Professional Documents
Culture Documents
ABG Poster A3 PDF
Uploaded by
Rafaela BritoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ABG Poster A3 PDF
Uploaded by
Rafaela BritoCopyright:
Available Formats
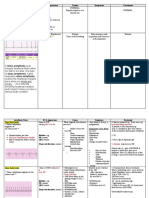
ABG...EASY AS...
1,2,3
NORMAL VALUES & DEFINITIONS 3 STEPS TO ABG INTERPRETATION
1. What is the pH? Is it alkolotic (57.45) or acidotic (67.35)?
NAME DEFINITION VALUE
2. Whats happening with the respiratory system (CO2) and the metabolic systems (HCO3-)?
pH Refers to hydrogen ion (H+) levels, hence 7.35 - 7.45 If the problem is in the lungs (respiratory) the CO2 will be heading in the opposite direction of the pH.
the H in pH. H+ levels are important For example: respiratory acidosis: The pH will be low - 6pH 7.22 and the CO2 will be high - 5CO2 55mmhg
If the problem is metabolic the HCO3 will head in the same direction as the pH
because a lack of (deficit) or too much For example: metabolic alkalosis: The pH will be high - 57.55 and the HCO3- will also be high HCO3- 535mmol/L.
(excess) will tell you if the patient is Note: an easy way to remember for a Metabolic problem, think M as in the pH will head in the saMe direction as the
acidotic or alkolotic. One confusing point HCO3-. For respiratory the pH will head in the Opposite direction as the CO2.
about pH is that it is an INVERSE ratio, 3. Is there any (if any) compensation occurring?
No compensation:
which means that the more H+ present, the pH remains abnormal, and the other value (where the problem isnt occurring, i.e. CO2 or HCO3-) will remain normal or has
lower the pH and vice versa. made no attempt to help normalise the pH.
Acid Can give away a H+ or can separate 20 parts base / For example: in uncompensated metabolic acidosis:
pH 67.23, HCO3- 6 15mmol/L, and the CO2 will be normal at 40mmHg.
(dissociate) hydrogen from its ion, so the 1 part acid Partial compensation
hydrogen is not positive and therefore no pH is still abnormal, and the other value is abnormal in an attempt to help normalise the pH.
For example: in partially compensated respiratory alkolosis:
longer an acid. pH 57.62, CO2 627 and the HCO3- will be abnormal at 617mmol/L
Acids are end products of metabolism and Full compensation
The pH is normal, as the other value is abnormal and has been successful in normalising the pH.
must be buffered or excreted to achieve a For example: Fully compensated metabolic acidosis
normal pH pH 7.38, HCO3- 615mmol/L and the CO2 630mmHg 6
Base Unlike Acids, bases can accept a H+ and
bond with hydrogen. They are all negative WHAT CAUSES THESE CHANGES?
and like to buffer body acids. METABOLIC ACIDOSIS
Can be caused by either an increase in circulating acids and or a loss of base (HCO3-). These include:
Base excess / Represents an increase or decrease in the -2 to +2mmol/L Renal failure (unable to excrete acids or H+)
Lactic acidosis (increase in circulating acids)
Base deficit amount of base compared with the amount Keto - acidosis (increase in circulating acids)
of acids present Diarrhoea (HCO3- loss)
METABOLIC ALKOLOSIS
Can be caused by an increase in HCO3- or loss of metabolic acids. These include:
Prolonged vomiting (acid loss)
HCO3- Concentration of hydrogen carbonate in 22-26mmol/L GI suctioning (acid loss)
Hypokalaemia (H+ (an acid) excreted to maintain electrolyte balance)
blood. Used to determine along with pH RESPIRATORY ACIDOSIS
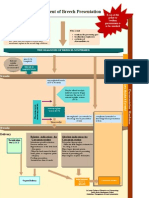
and CO2 source of acid base imbalance. Caused by increased CO2 levels which is then converted to an acid (H+) as the body tries compensate by excreting acids via the
kidneys. These include:
Hypoventilation:
- sedatives/sedation/opiates
pCO2 Carbon dioxide partial pressure (tension). 35-45 mmhg Depression of respiratory centre in brain stem via trauma
Pneumonia
Reflects alveolar ventilation as it diffuses Pulmonary oedema
across the alveolar capillary membrane and Asthma
RESPIRATORY ALKALOSIS
blown off. Caused by a hyperventilation, the body getting rid of too much CO2, for example:
Anxiety
Hypoxaemia (caused by heart failure)
paO2 Arterial oxygen tension. In other words 75-100mmhg
how well the lungs are able to pick up TREATMENT GOALS/GUIDELINES
oxygen, i.e. supply, but not demand (this
As with both acidosis and alkolosis, there needs to be a diagnosis of why the patients acid base status is such. Treatment is then
is shown in a mixed venous gas, discussed aimed at stabilising the initial/presenting problem as well the acid-base status. However, general guidelines include correcting the
later). fluid balance and electrolyte status. Continuous regular ABG monitoring and recording for trends. Possible dialysis to remove
excess lactate, manipulation of ventilation settings to adjust CO2 levels, but always maintaining tissue perfusion. Depending
Lactate When cells no longer have enough O2 for 0.5 - 2.0mmol/L on severity of HCO3- levels and pH - possible sodium bicarbonate infusion (this is controversial however). Of course any of the
(Lactic Acid) normal aerobic metabolism (cell hypoxia) adjustments made should only be done with an order from a medical officer, and must go through the intensive care team before
Anaerobic metabolism takes over resulting any changes to treatments are applied. 4
in lactate production, leading to lactic aci-
Hb
dosis
Amount of haemoglobin in blood possibly 135 - 180g/L 7
OXYHAEMOGLOBIN
(Haemoglobin) capable of carrying oxygen.
Superior
DISSOCATION CURVE (ODC)
MIXED VENOUS Vena Cava What is it and why is it important?
The ODC looks at the relationship between oxygen tension (pressure)
BLOOD GAS VALUES Pulmonary
and oxygen saturation. It helps us better understand how our blood interacts
with oxygen, i.e. how and why it picks up and lets oxygen go.
Artery The S shape tells us that after an amount of oxygen has accumulated in
NAME VALUE the blood, there isnt room for any more, no matter how much oxygen you
pH 7.33 - 7.44 throw at the haemoglobin molecule, it wont change
HCO3- 24-28mmol/L Affinity basically means how much we (or blood) are attracted to
pCO2 41-57 mmhg someone (oxygen). The ODC shows us what changes the affinity of blood
paO2 35-40mmhg for oxygen.
sO2 70 - 75%
RIGHT SHIFT (ACIDOSIS)
Mixed venous gases measures oxygen left in the Shift of the curve to right decreases affinity - meaning that the Hb isnt
very attracted to oxygen, and when it does pick up oxygen, it lets it go very
blood as it returns to the heart (right side) after
quickly.
it has been pumped around the body supply- Increased temperature and CO2 help this right shift.
ing cells with oxygen.
The body normally extracts 25% of available LEFT SHIFT (ALKALOSIS)
Shift of the curve to the left increases affinity - meaning that the Hb is very
oxygen and leaves 75% in reserve in times of
attracted (oh la la) to oxygen and when oxygen is picked up, the Hb has a
stress or illness.4 hard time letting it go at the cellular level. Decreased temperature and CO2
help the curve move to the left. 2
The heart above shows where our subclavian central lines sits - in the superior vena cava, it is here we can take
venous blood gases. Samples from the pulmonary artery are however, more accurate and can only be performed
ALKALOSIS ACIDOSIS
if the patient has a PA catheter.
OTHER VALUES
OFTEN OVERLOOKED
Anion gap - This value is used in metablic acidosis to find the cause. It reflects unmeasured anions (negatively charged
ions) such as proteins, sulfates, phosphates etc. The equation to find the anion gap is (Na + K+) - (cl + [HCO3-])
a high value can be caused by keto or lactic acidosis, or renal failure. Low values may indicate hyponatremia or decreased
plasma protiens.
10-20mmol/L
OXYGEN STATUS Hb O2
O2 Hb
p50a - oxygen tension at 50% saturation on ODC. This is used to reflect affinity of Hb for oxygen.
25-29mmhg
FMetHb - This is the fraction of methaemoglobin. Think of methaemoglobin like haemoglobin, but we carry less than 1%
of it in our blood. As it is unable to combine with oxygen and it also decreases the oxygen carrying capacity of blood. Ex-
posure to certain drugs and chemicals can dangerously elevate levels.
0.2-0.6%
FCOHb - Fraction of carboxyhaemoglobin. Much similar to FMetHb in its actions. Affinity of Hb for carbon monoxide is BICARBONATE/CARBONIC (HCO3-/H2CO3) BUFFERING SYSTEM
200 times greater than that of oxygen and impairs oxygen transport and release (ODC shift to left, alkolosis). This level can This is the most active buffering system.
be high in heavy smokers. Needs good renal function (HCO3- regulation)
0.0-8.0% Converts H+ (hydrogen) to H2CO3 (carbonic acid) which is then able to be blown off via the lungs as CO2.
Fshunte - Relative physiological shunt. Basically the amount of venous (de-oxygenated) blood that did not receive oxygen
H2O + CO2 n H2CO3 nH+ + HCO3-
whilst travelling through the lungs. This can be caused by atelectasis, a pulmonary embolism (PE), mucous plugs and pul-
The H2O and CO2 is regulated via the lungs and HCO3- and H+ via the kidneys. An increase in one value can shift the
monary oedema, all of which reduces oxygen transport into the blood.
equation and helps maintain equilibrium.
1.0-10%
A problem in either the lungs or kidneys or both can throw this equation out of whack, resulting in an acid base imbalance.
FO2Hb - fraction of oxyhaemoglobin. This measures just how much blood (Hb) is carrying oxygen compared to the total
Other buffers include protein and phosphate buffers.
amount of Hb capable of carrying. Similar to your SO2, however FCOHb and FMetHb are not included as they are not ca-
pable of carrying oxygen.
94-98% RESPIRATORY REGULATION OF ACID BASE BALANCE
Eliminates volatile acids (CO2)
Hct - Hematocrit. This shows us how much red blood cells there are in a sample of blood - i.e. how watered down (or not) Works within minutes
blood is. 36-44%7 Dependent on HCO3- stores and adequate gas exchange
CO2 diffuses passively into the cerebrospinal fluid and the medulla controls rate and depth of respiration
REFERENCE LIST
1. Coleman, n. and Houston, L. 1998 Demystifying acid-base regulation Australian nursing Journal 5, 8, 23-26
2. Dickson, S. 1995 Understanding the Oxyhemoglobin Dissociation Curve. Critical care Nurse 15, 10, 54-58. RENAL REGULATION OF ACID BASE BALANCE
3. Minor, J. and George, E. 2008 Using mixed venous oxygen saturation to improve patient assessments. Nursing2008 56, 1, 1-3.
4. McCance, K. and Heuther, S. 1998 Pathophysiology, 3rd edn, Mosby, St. Louis, Missouri. Eliminates fixed acids (harder to remove than volatile) H+
Regulates HCO3- depending on need
5. Pruitt, W. 2004 Interpreting Arterial blood gases: Easy as ABC. Nursing2004 34, 2, 50-53.
6. Tastota, F. 1994 Assessing A.B.G.s: Maintaining the delicate balance. Nursing94 24, 5, 34-44.
7. The Blood Gas Handbook, 2005. Radiometer Medical ApS RadiometerCopenhagen, Bronshoj.
8. Wikipedia contributors, 2008 Pulmonary artery. n.p. Available URL: www.wikipedia.org/w/index.php?title=Pulmonary artery&oldid=183841779 <Accessed 2008 February 2> Controls phosphate and ammonia buffer systems
9. Wikipedia contributors, 2008 Oxygen-haemoglobin dissociation curve. n.p. Available URL: wikipedia.org/w/index.php?title=Oxygen-haemoglobin dissociation curve&oldid=187503438 <Accessed 2008 February 2>
Author: Amy ODonnell Date: 9th February, 2008 Bicarbonate/carbonic acid system can only work if bicarbonate stores are replaced by the kidneys.1
Works slowly, from hours to days
You might also like
- Abg Made EasyDocument24 pagesAbg Made EasynbvillarazoNo ratings yet
- Icu Nurse SheetDocument1 pageIcu Nurse SheetJan MarcusNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- ABG Interpretation - ATSDocument5 pagesABG Interpretation - ATSHAMMYER ALROKHAMINo ratings yet
- Arterial Blood Gas Analysis - making it easyFrom EverandArterial Blood Gas Analysis - making it easyRating: 4.5 out of 5 stars4.5/5 (4)
- ACAQ Crit Care Nursing CurriculumDocument91 pagesACAQ Crit Care Nursing CurriculumAnne Julia Agustin100% (1)
- Fluid and Electrolytes for Nursing StudentsFrom EverandFluid and Electrolytes for Nursing StudentsRating: 5 out of 5 stars5/5 (12)
- Cardiac Study GuideDocument9 pagesCardiac Study GuideJane DiazNo ratings yet
- Schaum's Outline of Critical Care Nursing: 250 Review QuestionsFrom EverandSchaum's Outline of Critical Care Nursing: 250 Review QuestionsRating: 5 out of 5 stars5/5 (1)
- ABG InterpretationDocument11 pagesABG InterpretationertrggerNo ratings yet
- Chapter (10) : Assessment of Cardiovascular SystemDocument10 pagesChapter (10) : Assessment of Cardiovascular SystemSandra GabasNo ratings yet
- EKG Basics1Document16 pagesEKG Basics1Jamie Lemons100% (1)
- Dosage Calculations PacketDocument39 pagesDosage Calculations PacketJack KeurigNo ratings yet
- Increased Intracranial Pressure and Monitoring Site PDFDocument21 pagesIncreased Intracranial Pressure and Monitoring Site PDFSari RakhmawatiNo ratings yet
- IV Solutions and Recommended UsageDocument11 pagesIV Solutions and Recommended Usageedver_19100% (10)
- Sample Acls For DummiesDocument3 pagesSample Acls For DummiesTodd Cole100% (1)
- Blood Gas InterpretationDocument36 pagesBlood Gas InterpretationMary Charmaine DivinagraciaNo ratings yet
- Arrythmia Name: Normal Sinus RhythmDocument7 pagesArrythmia Name: Normal Sinus RhythmJulx0No ratings yet
- ICU Cheat SheetDocument2 pagesICU Cheat SheetPrescilla Randazzo100% (1)
- Spotlight On Cardiac DrugsDocument2 pagesSpotlight On Cardiac Drugspauerish100% (2)
- ABG Reference GuideDocument1 pageABG Reference GuideUnclePorkchopNo ratings yet
- Cardiac Meds ChartDocument1 pageCardiac Meds ChartCharlotte Louise75% (4)
- CCRN-PCCN Review RenalDocument11 pagesCCRN-PCCN Review RenalGiovanni MictilNo ratings yet
- Reducing CLABSI Rates Through Proper Hand HygieneDocument1 pageReducing CLABSI Rates Through Proper Hand HygieneMomina ArshadNo ratings yet
- Critical Care Drug Reference SheetDocument12 pagesCritical Care Drug Reference SheetYanina CoxNo ratings yet
- Entire Medication BundleDocument22 pagesEntire Medication BundleKarina Castillo100% (1)
- Patient Assessment Marking SheetDocument2 pagesPatient Assessment Marking SheetJim Courtney100% (4)
- DYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDocument3 pagesDYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDarell M. Book100% (1)
- MAP, CO, and SV+HRDocument11 pagesMAP, CO, and SV+HRjenwiley318096% (73)
- MedicalSurgical Nursing ReviewDocument86 pagesMedicalSurgical Nursing ReviewPopa D. SilviuNo ratings yet
- 17 Cardiac DrugsDocument6 pages17 Cardiac DrugshiwaralelataNo ratings yet
- Pope, B. CCRN-PCCN-CMC Review Endocrine and BehavioralDocument14 pagesPope, B. CCRN-PCCN-CMC Review Endocrine and BehavioralKeisha JenkinsNo ratings yet
- Cardiac Med ChartsDocument6 pagesCardiac Med ChartsNursingSchoolNotes100% (15)
- Ecg Reading NotesDocument17 pagesEcg Reading NotesMarian FloresNo ratings yet
- Critical Care Note PDFDocument10 pagesCritical Care Note PDFlml100% (1)
- IV PDFDocument63 pagesIV PDFelbagouryNo ratings yet
- Quick Nursing Student Notes 2Document1 pageQuick Nursing Student Notes 2Frank KimNo ratings yet
- ABGs Respiratory/MetabolicDocument3 pagesABGs Respiratory/MetabolicJoe B100% (1)
- Acid-Base WorksheetDocument2 pagesAcid-Base WorksheetMayer Rosenberg100% (17)
- Vent Modes ChartDocument1 pageVent Modes Chartladyhavocinc100% (1)
- Hypertension Drugs and Pathophysiology ReviewDocument9 pagesHypertension Drugs and Pathophysiology ReviewChelsea SmithNo ratings yet
- Central Line Cheat SheetDocument1 pageCentral Line Cheat SheetLara Mae100% (1)
- Lab ValuesDocument3 pagesLab Valuessurviving nursing schoolNo ratings yet
- Pre - and Post Test Cardiac ArrhythmiasDocument6 pagesPre - and Post Test Cardiac ArrhythmiasEköw Santiago JavierNo ratings yet
- Practice StripsDocument9 pagesPractice StripsErica Yamamoto50% (4)
- Test InformationDocument5 pagesTest InformationCatalina BorquezNo ratings yet
- Invasive Hemodynamic Monitoring TechniquesDocument24 pagesInvasive Hemodynamic Monitoring Techniquesheyyymeee100% (3)
- Ekg Chart PDF 01Document5 pagesEkg Chart PDF 01YukiMaedaNo ratings yet
- Commonly Used Lab Values at A Glance Chem 7 1Document9 pagesCommonly Used Lab Values at A Glance Chem 7 1annatw100% (10)
- Cardiovascular DrugsDocument6 pagesCardiovascular Drugslhayes123488% (16)
- Anti-Infectives Course #25Document18 pagesAnti-Infectives Course #25Gina Giammalvo100% (2)
- BASIC ECG READING For Nle NOVEMBER 2018Document63 pagesBASIC ECG READING For Nle NOVEMBER 2018Sharmaine KimmayongNo ratings yet
- Labs 1.19 ABG AnalysisDocument1 pageLabs 1.19 ABG AnalysisMonica GonzalezNo ratings yet
- Cardiac Meds CompleteDocument3 pagesCardiac Meds CompleteDanielle100% (2)
- Obstetrics - Cardiovascular Disease in PregnancyDocument3 pagesObstetrics - Cardiovascular Disease in PregnancyJonathanNo ratings yet
- Nursing School EKGDocument43 pagesNursing School EKGRob Dickerson100% (1)
- Saudi Council for Health Specialties oversees Pediatric Surgery FellowshipDocument17 pagesSaudi Council for Health Specialties oversees Pediatric Surgery FellowshipmdbahaNo ratings yet
- Basic Computations 2 IV & IVFDocument37 pagesBasic Computations 2 IV & IVFCarl Elexer Cuyugan Ano100% (5)
- Dutch Euthanasics StudyDocument113 pagesDutch Euthanasics StudyAraceli Ecot CalunodNo ratings yet
- RE - RegistrationDocument4 pagesRE - RegistrationAraceli Ecot CalunodNo ratings yet
- Basic Computations 2 IV & IVFDocument37 pagesBasic Computations 2 IV & IVFCarl Elexer Cuyugan Ano100% (5)
- NIH Drug StemsDocument9 pagesNIH Drug StemsAraceli Ecot CalunodNo ratings yet
- BreechDocument1 pageBreechAraceli Ecot CalunodNo ratings yet
- AbgDocument7 pagesAbgAraceli Ecot CalunodNo ratings yet
- BreechDocument1 pageBreechZiyadNo ratings yet
- "Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Home VisitDocument3 pages"Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Home VisitCarl Elexer Cuyugan AnoNo ratings yet
- NLE ReviewerDocument246 pagesNLE Reviewerblazegomez99% (69)
- ABG Interpretation: Julie Perkins RRT-NPS LPCH Respiratory CareDocument14 pagesABG Interpretation: Julie Perkins RRT-NPS LPCH Respiratory CareTracy100% (4)
- Basic Computations 2 IV & IVFDocument37 pagesBasic Computations 2 IV & IVFCarl Elexer Cuyugan Ano100% (5)
- JHLDocument35 pagesJHLAraceli Ecot CalunodNo ratings yet
- Board Exam Test Taking StrategiesDocument53 pagesBoard Exam Test Taking StrategieskhaeydiancoNo ratings yet
- Abg PrimerDocument22 pagesAbg PrimerAraceli Ecot CalunodNo ratings yet
- Medical Surgical Nursing BulletsDocument143 pagesMedical Surgical Nursing BulletsJennye100% (3)
- Cranial Nerves FunctionsDocument6 pagesCranial Nerves FunctionsAraceli Ecot CalunodNo ratings yet
- Anatomy: Patellar Tendon TearDocument11 pagesAnatomy: Patellar Tendon TearrahadianpambudiNo ratings yet
- Ineffective Airway ClearanceDocument2 pagesIneffective Airway ClearanceMaria ArregoitiaNo ratings yet
- Cerebral PalsyDocument15 pagesCerebral Palsydxtyle-1No ratings yet
- Cardio PlusDocument3 pagesCardio Plusapi-3805007No ratings yet
- Etiology, Pathophysiology andDocument6 pagesEtiology, Pathophysiology andlatifa adluNo ratings yet
- Psychoanalytic Theory ExplainedDocument3 pagesPsychoanalytic Theory ExplainedHisabu MohammedNo ratings yet
- Causes and Mechanisms of Acute Renal Injury and Chronic Kidney DiseaseDocument12 pagesCauses and Mechanisms of Acute Renal Injury and Chronic Kidney DiseaseCres Padua QuinzonNo ratings yet
- Health - ALL ABT STRESSSSSSSSSDocument10 pagesHealth - ALL ABT STRESSSSSSSSSDennise Adrianne OfarilNo ratings yet
- Harry Best: The DeafDocument171 pagesHarry Best: The DeafGutenberg.org100% (1)
- SpirometryDocument63 pagesSpirometryAries DocNo ratings yet
- Neurology Tutorial Format: Neuro Anatomy & ExaminationDocument2 pagesNeurology Tutorial Format: Neuro Anatomy & Examinationsan MunNo ratings yet
- Abnormal Psych Notes 1Document4 pagesAbnormal Psych Notes 1ALYANAH DALE MAGNONo ratings yet
- AP Prefixes Suffixes Ebook 2016Document22 pagesAP Prefixes Suffixes Ebook 2016Jorge MarroneNo ratings yet
- Relationship Between Cigarette Smoking and Novel Risk Factors For Cardiovascular DiseaseDocument4 pagesRelationship Between Cigarette Smoking and Novel Risk Factors For Cardiovascular DiseaseInternational Medical PublisherNo ratings yet
- Ezolvin Syrup Patient Information Leaflet PDFDocument1 pageEzolvin Syrup Patient Information Leaflet PDFSameer SamouaNo ratings yet
- Neurological Rehabilitation and The Management of Spasticity - 2016 - MedicineDocument7 pagesNeurological Rehabilitation and The Management of Spasticity - 2016 - MedicinemateoNo ratings yet
- Asssessment Nursing Diagnosis Plan of Care Interventions Rationale EvaluationDocument5 pagesAsssessment Nursing Diagnosis Plan of Care Interventions Rationale EvaluationRoldan VidadNo ratings yet
- Chirurgie Pediatrica Engleza 125 Teste 2019 08.02.2019Document25 pagesChirurgie Pediatrica Engleza 125 Teste 2019 08.02.2019gm hashNo ratings yet
- Nutrition ManualDocument405 pagesNutrition ManualRaghavendra Prasad100% (1)
- Assessment of the Musculoskeletal SystemDocument35 pagesAssessment of the Musculoskeletal SystemChristine Joy MolinaNo ratings yet
- Persuasive Speech Outline CFDocument4 pagesPersuasive Speech Outline CFThanh Trần100% (1)
- Family Nursing Care Plan For FeverDocument2 pagesFamily Nursing Care Plan For Feverbharat singhNo ratings yet
- HIV AwarenessDocument35 pagesHIV AwarenessCadine DavisNo ratings yet
- Diseases of The Newborn Part2Document6 pagesDiseases of The Newborn Part2sarguss14100% (1)
- OaDocument6 pagesOafidatahir93No ratings yet
- Unit 2 Exercises GHIJKPDocument5 pagesUnit 2 Exercises GHIJKPAry OrtizNo ratings yet
- Hunger and AppetiteDocument20 pagesHunger and AppetiteAzeera RohimiNo ratings yet
- Is It True That GanodermaDocument2 pagesIs It True That GanodermaRohit SharmaNo ratings yet
- Toxicological Materia MedicaDocument104 pagesToxicological Materia Medicakayes82No ratings yet