Professional Documents
Culture Documents
Oral Corticosteroids
Uploaded by
loraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oral Corticosteroids
Uploaded by
loraCopyright:
Available Formats
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Introduction
Many ocular and systemic conditions recognized by optometrists can be treated by the
judicious use of corticosteroids, commonly known as steroids. This course serves to educate
the reader about the mechanisms of steroid action, potential ocular side effects and systemic
effects. It also provides information on indications and contraindications for use of steroids in
optometric practice.
Mechanism of Action of Steroids
In the mid 1800s, Addison and Brown-Sequard studied the role of adrenal glands in regulating
body function. Later, in the early 1900s, several hormones termed glucocorticoids and
mineralocorticoids were isolated from the cortex of the adrenal gland. The most important
glucocorticoid derived from the adrenal gland is cortisol (sometimes called hydroxycortisone).
The mid-1900s brought the discovery of the interesting link between the adrenal glands, the
pituitary gland (responsible for secreting adrenocorticotropic hormone, or ACTH, which
stimulates adrenal cortex steroid production), and the hypothalamus (responsible for secreting
corticotropin-releasing factor, or CRF, which stimulates pituitary ACTH production). The
hypothalamus secretes more CRF in response to neural excitatory stimuli and reduced plasma
corticosteroid concentration. This cascades to increasing pituitary ACTH production that
ultimately increases adrenal cortex steroid production. This interdependent feedback
mechanism is termed the H-P-A axis (Figure 1).
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 1 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Figure 1. H-P-A (Hypothalamus-Pituitary-Adrenal Cortex) Axis
What is the benefit of this H-P-A axis? Simply put, it controls adaptation by the body to
changing internal and external stimuli regulating corticosteroid secretion. The corticosteroids
affect the body in many complex ways, some of which are shown in Table 1.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 2 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
EFFECT MECHANISM
Anti-inflammatory Reduce T cells and B cells
responsible for inflammatory
response
Inhibit macrophage and neutrophil
migration
Inhibit prostaglandin synthesis by
inhibition of phospholipase A(Z)
Hyperglycemia Increase liver glycogen storage
Inhibit glucose oxidation
Increase insulin resistance by cell
Alteration of Lipid distribution Increase fat deposits on face/neck
(Cushingoid)
Decrease fat from extremities
Increase lipid production from
protein
Increase in low-density lipoproteins
(LDLs)
-decrease in high-density
lipoproteins (HDLs)
Blood cell constituents Iincrease red blood cell and
polymorphonuclear leukocyte
number
Decrease eosinophils, basophils, and
monocytes
Central nervous system Various mood changes (unknown
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 3 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
mechanism)
Allergic Response Rreduce symptoms (unknown
mechanism)
Table 1. Some corticosteroid effects on the body
In a normal individual, the adrenal glands normally secrete about 25mg of cortisol
(hydrocortisone) and 5 mg corticosterone per day. Only about 5% of these steroids are
biologically active, the remainder being bound to plasma protein. It is remarkable that such a
small amount of active steroid can so dramatically modulate numerous metabolic activities.
Because the natural steroids are so potent and affect so many systems, the use of synthetic
steroids in clinical practice should be done conservatively.
The main use of steroids in practice is to reduce inflammatory action. Figure 2 displays the
cellular synthesis of prostaglandins and leukotrienes from arachidonic acid. This synthesis is
termed the inflammatory pathway, and is the main cascade to the inflammatory response:
Figure 2. The inflammatory pathway and its inhibition by steroids and non-steroidal anti-
inflammatory drugs.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 4 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
The synthesis products of prostaglandins (particularly PGE(1), PGE(Z), and PGF(Z-ALPHA)) and
leukotrienes have been implicated in inflammatory responses such as vascular dilation and
polymorphonuclear leukocyte migration, but their exact mechanisms of action are still not well
understood. Steroids (specifically glucocorticosteroids such as cortisol or prednisone) reduce
prostaglandin and leukotriene production by inhibiting the enzyme phospholipase A2, which
converts phospholipids into arachidonic acid.
As a side note, non-steroidal anti-inflammatory drugs (NSAIDs), such as indole derivatives
(e.g.,indomethacin), pyrazolon derivatives (e.g., phenylbutazone), propionic acids (e.g.,
flurbiprofen), and the fenamates (e.g.,mefenamic acid) inhibit the enzyme cyclo-oxygenase
from producing prostaglandins further along in the inflammatory pathway. Because steroids
block the inflammatory pathway at a higher level, it makes sense that they are generally
superior to NSAIDs in reducing inflammation.
Steroids Commonly Used in Clinical Practice
Several steroids have been made synthetically for clinical use. Table 2 shows the relative anti-
inflammatory potencies of various corticosteroids, with hydrocortisone used as the standard
with a value of 1.0.
RELATIVE ANTI-
INFLAMMATORY
EQUIVALENT DOSE (mg)
CORTICOSTEROID RELATIVE POTENCY
Cortisone 25 0.8
Hydrocortisone 20 1
Prednisone 5 4
Prednisolone 5 4
Triamcinolone 4 5
Methylprednisone 4 5
Dexamethasone 0.75 25
Betamethasone 0.75 25
Table 2. Anti-inflammatory potencies of various corticosteroids relative to hydrocortisone
(source: Jaanus SD, Cheetham JK, Lesher GA. Antiinflammatory Drugs in Bartlett JD & Jaanus
SD. Clinical Ocular Pharmacology (4th Edition) 2001 Butterworth-Heinemann Chapter 12)
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 5 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
The effect of reducing inflammation depends heavily on the type and dosage of steroid used.
The most common steroid used by practitioners for oral use is prednisone. It is available in
tablet (1, 2.5, 5, 10, 20 mg amounts) and syrup forms (5, 6.7 and 15mg/mL concentrations).
Figure 3. Prednisone tablets (left) and syrup (image from MyAsthmaCentral.com website
http://www.healthcentral.com/asthma/)
Besides the oral route of administration, steroids can also be inhaled (such as in certain inhalers
for asthma treatment), injected either locally or intravenously (IV), and applied by the topical
administration. Table 3 shows some commercially available injectable steroids and their typical
route of administration. Table 4 lists the current commercially available topical steroids.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 6 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
CORTICOSTEROID TRADE NAME ADMINISTRATION ROUTE
Methylprednisolone Depo-Medrol IV, retrobulbar, transeptal
IV, subconjunctival/
Solu-Medrol tenons
Dexamethasone Decadron-LA IV, subconj/tenons, transeptal
Retrobulbar, intravitreal
Decadron Phosphate
Betamethasone Celestone Subconj/tenons, transeptal
Hydrocortisone (various Various IV, topical, subconj/tenons
forms)
Triamcinolone Aristocort, Kenalog Subconj/tenons, transeptal,
intravitreal
Table 3. Some commercially available injectable steroids and their typical administration
routes
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 7 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
TOPICAL OCULAR STEROID TRADE NAME CONCENTRATION/
FORMULATION
Prednisolone acetate Pred Forte (Allergan) 1.0% suspension
Econopred Plus (Alcon) 1.0% suspension
AK-Tate (Akorn) 1.0% suspension
Pred Mild (Allergan) 0.125% suspension
Econopred (Alcon) 0.125% suspension
Prednisolone sodium Inflamase Forte (CIBA) 1.0% solution
phosphate
Metreton (Schering) 0.5% solution
Inflamase Mild (CIBA) 0.125% solution
AK-Pred (Akorn) 0.125% solution
Dexamethasone alcohol Maxidex (Alcon), others 0.1% susp, ointment
Tobradex (Alcon) 0.1% susp, ointment
Fluorometholone acetate Flarex (Alcon) 0.1% suspension
Eflone 0.1% suspension
Fluorometholone alcohol FML (Allergan) 0.1% suspension
FluorOp 0.1% ointment
FML-Mild (Allergan) 0.25% suspension
Rimexolone Vexol (Alcon) 1% suspension
Medrysone alcohol HMS (Allergan) 1.0% suspension
Lotoprednol etabonate Lotemax (Bausch & Lomb) 0.5% suspension
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 8 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Alrex (Bausch & Lomb) 0.2% suspension
Zylet (Bausch & Lomb) 0.5% suspension
Table 4. Topical ocular steroids, listed from most potent (top) to least potent (bottom)
Figure 4. Various steroids used in eye care. Pred Forte (prednisolone acetate 1%) suspension
(left) is a commonly prescribed ophthalmic suspension. Hydrocortisone 1% cream (middle) is
often available over-the-counter. Kenalog (triamcinolone acetate) suspension (right) must be
injected in-office.
Note that most topical steroids (except for sodium phosphate forms of Prednisolone) are in
suspension form. This requires that the patient shake the bottle to evenly distribute the steroid
before instilling on the eye. Also of note, acetate forms of steroids generally have the greatest
anti-inflammatory property, followed by alcohol, then phosphate forms. Hydrocortisone 1%
ointment formulation, available over-the-counter but not available in ophthalmic formulation
currently, is sometimes used for certain periocular skin conditions such as contact dermatitis.
Likewise, triamcinolone (Kenalog) dermatological cream (available in 0.025%, 0.1% and 0.5%
concentrations) and other combination steroid/antibiotic ointments such as Maxidex,
Tobradex, Vasocidin, Blephamide, Cetapred, and Pred-G, could be considered as alternative
treatments. However, the practitioner should always be aware if they are prescribing a drug in
an off-label use. Tobradex (tobramycin 0.3% antibiotic + dexamethasone 0.1% steroid) and
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 9 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Zylet (tobramycin 0.3% antibiotic + lotoprednol 0.5% steroid) are the two steroid-antibiotic
combination ophthalmic suspensions prescribed currently.
Ocular Indications for Steroid Use
Ocular indications for steroids are numerous and include (but are not limited) to the following.
Eyelids blepharitis, chalazia, dermatitis, burns
Conjunctiva conjunctivitis (various types), mucocutaneous lesions, burns
Cornea edema, graft rejection, rosacea keratitis, dry eye syndrome, interstitial
keratitis, herpes simplex (stromal) keratitis, herpes zoster keratitis, post-herpes zoster
neuralgia, infiltrates, marginal ulcers, burns
Uvea iridocyclitis, uveitis, traumatic hyphema, sympathetic ophthalmia
Sclera episcleritis, scleritis
Retina vasculitis, chorio-retinitis
Optic Nerve neuritis, temporal arteritis
Orbit endophthalmitis, pseudotumor cerebri, Graves ophthalmopathy
Although optometrists frequently prescribe topical steroids for various ocular conditions as
listed above, injected or orally administered steroids are used less often. Ocular indications for
oral or injectable steroids include the following.
Uveitis not responding to topical therapy
Posterior uveitis and/or chorioretinitis
Orbital pseudotumor
Acute ocular allergic response not responding to topical therapy
Scleritis note subconjunctival injections are contraindicated
Temporal Arteritis/Arteritic Anterior Ischemic Optic Neuropathy
Optic Neuritis
Severe burns
Underlying autoimmune disease (collagen-vascular disorders)
Prednisone is available generically and is typically the least expensive of the steroids. Tablets
available in several dosages, with the 10 mg tablets being commonly used. Methylprednisone
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 10 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
is available in Dosepak packaging, consisting of six 4 mg tablets (totaling 24 mg) taken at once
the first day, with the dosage reduced by one tablet per day over the course of a week.
Figure 5. Methylprednisone Dosepak blister package
Methylprednisone therapy is typically not as effective as Prednisone therapy, which is normally
prescribed at between 40-80mg per day for a few days and then tapered gradually and evenly
over one to three weeks.
Take Steroids with Food
It is recommended that oral steroids be taken during meals to reduce the potential of causing
gastric ulcers. Amounts up to 60 mg can be taken at once, but higher dosages should be
divided equally between breakfast and dinner. The maximum therapeutic effect can be
achieved with the daily amount split equally into four dosages, with one dose taken every six
hours.
Tapering Steroid Dosage
An important rule is that the higher the potency or starting dosage of a steroid, or the longer it
is used, the longer the time period required for tapering. Since deaths have occurred from too
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 11 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
sudden a withdrawal from oral steroids, this rule should not be taken lightly. Suppression of
the H-P-A axis with steroid treatment is a serious concern, resulting in reduced adrenal
production of the bodys natural steroids. One study even demonstrated a reduction of natural
plasma cortisol levels by as much as 50% with topical dexamethasone use. Sudden cessation of
steroids heavily taxes the now atrophic adrenal cortex, potentially causing it to cease function.
This can lead to hypotension and shock.
With long-term (several weeks or more) use of oral steroids, it is recommended that dosage
should not be reduced by more than 0.5 to 1 mg every two to three weeks. Patients requiring
long-term steroid use should ideally be managed by their primary physician in coordination
with any specialists involved in treating their condition. In rare cases, however, such as an
acute dermatitis from a known chemical burn, a dose of 40-60mg per day for 48 hours with
immediate discontinuation may be safe.
Treatment of Ocular Conditions
Figure 6. Dry Eye Syndrome
Dry Eye Syndrome
The last few years have shown greater evidence that steroids may play a beneficial role in the
initial short-term management of dry eye. The 2007 Report of the International Dry Eye
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 12 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Workshop (DEWS) described several clinical trials that demonstrated an improvement in the
inflammatory nature of dry eye with topical ophthalmic methylprednisone 1% or lotoprednol
0.5% (Lotemax) on a four times a day drop dosage. The US Food and Drug Administration (FDA)
labels topical ophthalmic steroids for the treatment of steroid responsive inflammatory
conditions of the palpebral and bulbar conjunctiva, cornea and anterior segment of the globe
such as allergic conjunctivitis, acne rosacea, superficial punctate keratitis, herpes zoster
keratitis, iritis, cyclitis, selected infective conjunctivitides. Based on this labeling, topical
ophthalmic steroids may be indicated for treatment of keratoconjunctivitis sicca (KCS) due to
dry eye. Further support for the inflammatory aspect of dry eye is seen in the increased benefit
of topical ophthalmic cyclosporine 0.005% (Restasis), an antimetabolite drug that reduces the
production of inflammatory cytokines that potentiate the dry eye cycle. Clinical use of steroids
for KCS has been primarily with initiating soft steroids (i.e. those that have less ocular side-
effects) such as Lotemax or Alrex (lotoprednol 0.2% ophthalmic suspension) on a QID dosage
for 1 to 4 weeks, reducing to BID dosage for another 4 to 8 weeks. This can be done in
conjunction with preservative-free ocular lubricants. If improvement or resolution of signs or
symptoms of dry eye results, then conversion to long-term ophthalmic cyclosporine 0.005% on
BID dosage can be prescribed. At this time, long-term use of steroids for the management of
dry eye syndrome is not recommended.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 13 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Figure 7. Uveitis
Uveitis
Uveitis is probably the most common ocular indication for steroid treatment seen in optometric
practices. A general rule of thumb is to hit hard (i.e., initially use a topical steroid at least
every 2 hours then taper), and use a steroid with good anti-inflammatory potency (such as
ophthalmic prednisone acetate 1%) in combination with cycloplegia of the affected eye.
Posterior uveitis, in which the patient may show haze and cells in the vitreous and/or
chorioretinal inflammation, usually requires oral steroid treatment in addition to topical
treatment. Determining the underlying etiology of uveitis is also essential. It is possible that
the underlying etiology also requires an oral steroid for treatment particularly if the cause is
of an autoimmune nature.
Subconjunctival steroid injections are sometimes used in uveitis cases, but there is greater risk
of ocular side effects such as globe perforation, posterior subcapsular cataract formation and
ocular hypertension due to the bolus of steroid present. Regardless of route of administration,
steroid dosages should be tapered appropriately once resolution begins.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 14 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
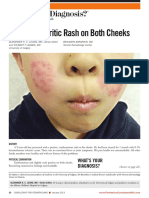
Figure 8. Contact Dermatitis
Contact Dermatitis
Contact dermatitis is a type IV (cell-mediated) allergic reaction involving the eyelids and
conjunctiva. It is typically caused by cosmetics as well as numerous antibiotics, preservatives,
and other medications or chemicals. Removing the offensive substance is first priority,
combined with cool compresses and possibly oral tetracycline or doxycycline.
Topical steroid ointments or creams such as 0.5% to 1% hydrocortisone or 0.1%
dexamethasone three times a day for a few days may be very useful in reducing edema and
inflammation. However, the practitioner should be aware that combination antibiotic/steroid
drugs may worsen the condition if the patient is sensitive to the associated antibiotic (ie:
neomycin). Also, fluorinated steroids can cause persistent dermatitis.
Occasionally, patients may present with scaly, itchy eyelids or periocular skin that indicates
eczematous inflammation. These patients also benefit from topical steroid ointments or
creams, as noted above. Once resolution begins, tapering of the steroid can occur.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 15 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Figure 9. Scleritis
Scleritis
Scleritis, typically involving inflammation of the scleral, episcleral, and conjunctival vessels, is
another ocular condition in which steroids may be necessary. Their use may be indicated if
NSAIDs are ineffective in treating the associated eye pain.
The presentation of scleritis is almost always raises the suspicion for underlying autoimmune
disease such as rheumatoid arthritis or other connective tissue disorders, so, like certain
uveitides, oral steroid treatment may benefit both the ocular and systemic conditions
concurrently.
Typical dosage is 60 to 100 mg of oral prednisone per day for one week, followed by no more
than a 10 mg per day taper for two to three weeks. It should be noted that topical steroids
have limited effectiveness with scleritis, and that subconjunctival steroid injections are
contraindicated with scleritis due to the higher risk of tissue necrosis.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 16 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Figure 10. Chalazion
Chalazion
Chalazia are longstanding sterile granulomatous infiltrations of the meibomian glands resulting
from a quiescent hordeola. They can also appear spontaneously. The patient reports a hard,
immobile lump that is not painful to the touch. Most chalazia are simply an irritant or cosmetic
inconvenience, and one in four resolve without treatment.
Persistent chalasia that do not respond to warm compresses, digital massage, and oral
antibiotics may require curettage and excision or an intralesional injection of steroid such as
triamcinolone (Kenalog). After local anesthesia, a dose of 0.05 to 0.3 ml of a 5 to 40mg/mL
suspension can be injected into the lesion using a 27-30 gauge needle. Resolution typically
occurs in 1-2 weeks, but may require a second injection a few weeks later if the chalazion is
large. The steroid serves to suppress the inflammatory cells that reside within the chalazion.
Depigmentation of the skin at the injection site may occur, but may be avoided by conjunctival
versus transepithelial injection. The depigmentation usually reverses.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 17 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Figure 11. Arteritic Anterior Ischemic Optic Neuropathy
Arteritic Anterior Ischemic Optic Neuropathy
Arteritic Anterior Ischemic Optic Neuropathy (also known as temporal arteritis) is an indication
for the immediate prescription of oral prednisone. Classic findings include jaw claudication,
tenderness of the temporal scalp area and the head and neck areas, notably reduced vision in
one eye, and an elevated Erythrocyte Sedimentation Rate (ESR).
This idiopathic vasculitis typically affects 1:1000 individuals over the age of 50, most often
women. Up to 75% of patients who have reduced vision in one eye (the typical initial
presentation) will develop reduced vision in the contralateral eye within 24 hours to weeks,
resulting in bilateral blindness in up to half of untreated patients. Although prognosis for the
initially involved eye is poor, prompt steroid treatment (either oral or intravenous) may prevent
the incidence of contralateral eye involvement to less than 1% over a five-year duration.
Usually treatment with 80-120 mg/day of prednisone may be initiated, but if significant visual
reduction is present, up to 250 mg of intravenous hydrocortisone or 250 mg of
methylprednisone every 6 hours for four days is preferred over oral treatment. The patient
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 18 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
should be referred promptly for hospitalization and adjustment of steroid dosage according to
symptoms and ESR levels. Oral prednisone 80-100 mg/day for 2-3 weeks typically follows the
intravenous treatment with dosages tapered over several months to years.
Figure 12. Optic Neuritis
Optic Neuritis
Optic neuritis is another condition in which steroids can play an important treatment role.
Typically in younger patients (e.g., ages 18-45 years), optic neuritis may be associated with a
relatively sudden onset of pain on eye movement, poor to no pupil response in the affected eye
or eyes, variable visual field defects, desaturation of color vision, and/or loss of visual acuity.
Causes range from idiopathic to infective to systemic conditions such as multiple sclerosis, so
the practitioner must first try to determine the cause if possible before initiating treatment.
The Optic Neuritis Treatment Trial (ONTT) demonstrated that using oral steroids alone may
actually exacerbate the condition. The preferred treatment is intravenous methylprednisolone
for the first few days followed by oral prednisone tapered over a few weeks.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 19 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Determining and treating the underlying cause is the most important management approach.
One must remember that steroids are considered palliative therapy that is, they suppress the
inflammatory response (and often the pain associated with the inflammation) but the
underlying cause of the disease remains.
Figure 13. Herpetic Keratitis
Herpetic Keratitis
Steroid treatment for herpetic keratitis has been a controversial subject. Steroids typically slow
epithelial healing and suppress the host immune response, which may set the stage for
worsening of the herpetic infection or lead to stromal keratitis.
Therefore, it is not recommended by this author to use steroids with epithelial dendritic
keratitis. However, should the inflammation move to the stroma (e.g., disciform keratitis),
topical steroids should be used alternating with antiviral medications several times per day to
reduce the potential of stromal scarring and visual loss. Steroids also reduce stromal
inflammation that impedes proper cornea epithelial migration.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 20 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Topical antibiotic/steroid ointment applied two to four times daily to vesicular skin lesions
along the dermatome may be useful in cases of severe zoster-related post-herpetic neuralgia.
Topical steroids can be also used to treat the many forms of herpes zoster keratitis that involve
the corneal stroma, in conjunction with antiviral medications.
Figure 14. Herpes Zoster Dermatologic Lesions
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 21 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Figure 15. Macular Edema (as seen on fluorescein angiogram)
Macular Edema
Although currently not part of the optometrists scope of practice, the benefits of intravitreal
and sub-Tenons injections of steroid in the resolution of macular edema and inflammation has
been increasingly noted both clinically, and in several studies. Ocular coherence tomography
and fluorescein angiography have shown a faster resolution of macular swelling with
intravitreal triamcinolone (Kenalog) injection. Typically a 4mg amount is injected into the
vitreal space. Use of triamcinolone for the treatment of clinically-significant macular edema
(CSME) and certain forms of macular degeneration have also been investigated, with positive
results. Further protocols are being developed in the use of triamcinolone injections for these
retinal conditions. For further information on this treatment, refer to the authors other web
C.E. article: Acquired Macular Diseases: Pathophysiology, Diagnosis and Management.
Ocular and Systemic Side-Effects of Steroids
Although steroids may be considered by some to be a panacea for many conditions, their ocular
and systemic side effects are numerous and should be well understood by the optometrist.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 22 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
OCULAR SIDE EFFECTS SYSTEMIC SIDE EFFECTS
Posterior subcapsular cataracts Adrenal insufficiency
Ocular hypertension/glaucoma Cushingoid syndrome
Secondary ocular infection Gastric ulceration
Slowed corneal epithelial healing Hyperglycemia/diabetes
Uveitis Reduced immunity/fever
Increased corneal thickness Liver disease; jaundice
Transient ocular discomfort Severe mood changes
Ptosis Delayed wound healing
Exophthalmos (injected steroids) Osteoporosis
Globe perforation (injected steroids) Menstrual cycle changes or cessation
Tissue necrosis (injected steroids) Elevated intracranial pressure
Eyelid depigmentation (injected Reduced growth in children
steroids) Miscarriage in pregnant women
Hemorrhage of ocular tissue Generalized edema
Corneal or scleral thinning Encourage blot clots
Spread of epithelial herpes keratitis Convulsions
Muscle wasting
Lowered sex hormone levels
Lowered potassium levels
Fragile skin, acne
Reduced sperm count
Male-pattern baldness (men +
women)
Passed through breast milk
Table 5. Ocular and systemic side effects of steroids
Posterior subcapsular cataracts and ocular hypertension are the classic potential ocular side
effects of steroid use and may occur with any route of steroid administration. Long-term
therapy (e.g., a year or more) can cause these problems, but children may manifest these
sequelae more rapidly. Steroid type also plays a role, with prednisone and dexmethasone
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 23 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
having greater propensity to cause increased intraocular pressure versus lotoprednol or
florometholone, which have less potential. Intraocular pressure measurement and lens
condition should be checked regularly (each examination) for patients using steroids.
Figure 16. Posterior subcapsular cataract (seen on retro-illumination off the fundus)
For those patients who are steroid responders, tapering off the steroid usually lowers the
pressure back to baseline level. Mechanisms of action for the ocular side effects of steroid use
are still not well known. It is thought that steroids affect the trabecular meshwork cellular
metabolism regulating aqueous outflow, and changing the posterior lens sub-capsular fiber
arrangement, but these actual processes are still being investigated.
Reduced epithelial healing and reduced immunity can occur with steroid use. Therefore these
drugs should be avoided when treating acute bacterial or fungal infections or when there is a
significant corneal epithelial defect over non-inflamed stroma. If steroid use is required, it
should be done in combination with an anti-infective agent or agents.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 24 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
The author has found clinically that recent adenoviral infiltrative infections, which show no
epithelial compromise, respond favorably to topical steroid treatment.
Various complications to ocular tissues can occur from injectable steroids, typically related to
the injection itself rather than to the steroid. Subconjunctival injections can cause the greatest
intraocular pressure rise due to proximity of the steroid to the trabeculum, whereas
retrobulbar injections increase risk of physical damage to the optic nerve regardless of the
agent being injected.
Figure 17. Buffalo hump resulting from prednisone use
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 25 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Figure 18. Supraclavicular fat pads resulting from prednisone use
The Cushingoid side effect of systemic steroid use mirrors Cushings Syndrome (cortisol
hypersecretion by the adrenal glands). In this condition, fat deposition on the back of the neck
and face create the classic round moon face and buffalo hump typical of the condition.
Weight gain, hirsutism (male-pattern hair growth), acne, hypertension and mood changes
including psychosis and suicidal tendencies are also associated with steroid use.
Other potential systemic problems include gastric ulcers due to the steroid reducing protective
prostaglandin secretions in the gut. Concurrent treatment with H2-receptor antagonists such
as ranitidine (Zantac) 150 mg BID, famotidine (Pepcid) 20 mg BID, or a proton pump inhibitor
such as omeprazole (Prilosec) or lansoprazole (Prevacid) as well as taking steroids with meals
may help protect the gut.
Hyperglycemia potentially leading to steroid-induced diabetes may also occur, as well as
electrolyte disturbances such as sodium retention and potassium depletion. Potassium
supplements (e.g., Slow-K) may be necessary for the patient using steroids.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 26 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Retardation of skeletal growth in children has been reported, even with low dosages (e.g., 8
mg per day), and inhibition of osteoblast activity may affect ribs and vertebrae, causing
osteoporosis.
Increased susceptibility to infection and poor wound healing are also points to note, and
women should be cautioned of potential miscarriages, menstrual problems, and passage of
the steroid in the breast milk to nursing babies.
Mood swings, (into) psychosis, euphoria, or depression can occur with steroid treatment, and
the patient should be made aware of this.
Contraindications to Using Steroids
As the side effects above indicate, steroids can precipitate or exacerbate a condition in at-risk
individuals. Table 6 lists potential ocular and systemic conditions that may be relative or
absolute contraindications to steroid use.
OCULAR CONTRAINDICATIONS SYSTEMIC CONTRAINDICATIONS
Glaucoma Peptic ulcer disease
Cataracts Diabetes/hyperglycemia
Herpetic epithelial infections Osteoporosis
Acute bacterial or fungal infection Renal disease
Significant corneal epithelial defect Immunocompromise
Unsure diagnosis Mental health problems
Pregnancy
Congestive heart failure
Systemic hypertension
Table 6. Potential ocular and systemic contraindications to steroid use
Steroids may reduce the response to anticoagulant therapy, so combining steroid therapy with
aspirin or other anticoagulants may be contraindicated. Rifampin, phenylbutazone, and
phenytoin may also reduce the effect of systemic steroids.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 27 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
Systemic Steroid Prescribing
Ideally, a full medical history, physical and blood work-up (including blood pressure, glucose
evaluation, complete blood count and organ function) should be performed before prescribing
any systemic steroid, to rule-out any contraindications. Medical evaluations should continue
during any extended use of systemic steroids. The benefit of taking a systemic steroid should
always outweigh the risk. Proper dosage based on age, weight, and the condition being treated
should be carefully determined. The minimum dose to safely provide the therapeutic effect is
the goal. Dose packs are useful for short-term use of a steroid. However, long-term steroid
use requires careful tapering once resolution of the conditions begins. This tapering should be
longer when the duration of treatment is longer. Some patients may only require a taper over
a few days, while others may require a taper that extends over many months. Consultation and
follow-up communication with the patients primary care provider should be an essential part
of systemic steroid treatment.
Summary
Optometric physicians should be knowledgeable of the mechanism, routes of administration,
potential side effects, indications, and contraindications of steroid use. When patients are
treated with steroids, judicious application is recommended, and communication with the
patients primary care provider and/or other specialists is recommended. However, even with
these concerns and precautions, the power of steroids in managing a myriad of ocular diseases
and underlying systemic conditions holds testament to their great value in patient care.
References
1. Katzung B. Basic and Clinical Pharmacology (7th Ed.). Appleton & Lange, Stamford,
Connecticut, 1998.
2. Zimmerman T, Kooner K, Sharir M, Fechtner R. Textbook of Ocular Pharmacology.
Lippincott-Raven, New York, New York. 1997.
3. Rhee J, Pyfer MF (Eds.). The Wills Eye Manual (3rd Ed). Lippincott, Williams and Wilkins,
1999.
4. Jaanus SD. Anti-inflammatory drugs. in Bartlett JD, Jaanus SD, eds. Clinical Ocular
Pharmacology (3rd Ed). Butterworth-Heinemann, Boston, 1996.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 28 of 29
Application of Topical, Injection, and
Oral Corticosteroids in Ocular Disease
Management
Author: Lorne B. Yudcovitch OD, MS, FAAO
COPE #22300-AS 2 credit
5. Davis AR, et al. Topical steroid use in the treatment of ocular alkali burns. British
Journal of Ophthalmology 81:732-4, 1997.
6. Hardman JG, Limbird LE, Gilman AG, eds. Goodman & Gilman's The Pharmacological
Basis of Therapeutics (10th Ed.). McGraw-Hill Publishing, New York, 2001
7. Kanski JJ. Clinical Ophthalmology (3rd Ed.). Butterworth-Heinemann, Oxford. 1994.
8. Fiscella RG, et al. Generic prednisolone suspension substitution. Archives of
Ophthalmology. 116(5):703. 1998.
9. Spalton DJ, Hitchings RA, Hunter PA. Atlas of Clinical Ophthalmology (2nd Ed.). Gower
Medical, 1994.
10. Glanze WD, Anderson KN, Anderson LE (Eds.). The Mosby Medical Encyclopedia
(Revised Ed.). C.V. Mosby Company, New York, 1992.
11. U.S. Food and Drug Administration Center for Drug Evaluation and Research.
12. Consumer Drug Information Sheet: Zylet
13. http://www.fda.gov/cder/consumerinfo/druginfo/zylet.HTM
14. Drugs.com Prescription drug information for consumers and professionals. Maxitrol.
http://www.drugs.com/mtm/M/Maxitrol.html
15. National Institute of Health National Institute on Drug Abuse: NIDA InfoFacts: Steroids
(Anabolic-Androgenic). http://www.nida.nih.gov/Infofacts/steroids.html
16. My Health Central website, asthma section. http://www.healthcentral.com/asthma/
17. EyeRounds.org. University of Iowa Department of Ophthalmology website.
http://webeye.ophth.uiowa.edu/eyeforum/
18. Pflugfelder S. Antiinflammatory therapy for dry eye. American Journal of
19. Ophthalmology, 2003. Volume 137 , Issue 2 , Pages 337 342.
20. Gipson, Ilene K. et al. Research in Dry Eye: Report of the Research Subcommittee.of the
International Dry Eye WorkShop (2007). The Ocular Surface, Volume 5, Number 2, April
2007, pp. 179-193(15)
21. Rafael Ernane AA, Cristina M, Michel EF. Intravitreal triamcinolone acetonideinjection in
the treatment of Vogt-Koyanagi-Harada syndrome Arq. Bras. Oftalmol. vol.67 no.3 So
Paulo 5/6 2004
22. Konstantopoulos A, Williams CP, Luff AJ. Outcome of intravitreal
triamcinolone acetonide in postoperative cystoid macular oedema. Eye. 2006 Sep 29.
23. Audren F, et al. Intravitreal triamcinolone acetonide for diffuse diabetic
macular oedema: 6-month results of a prospective controlled trial. Acta Ophthalmol
Scand. 2006 Oct;84(5):624-30.
Copyright Pacific University, Forest Grove, Oregon, USA
Documents and materials located on the Pacific University gopher, WAIS, WWW, phonebook, and FTP servers are
copyrighted by the Pacific University, or by the authors of the individual documents, and are provided for the
convenience of university faculty, students, and staff, with no warranty of accuracy or usability.
www.pacificu.edu/optometry/ce Page 29 of 29
You might also like
- Adrenocorticosteroids & Adrenocortical AntagonistsDocument20 pagesAdrenocorticosteroids & Adrenocortical Antagonistsapi-3859918No ratings yet
- 655 FullDocument16 pages655 FullGhina nurulNo ratings yet
- CorticosteroidsDocument49 pagesCorticosteroidskaleab AlemayehuNo ratings yet
- Corticosteroids and Associated DiseasesDocument76 pagesCorticosteroids and Associated DiseasesALNAKINo ratings yet
- Dosis Estrés 2019Document6 pagesDosis Estrés 2019Braulio SantanaNo ratings yet
- #6 Adrenocorticosteroids 5 PDFDocument8 pages#6 Adrenocorticosteroids 5 PDFOmar BasimNo ratings yet
- Safety of Medications in Pediatric EndocrinologyDocument12 pagesSafety of Medications in Pediatric EndocrinologyandreNo ratings yet
- Dermatology: RoundsDocument6 pagesDermatology: RoundsPin Wijaya100% (1)
- 18 Applied PharmacologyDocument88 pages18 Applied Pharmacologyrajkamal kNo ratings yet
- The Eicosanoids: Prostaglandins, Thromboxanes, Leukotrienes, & Related CompoundsDocument60 pagesThe Eicosanoids: Prostaglandins, Thromboxanes, Leukotrienes, & Related CompoundsMer CiNo ratings yet
- Pharmacology of Adrenocorticoids and Adrenocorticotropic AntagonistsDocument32 pagesPharmacology of Adrenocorticoids and Adrenocorticotropic AntagonistsJoyce VillanuevaNo ratings yet
- Adrenocortical AgentsDocument14 pagesAdrenocortical AgentsFredie O HadjimudinNo ratings yet
- Atow 470 00Document7 pagesAtow 470 00rogelio cruzNo ratings yet
- SteroidsDocument22 pagesSteroidsLuqman QadirNo ratings yet
- Pharmacological effects and clinical applications of corticosteroids in dentistryDocument27 pagesPharmacological effects and clinical applications of corticosteroids in dentistryFinnyalfNo ratings yet
- Corticosteroids: Saitoti S. Clinical Pharmacologist UdomDocument33 pagesCorticosteroids: Saitoti S. Clinical Pharmacologist UdomZabron LuhendeNo ratings yet
- Bnab 014Document38 pagesBnab 014RodrigoNo ratings yet
- Corticosteroid: 1 Mineralocorticoids, Mainly Aldosterone in Humans Have SaltretainingDocument5 pagesCorticosteroid: 1 Mineralocorticoids, Mainly Aldosterone in Humans Have Saltretaining우영박No ratings yet
- CorticosteroidsDocument42 pagesCorticosteroidsejiNo ratings yet
- Obat Golongan KortikosteroidDocument43 pagesObat Golongan KortikosteroidFitri Andriani IbrahimNo ratings yet
- A Review On Pharmacological and Analytical Aspects of Diosgenin: A ConciseDocument7 pagesA Review On Pharmacological and Analytical Aspects of Diosgenin: A ConciseAshu GadewarNo ratings yet
- Adrenal Insufficiency in Critical IllnessDocument16 pagesAdrenal Insufficiency in Critical IllnessjazluisjoyaNo ratings yet
- Administering Corticosteroids in Neurologic Diseases3724Document12 pagesAdministering Corticosteroids in Neurologic Diseases3724Carmen BritoNo ratings yet
- Badr Et Al, 2020Document10 pagesBadr Et Al, 2020UrwaTariqNo ratings yet
- Current Approach CAH and Adrenal Insuf 2015Document20 pagesCurrent Approach CAH and Adrenal Insuf 2015Pablo MoraNo ratings yet
- Protein Binding: Naila Abbasi Assistant Professor Department of PharmacyDocument50 pagesProtein Binding: Naila Abbasi Assistant Professor Department of PharmacyMuhammad MursaleenNo ratings yet
- Adrenocorticosteroids RevisedDocument56 pagesAdrenocorticosteroids RevisedGhina RizwanNo ratings yet
- The Role of Drug Metabolizing Enzymes in Clearance - UGTDocument16 pagesThe Role of Drug Metabolizing Enzymes in Clearance - UGTSHASHIKANT PAWARNo ratings yet
- Host Modulation Therapy: Presented By: Pallavi Prashar Mds Ii YearDocument50 pagesHost Modulation Therapy: Presented By: Pallavi Prashar Mds Ii YearGopuNo ratings yet
- The Gonadal Hormones & InhibitorsDocument41 pagesThe Gonadal Hormones & InhibitorsSaddamix AL OmariNo ratings yet
- 04.02-01 Endocrine IIDocument6 pages04.02-01 Endocrine IIMaikka IlaganNo ratings yet
- Lecture 10 Steroids (Week 12)Document9 pagesLecture 10 Steroids (Week 12)ahmadslayman1No ratings yet
- Host ModulationDocument17 pagesHost ModulationIbrar HumayunNo ratings yet
- Drugs Treating ArthritisDocument38 pagesDrugs Treating ArthritisDere RawandNo ratings yet
- Congenital Adrenal HyperplasiaDocument29 pagesCongenital Adrenal HyperplasiaMohan RaoNo ratings yet
- Adrenal Hormones: Pituitary Gland Consists of 3 LobesDocument9 pagesAdrenal Hormones: Pituitary Gland Consists of 3 LobesMoha MedNo ratings yet
- ChoiDocument19 pagesChoiLuciana RafaelNo ratings yet
- Role of Drugs in Orthodontics / Orthodontic Courses by Indian Dental AcademyDocument239 pagesRole of Drugs in Orthodontics / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Corticosteroid-Related Central Nervous System Side Effects: Case ReviewDocument6 pagesCorticosteroid-Related Central Nervous System Side Effects: Case Revieweva.mmNo ratings yet
- Pharmacodynamic Pharmacokinetic of CorticosteroidDocument34 pagesPharmacodynamic Pharmacokinetic of CorticosteroidIvaNo ratings yet
- Corticosteroid Adverse Effects - StatPearls - NCBI BookshelfDocument12 pagesCorticosteroid Adverse Effects - StatPearls - NCBI Bookshelfantonio.mastrangelo.999No ratings yet
- SteroidsDocument25 pagesSteroidsalhusien.abd2000No ratings yet
- CorticosteroidsDocument18 pagesCorticosteroidsمحمد العراقيNo ratings yet
- Anti Inflammatory and Immuno Supressive Effects of GlucocorticoidsDocument50 pagesAnti Inflammatory and Immuno Supressive Effects of GlucocorticoidssiddardhaNo ratings yet
- Systemic and Local Applications of Steroids in Endodontics: An Update ReviewDocument8 pagesSystemic and Local Applications of Steroids in Endodontics: An Update ReviewJorge OrbeNo ratings yet
- Update On Management of The Oral and Maxillofacial Surgery Patient On CorticosteroidsDocument12 pagesUpdate On Management of The Oral and Maxillofacial Surgery Patient On Corticosteroidsconstanza gormazNo ratings yet
- Adrenocortical AgentsDocument8 pagesAdrenocortical AgentsKarina Madriaga100% (1)
- 1.2 CorticosteroidsDocument9 pages1.2 Corticosteroidsua091031No ratings yet
- Corticosteroids Group Project Covering Types, Mechanisms, Uses, Side EffectsDocument10 pagesCorticosteroids Group Project Covering Types, Mechanisms, Uses, Side EffectsMahnoor ArshadNo ratings yet
- Drugs Affecting Corticosteroid LevelsDocument24 pagesDrugs Affecting Corticosteroid LevelsAshaNo ratings yet
- VACDocument39 pagesVACkarthikaNo ratings yet
- Practical Diabetes International - November December 1996 - Dunning - Corticosteroid Medications and Diabetes MellitusDocument3 pagesPractical Diabetes International - November December 1996 - Dunning - Corticosteroid Medications and Diabetes MellitusAura DiscyacittaNo ratings yet
- Adrenocorticoids & Their Physiologic EffectsDocument77 pagesAdrenocorticoids & Their Physiologic EffectsSamson100% (1)
- Biopharmaceutics &pharmakinetics: Subject Code-604t Unit - 1Document27 pagesBiopharmaceutics &pharmakinetics: Subject Code-604t Unit - 1Babbu Singh GurjarNo ratings yet
- Pharmacologic Principles NURSINGDocument69 pagesPharmacologic Principles NURSINGYousef JafarNo ratings yet
- Classification of Toxic Effects 2Document62 pagesClassification of Toxic Effects 2zeynep deren sayNo ratings yet
- Supra R RenalDocument24 pagesSupra R RenalAriadna Torres LpzNo ratings yet
- 5 - Pharmacology of Corticosteroids (Final)Document14 pages5 - Pharmacology of Corticosteroids (Final)Morad KananNo ratings yet
- Lipid MediatorsFrom EverandLipid MediatorsFiona M. CunninghamNo ratings yet
- Form SpirometriDocument1 pageForm SpirometriloraNo ratings yet
- Materi Prof - Dr.aanthony TanDocument4 pagesMateri Prof - Dr.aanthony TanloraNo ratings yet
- Ovarian Cysts JournalDocument7 pagesOvarian Cysts JournalFandi AhmadNo ratings yet
- Maat 12 I 3 P 271Document5 pagesMaat 12 I 3 P 271loraNo ratings yet
- Weight-For-Length GIRLS: Birth To 2 Years (Z-Scores)Document1 pageWeight-For-Length GIRLS: Birth To 2 Years (Z-Scores)Malisa LukmanNo ratings yet
- AcsDocument9 pagesAcsMayer RosenbergNo ratings yet
- Chapter II PDFDocument22 pagesChapter II PDFloraNo ratings yet
- Tinea Incognito - Jan. 2013Document3 pagesTinea Incognito - Jan. 2013loraNo ratings yet
- Grave DiseaseDocument34 pagesGrave DiseaseloraNo ratings yet
- Dermatophytosis PDFDocument13 pagesDermatophytosis PDFsimcassNo ratings yet
- Itch and Nerve Fibers With Special Reference To AtopicDocument8 pagesItch and Nerve Fibers With Special Reference To AtopicloraNo ratings yet
- Notes For USMLE Rx-01312019-Part IDocument410 pagesNotes For USMLE Rx-01312019-Part IjillNo ratings yet
- Congenital Adrenal Hyperplasia: Presented By: Ahmad Fazwan JunaidiDocument16 pagesCongenital Adrenal Hyperplasia: Presented By: Ahmad Fazwan JunaidiZakirNo ratings yet
- The Impact of Stress On HealthDocument40 pagesThe Impact of Stress On Healthmamak88No ratings yet
- Mind Map On Endocrinology of Human For BSC StudentsDocument3 pagesMind Map On Endocrinology of Human For BSC Students2023ebcs499No ratings yet
- Adrenocorticosteroids: C39 Adrenocorticosteroids & Adrenocortical AntagonistsDocument5 pagesAdrenocorticosteroids: C39 Adrenocorticosteroids & Adrenocortical AntagonistsHydieNo ratings yet
- GLUCOCORTICOIDS AND METABOLISMDocument34 pagesGLUCOCORTICOIDS AND METABOLISMCrystine SinatraNo ratings yet
- Endocrine ConditionsDocument5 pagesEndocrine ConditionsGlen DizonNo ratings yet
- Lecture10 CommunicationIII 1Document30 pagesLecture10 CommunicationIII 1Liana Rose MeregildoNo ratings yet
- Reiki Level 1 ManualDocument29 pagesReiki Level 1 ManualFabian DeeNo ratings yet
- Pharmacology 4th Semester BSN Notes, Educational PlatformDocument985 pagesPharmacology 4th Semester BSN Notes, Educational PlatformPen N PapersNo ratings yet
- Semper Fit Advance Fitness CourseDocument255 pagesSemper Fit Advance Fitness CourseUnited States Militia73% (11)
- Waxes and SteroidsDocument7 pagesWaxes and SteroidsAllyssa FernandezNo ratings yet
- Adrenal GlandsDocument116 pagesAdrenal GlandsBrandon AreteNo ratings yet
- Case Study HyperkalemiaDocument10 pagesCase Study HyperkalemiaJamaica Cerrero100% (1)
- Blood Pressure RegulationDocument11 pagesBlood Pressure RegulationManuNo ratings yet
- Endocrinology Part 2Document6 pagesEndocrinology Part 2Prabhjot MundiNo ratings yet
- 4-The Adrenal Gland - AldosteroneDocument20 pages4-The Adrenal Gland - AldosteroneAndrie Gunawan100% (1)
- Psycho - TextDocument137 pagesPsycho - TextsajithaNo ratings yet
- Adrenal GlandsDocument28 pagesAdrenal GlandsMegan ZikNo ratings yet
- Case Study Addison's Disease Part 1Document27 pagesCase Study Addison's Disease Part 1Whitney PierreNo ratings yet
- The Nutritional Relationships of MagnesiumDocument5 pagesThe Nutritional Relationships of MagnesiumwynvelNo ratings yet
- How Chakras Interact with the Endocrine SystemDocument11 pagesHow Chakras Interact with the Endocrine SystemNalini Muniyendi100% (2)
- Acetaminophen Increases Aldosterone Secretion While SuppressingDocument7 pagesAcetaminophen Increases Aldosterone Secretion While SuppressingKhánh Nguyễn NgọcNo ratings yet
- 3rd BSC Endocrinology NotesDocument25 pages3rd BSC Endocrinology NotesPratyashaNo ratings yet
- Azimat Nuclear PDFDocument2,054 pagesAzimat Nuclear PDFrahmatNo ratings yet
- Congenital Adrenal HyperplasiaDocument28 pagesCongenital Adrenal HyperplasiaWindelyn Gamaro0% (1)
- X ICSE Endocrine System-1 PDFDocument9 pagesX ICSE Endocrine System-1 PDFthe lillyNo ratings yet
- Apbio 45 LectoutDocument15 pagesApbio 45 LectoutSimone Alexis GuinocorNo ratings yet
- Health Psychology Canadian 4th Edition Taylor Solutions ManualDocument32 pagesHealth Psychology Canadian 4th Edition Taylor Solutions ManualJosephWilliamsinaom100% (13)
- Endocrine System CH 9Document57 pagesEndocrine System CH 9Gibraluve Barbado PonceNo ratings yet