagesDrugs For Psyciatric Disordersapi-36993610% (1)
- Pharmacological Classification of DrugsDocument68 pagesPharmacological Classification of Drugssanjeev khanalNo ratings yet
- Pharmacology and Toxicology of Antidepressants and AntipsychoticsDocument50 pagesPharmacology and Toxicology of Antidepressants and AntipsychoticsPintu Bhushan MitraNo ratings yet
- Rang Dale S Pharmacology Self Assessment Questions 7th PDFDocument62 pagesRang Dale S Pharmacology Self Assessment Questions 7th PDFJohita Paz100% (8)
- Algorithm For DX TBDocument6 pagesAlgorithm For DX TBmieraelNo ratings yet
- Medicamentosa MDDDocument3 pagesMedicamentosa MDDmieraelNo ratings yet
- Prothrombin Time Dan Activated Prothrombin Time 1Document9 pagesProthrombin Time Dan Activated Prothrombin Time 1mieraelNo ratings yet
- Prothrombin Time Dan Activated Prothrombin TimeDocument9 pagesProthrombin Time Dan Activated Prothrombin TimemieraelNo ratings yet
- Klasifikasi Patofisiologis TrombositopeniaDocument1 pageKlasifikasi Patofisiologis TrombositopeniamieraelNo ratings yet
- Jaw Thrust Head Tilt LO 7Document2 pagesJaw Thrust Head Tilt LO 7mieraelNo ratings yet
- Emergency PDFDocument11 pagesEmergency PDFmieraelNo ratings yet
- Pamflet Katarak KomunitasDocument1 pagePamflet Katarak KomunitasmieraelNo ratings yet
- Serotonin SyndromeDocument8 pagesSerotonin SyndromeJuan Carlos AlfaroNo ratings yet
- 2008 Curcumin AD - Hong Kong StudyDocument22 pages2008 Curcumin AD - Hong Kong StudysandyedamanaNo ratings yet
- 1 Mood Disorders Whole Document 1Document10 pages1 Mood Disorders Whole Document 1Myles Zen Dieta EaNo ratings yet
- Bystritsky Anxiety Treatment Overview Pharm Therap 2013Document14 pagesBystritsky Anxiety Treatment Overview Pharm Therap 2013Amanuel MaruNo ratings yet
- Pharmacological Strategies in The Management of Alzheimer'S DiseaseDocument46 pagesPharmacological Strategies in The Management of Alzheimer'S DiseaseKreshnik IdrizajNo ratings yet
- Augmentation Strategies in Obsessive Compulsive DisorderDocument18 pagesAugmentation Strategies in Obsessive Compulsive DisorderLucijano Andreas SoftićNo ratings yet
- Problems Currently Available AntidepressantsDocument11 pagesProblems Currently Available AntidepressantsArfa NisaNo ratings yet
- Medication dosing and notes for anxiety and depressionDocument2 pagesMedication dosing and notes for anxiety and depressionMaryNguyenNo ratings yet
- Jetlax's CNS Pharmacology Cheat Sheet For The Philippines v6.0 at Bit - Ly - CNSPcol - See Bit - Ly - CNSHandouts For 5.0 CorrectionsDocument61 pagesJetlax's CNS Pharmacology Cheat Sheet For The Philippines v6.0 at Bit - Ly - CNSPcol - See Bit - Ly - CNSHandouts For 5.0 CorrectionsShalimar BasmanNo ratings yet
- Psychotropic DrugsDocument60 pagesPsychotropic DrugsLaTasha Lindemann RNNo ratings yet
- الادوية فى مصر مرتبة بالاسم العلمى وبالتصنيفDocument112 pagesالادوية فى مصر مرتبة بالاسم العلمى وبالتصنيفmahgad83% (24)
- 2ND and 3RD Drug StudyDocument16 pages2ND and 3RD Drug Study황춘히No ratings yet
- PENGGOLONGAN OBAT PSIKOTROPIK DAN SEDIAAN OBAT ANTI-PSIKOSISDocument18 pagesPENGGOLONGAN OBAT PSIKOTROPIK DAN SEDIAAN OBAT ANTI-PSIKOSISMirzanNo ratings yet
- Treatment Options For Hyperemesis GravidarumDocument11 pagesTreatment Options For Hyperemesis GravidarumJC QuinNo ratings yet
- MRTZ Bestel GB PDFDocument8 pagesMRTZ Bestel GB PDFmilanmcaNo ratings yet
- Types of Antidepressants and How They WorkDocument1 pageTypes of Antidepressants and How They WorkSadiq AchakzaiNo ratings yet
- Diagnosing Constipation, Obstipation, & Megacolon in CatsDocument6 pagesDiagnosing Constipation, Obstipation, & Megacolon in CatsPratiwi Retno SetyaningrumNo ratings yet
- Antidepresive Sedative ActivatoareDocument2 pagesAntidepresive Sedative ActivatoareDrima EdiNo ratings yet
- Quiz 5Document28 pagesQuiz 5YNo ratings yet
- Psilocybin For Depression and Anxiety Associated With Life-Threatening IllnessesDocument2 pagesPsilocybin For Depression and Anxiety Associated With Life-Threatening IllnessesJosé Carlos Solís SuárezNo ratings yet