Professional Documents
Culture Documents
Celex 52015XC0321 (02) en
Uploaded by
tito1628Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Celex 52015XC0321 (02) en
Uploaded by
tito1628Copyright:
Available Formats
C 95/10
EN
Official Journal of the European Union
21.3.2015
Guidelines
of 19 March 2015
on the formalised risk assessment for ascertaining the appropriate good manufacturing practice for
excipients of medicinal products for human use
(Text with EEA relevance)
(2015/C 95/02)
Introduction
These guidelines are based on the fifth paragraph of Article 47 of Directive 2001/83/EC (1).
According to the second paragraph of Article 46(f) of Directive 2001/83/EC, the manufacturing authorisation holder is
required to ensure that the excipients are suitable for use in medicinal products by ascertaining what the appropriate
good manufacturing practice (GMP) is. The appropriate GMP for excipients of medicinal products for human use shall
be ascertained on the basis of a formalised risk assessment in accordance with these guidelines. The risk assessment
shall take into account requirements under other appropriate quality systems as well as the source and intended use of
the excipients and previous instances of quality defects. The manufacturing authorisation holder shall ensure that the
appropriate GMP ascertained is applied. The manufacturing authorisation holder shall document the measures taken.
The excipient risk assessment/risk management procedure should be incorporated in the pharmaceutical quality system
of the manufacturing authorisation holder.
Manufacturing authorisation holders should have the risk assessment/management documentation for appropriate GMP
for excipients available on site for review by GMP inspectors. Consideration should be given to sharing relevant informa
tion from the risk assessment with the excipient manufacturer to facilitate continuous improvement.
A risk assessment as set out in these guidelines should be carried out for excipients for authorised medicinal products
for human use by 21 March 2016.
CHAPTER 1 SCOPE
1.1. These guidelines apply to the risk assessment for ascertaining the appropriate GMP for excipients for medicinal
products for human use. According to Article 1(3b) of Directive 2001/83/EC, an excipient is any constituent of
a medicinal product other than the active substance and the packaging material.
1.2. These guidelines do not cover substances added to stabilise active substances that cannot exist on their own.
CHAPTER 2 DETERMINATION OF APPROPRIATE GMP BASED ON TYPE AND USE OF EXCIPIENT
2.1. In EudraLex Volume 4, Guidelines for Good Manufacturing Practice, Medicinal Products for Human and Veterinary
Use, Part III: GMP related documents, ICH guideline Q9 on Quality Risk Management (ICH Q9), principles and
examples of tools for quality risk management that can be applied to different aspects of pharmaceutical quality,
including excipients, can be found.
2.2. These quality risk management principles should be used to assess the risks presented to the quality, safety and
function of each excipient and to classify the excipient in question, e.g. as low risk, medium risk or high risk.
Quality risk management tools such as those listed in EudraLex Volume 4, Part III, ICH Q9 (e.g. hazard analysis
and critical control points HACCP) should be used for this purpose.
2.3. For each excipient from each manufacturer used, the manufacturing authorisation holder should identify the risks
presented to the quality, safety and function of each excipient from its source be that animal, mineral, vegetable,
synthetic, etc. through to its incorporation in the finished pharmaceutical dose form. Areas for consideration
should include, but are not limited to:
(i) transmissible spongiform encephalopathy;
(ii) potential for viral contamination;
(1) Directive 2001/83/EC of the European Parliament and of the Council of 6 November 2001 on the Community code relating to medicinal
products for human use (OJ L 311, 28.11.2001, p. 67).
21.3.2015
EN
Official Journal of the European Union
C 95/11
(iii) potential for microbiological or endotoxin/pyrogen contamination;
(iv) potential, in general, for any impurity originating from the raw materials, e.g. aflatoxins or pesticides, or
generated as part of the process and carried over, e.g. residual solvents and catalysts;
(v) sterility assurance for excipients claimed to be sterile;
(vi) potential for any impurities carried over from other processes, in absence of dedicated equipment and/or
facilities;
(vii) environmental control and storage/transportation conditions including cold chain management, if
appropriate;
(viii) supply chain complexity;
(ix) stability of excipient;
(x) packaging integrity evidence.
2.4. Additionally, with respect to the use and function of each excipient, the manufacturing authorisation holder should
consider:
(i) the pharmaceutical form and use of the medicinal product containing the excipient;
(ii) the function of the excipient in the formulation, e.g. lubricant in a tablet product or preservative material in
a liquid formulation, etc.;
(iii) the proportion of the excipient in the medicinal product composition;
(iv) daily patient intake of the excipient;
(v) any known quality defects/fraudulent adulterations, both globally and at a local company level related to the
excipient;
(vi) whether the excipient is a composite;
(vii) known or potential impact on the critical quality attributes of the medicinal product;
(viii) other factors as identified or known to be relevant to assuring patient safety.
2.5. Having established and documented the risk profile of the excipient, the manufacturing authorisation holder
should establish and document the elements of EudraLex Volume 4 that he believes are needed to be in place in
order to control and maintain the quality of the excipient, e.g. Annex 1 or/and Annex 2; Part II: Basic Require
ments for Active Substances used as Starting Materials.
2.6. These elements will vary depending on the source, the supply chain and the subsequent use of the excipient, but as
a minimum the following high level GMP elements should be considered by the manufacturing authorisation
holder:
(i) establishment and implementation of an effective pharmaceutical quality system;
(ii) sufficient competent and appropriately qualified personnel;
(iii) defined job descriptions for managerial and supervisory staff responsible for manufacturing and quality
activities;
(iv) training programmes for all staff involved in manufacturing and quality activities;
(v) training programmes related to health, hygiene and clothing as identified as necessary to the intended
operations;
(vi) provision and maintenance of premises and equipment appropriate to the intended operations;
C 95/12
Official Journal of the European Union
EN
21.3.2015
(vii) documentation system(s) covering all processes and specifications for the various manufacturing and quality
operations;
(viii) systems for coding and identifying starting materials, intermediates and excipients to allow full traceability;
(ix) qualification program of suppliers;
(x) system for quality control of the excipient and a responsible person independent from production to release
the batches;
(xi) retention of records for incoming materials and excipients and retention of samples of excipients for the peri
ods required by EudraLex Volume 4, Part II;
(xii) systems to ensure that any activity contracted out is subject to a written contract;
(xiii) maintenance of an effective system whereby complaints are reviewed and excipients may be recalled;
(xiv) change management and deviation management system;
(xv) self-inspection program;
(xvi) environmental control and storage conditions.
CHAPTER 3 DETERMINATION OF EXCIPIENT MANUFACTURERS RISK PROFILE
3.1. After determination of the appropriate GMP, a gap analysis of the required GMP against the activities and capabili
ties of the excipient manufacturer should be performed.
3.2. Data/evidence to support the gap analysis should be obtained through audit or from information received from the
excipient manufacturer.
3.3. Certification of quality systems and/or GMP held by the excipient manufacturer and the standards against which
these have been granted should be considered as such certification may fulfil the requirements.
3.4. Any gaps identified between the required GMP and the activities and capabilities of the excipient manufacturer should
be documented. Furthermore, the manufacturing authorisation holder should perform a further risk assessment to
determine the risk profile, e.g. low risk, medium risk or high risk, for that excipient manufacturer. EudraLex Volume 4,
Part III, ICH Q9 should be used for that purpose. Quality risk management tools such as those listed there HACCP
etc. should be used for this.
3.5. The manufacturing authorisation holder should have a series of strategies ranging from acceptance through control
to unacceptable for the different risk profiles and based on these a control strategy, e.g. audit, document retrieval
and testing, should be established.
CHAPTER 4 CONFIRMATION OF APPLICATION OF APPROPRIATE GMP
4.1. Once the appropriate GMP for the excipient and the risk profile of the excipient manufacturer have been defined,
ongoing risk review should be performed through mechanisms such as:
(i) number of defects connected to batches of excipient received;
(ii) type/severity of such defects;
(iii) monitoring and trend analysis of excipient quality;
(iv) loss of relevant quality system and/or GMP certification by excipient manufacturer;
(v) observation of trends in drug product quality attributes; this will depend on the nature and role of excipient;
(vi) observed organisational, procedural or technical/process changes at the excipient manufacturer;
21.3.2015
EN
Official Journal of the European Union
(vii) audit/re-audit of excipient manufacturer;
(viii) questionnaires.
Based on the outcome of the risk review, the established control strategy should be reviewed and revised if needed.
C 95/13
You might also like
- Book For PharmaceuticalsDocument63 pagesBook For PharmaceuticalsPentesh NingaramainaNo ratings yet
- Appendix 2 Compulsory Exercises Aerial Hoop 2018 EngDocument28 pagesAppendix 2 Compulsory Exercises Aerial Hoop 2018 Engtito1628100% (1)
- Alberto Villoldo Book PDFDocument120 pagesAlberto Villoldo Book PDFtito1628100% (3)
- Aerial Yoga Manual 2018 Third Edition ADocument156 pagesAerial Yoga Manual 2018 Third Edition Atito1628100% (8)
- Analisis de RiesgoDocument1 pageAnalisis de Riesgotito1628No ratings yet
- Rings One Manual Ebook PDFDocument87 pagesRings One Manual Ebook PDFAarif Akbari67% (3)
- Skinfold Sume Referencee Valuese For Tope AthletesDocument7 pagesSkinfold Sume Referencee Valuese For Tope Athletestito1628No ratings yet
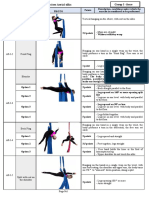
- Aerial Silks Exercises Group I Force MovesDocument23 pagesAerial Silks Exercises Group I Force Movestito1628100% (6)
- Aerial Yoga Manual 2018 Third Edition ADocument156 pagesAerial Yoga Manual 2018 Third Edition Atito1628100% (8)
- The Aerial Sling Manual: Prev Iew Prev IewDocument13 pagesThe Aerial Sling Manual: Prev Iew Prev Iewtito1628100% (1)
- Shamal 1206Document134 pagesShamal 1206tito1628No ratings yet
- Tutorial AnillasDocument40 pagesTutorial Anillastito1628No ratings yet
- The Aerial Sling Manual: Prev Iew Prev IewDocument13 pagesThe Aerial Sling Manual: Prev Iew Prev Iewtito1628100% (1)
- FMEA - A Guide For Continuous ImprovementDocument36 pagesFMEA - A Guide For Continuous Improvementvipin_chaudhary100% (1)
- HACCP en Drogas AnticancerDocument7 pagesHACCP en Drogas Anticancertito1628No ratings yet
- FDA Guidance - Submission of CMC Info For RDDPs and MAbsDocument30 pagesFDA Guidance - Submission of CMC Info For RDDPs and MAbsNelson Alejandro FierroNo ratings yet
- Business System ReviewDocument12 pagesBusiness System Reviewtito1628No ratings yet
- Handouts - GMP Workshop 27-28 Feb 2014Document76 pagesHandouts - GMP Workshop 27-28 Feb 2014tito1628No ratings yet
- Workshop 2 Spanish FDA RequirementsDocument29 pagesWorkshop 2 Spanish FDA Requirementstito1628No ratings yet
- S3 Guo Sherry Temperature ExcursionDocument51 pagesS3 Guo Sherry Temperature Excursiondian fitri anandaNo ratings yet
- Lynne EnsorDocument32 pagesLynne Ensortito1628No ratings yet
- EffectivenessofTrainingArthur Etal PDFDocument12 pagesEffectivenessofTrainingArthur Etal PDFIrene KangNo ratings yet
- CCP - en European CTD PDFDocument7 pagesCCP - en European CTD PDFtito1628No ratings yet
- CCP - en European CTD PDFDocument7 pagesCCP - en European CTD PDFtito1628No ratings yet
- A Historical View of Human Resource ManagementDocument12 pagesA Historical View of Human Resource Managementtito1628No ratings yet
- The Formalized Risk Assessment For Excipients - GenialDocument22 pagesThe Formalized Risk Assessment For Excipients - Genialtito1628No ratings yet
- 1-5 Equipment QualificationDocument47 pages1-5 Equipment QualificationSandip NajanNo ratings yet
- Optimized Interval Training ProtocolDocument6 pagesOptimized Interval Training Protocoltito1628No ratings yet
- Online OgilvieDocument7 pagesOnline Ogilvietito1628No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Зріз 3-ж курс 2 варіант ГусєваDocument4 pagesЗріз 3-ж курс 2 варіант ГусєваSasha MayNo ratings yet
- Cliche Swot Analysis CyprusDocument3 pagesCliche Swot Analysis CyprusVivi CarouzouNo ratings yet
- 5 Example of GMO PlantsDocument5 pages5 Example of GMO PlantsEmmanuel RicablancaNo ratings yet
- Menu Table D'hoteDocument5 pagesMenu Table D'hoteWinafriliaNo ratings yet
- Indian Wine IndustryDocument67 pagesIndian Wine IndustryVinay Singh100% (2)
- 002 Geography of Home Writings On Where We LiveDocument45 pages002 Geography of Home Writings On Where We LivearhitheoNo ratings yet
- A2-KET-Test 1Document18 pagesA2-KET-Test 1Ngọc Hà100% (1)
- Edible and Poisonous Plants of The Caribbean RegionDocument112 pagesEdible and Poisonous Plants of The Caribbean Regioncesar3126No ratings yet
- Bone Health (CN)Document8 pagesBone Health (CN)Nikken, Inc.No ratings yet
- Ground and Processed SpicesDocument11 pagesGround and Processed SpicesAnas MKNo ratings yet
- Resume of Dotnet DeveloperDocument4 pagesResume of Dotnet DeveloperrsraomcaNo ratings yet
- Test Cut 6Document6 pagesTest Cut 6Ramona FlowersNo ratings yet
- 15 The Plant WorldDocument5 pages15 The Plant WorldnishantNo ratings yet
- Conclusions & InferencesDocument69 pagesConclusions & InferencesPaulina ReyesNo ratings yet
- FOOD PROCESSING NC II (Study Guide)Document4 pagesFOOD PROCESSING NC II (Study Guide)Aldz Forbes Lpt100% (1)
- A 2 Szintfelmero AngolDocument2 pagesA 2 Szintfelmero AngolJanka SzöőrNo ratings yet
- IMPACT OF COVID 19 ON BAKERIES AROUND GM MILLS, COIMBATORE (Final)Document13 pagesIMPACT OF COVID 19 ON BAKERIES AROUND GM MILLS, COIMBATORE (Final)dprabha99No ratings yet
- Assignment-Sm Swot Analysis On Robin HoodDocument2 pagesAssignment-Sm Swot Analysis On Robin HoodzaraNo ratings yet
- I Got Lazxy, But There Is A Lot To Go OverDocument23 pagesI Got Lazxy, But There Is A Lot To Go OverGwainNo ratings yet
- Screening and CoachingDocument39 pagesScreening and CoachingDoyoung ChantelleNo ratings yet
- Source Book: Environmental Horticulture & Landscape IndustryDocument5 pagesSource Book: Environmental Horticulture & Landscape IndustryGic LandscapeNo ratings yet
- EDC Catering SOPDocument5 pagesEDC Catering SOPakenNo ratings yet
- SABER PRO. PART 5B (II) - Revisión Del IntentoDocument3 pagesSABER PRO. PART 5B (II) - Revisión Del IntentoOscar Leandro Gaitan VasquezNo ratings yet
- True or False Easter TraditionsDocument1 pageTrue or False Easter TraditionsSnezana DanilovicNo ratings yet
- Kimamon National High School Procurement PlanDocument3 pagesKimamon National High School Procurement Planispa44No ratings yet
- 2004 113 1030 Bernard Weiss, Sherlita Amler and Robert W. AmlerDocument9 pages2004 113 1030 Bernard Weiss, Sherlita Amler and Robert W. AmlerPlissken EderNo ratings yet
- Practicle 1, Part 1 WorksheetDocument7 pagesPracticle 1, Part 1 WorksheetHazim HsNo ratings yet
- Setting Up A Church NurseryDocument3 pagesSetting Up A Church NurseryPastor JeanneNo ratings yet
- Mushoku+Tensei 09+ +Youth+Period+ + (Sylphiette) (v2)Document254 pagesMushoku+Tensei 09+ +Youth+Period+ + (Sylphiette) (v2)aimoroida100% (1)
- A Woman ScornedDocument36 pagesA Woman ScornedmamolokocandykidNo ratings yet