Professional Documents
Culture Documents
Emergency I: I. Vomiting and Diarrhoea
Uploaded by
Keira IncognitusOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Emergency I: I. Vomiting and Diarrhoea
Uploaded by
Keira IncognitusCopyright:
Available Formats
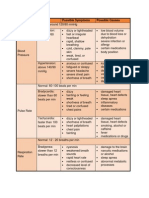
Lecture topic Lecture # 1st view Annotation Review Rereview
Emergency 1 2017-04-18 2017-04-18
Emergency I
I. Vomiting and diarrhoea
A. Differential diagnoses that need to be
excluded
1. Obstruction
- Intussusception
- Appendicitis
- hernia
2. infection
- UTI / meningitis / gastroenteritis
3. Metabolic conditions
- DKA
- HUS
4. Neurological
- Increased ICP?
B. History: to delineate the above DDx
- abdo pain / distension
- bile
- high fevers
- polydipsia, polyuria, wt loss
- headache - raised intracranial pressure
C. History/evaluation:
1. assessment of hydration
(a) fluids in:
- as a fraction of normal
(b) fluids out:
- wet nappies
- >8hours = red flag
- diarrhoea / vomiting
ii WHO dehydration scale
mild (5%)
- mild tachy, low urine o/p
moderate (7-9%)
- lethargy
- sunken eyes / fontanelle
- \/ skin turgor
severe (>10%)
- altered LOC
- signs of shock
D. Treatment
i mild dehydration
- frequent small volumes of fluids
- oral fluids!
- milk, gastrolyte.
- don't use orange juice (pulp causes vomiting)
- if not tolerated
- NG
- IV fluids
ii dystonic reaction
- prochloperazine, metoclopramide
- ondansetron is safest
- most common in <2 but can happen upto 11y.o.
therapy by age
baby (<12/12)
- anticholinergic antihistamine
- diazepam
infant (>1yr)
- Benztropine
II. Febrile child
- Points to rule out:
- bacteraemia?
- shock
- toxin: endo/exotoxaemia
A. diagnosis febrile convulsions
febrile convulsion
- 2-5% of kids
- family Hx
- not indicative of epilepsy (only 2-3% chance (double baseline) of developing epilepsy)
- do have /\ risk of recurrent febrile convulsions!
simple vs complex
- occur w/ fever
- fever may be apparent post seizure
- generalised
- whole body
- no focal activity
- brief (<5min)
- only 2-3h of post-ictal issues
- no residual neurological sequalae
complex if not the above
B. History
- irritable vs consolable
- localising symptoms
C. Evaluation – need to rule out bacteraemia
bacteraemia / sepsis: [NOT ALS APPROACH!]
(a) A - airway
(b) B - breathing
- effort
(c) C - circulatory impairment
- cap refil!!
- BP, hear rater
(d) D - disability
- AVPU
- P= GCS of 9
**no sign in isolation, absence of a sign doesn't exclude**
D. Treatment
1. bacteraemia
- t/f to hospital
i if meningococcal suspected:
- petichae = tiny areas of disseminated intravascular coagulation (DIC) in skin
- will grow - coalesce - pupura
(a) IM benzylpenicillin
- 300mg baby (<1yr)
- 600mg infant/child (1-9yrs)
- 1.2g 'adult' (includes child >10yrs)
(b) ceftriaxone
- 50mg/kg - up to 2g (for 'adults' or teens only)
(c) chemoprophylaxis for family:
- ceftriaxone / ciprofloxacin / rifampicin
You might also like
- IMCIDocument3 pagesIMCIwordlife360No ratings yet
- CC 13 Juli 2017 MeningoencephalitisDocument40 pagesCC 13 Juli 2017 MeningoencephalitisdelfiaNo ratings yet
- Acute Post Streptococcaالمحاضرة lDocument6 pagesAcute Post Streptococcaالمحاضرة lMGRNo ratings yet
- Dengue: Denv 2 Is The Most DangerousDocument5 pagesDengue: Denv 2 Is The Most DangerousNicole OrtegaNo ratings yet
- Paediatric Metabolic Emergencies Recognition, Investigations & ManagementDocument18 pagesPaediatric Metabolic Emergencies Recognition, Investigations & ManagementMalk OmryNo ratings yet
- Case Conference Friday Shift, June 30 2017Document49 pagesCase Conference Friday Shift, June 30 2017Izni AyuniNo ratings yet
- PEDIA Ear and ThroatDocument174 pagesPEDIA Ear and ThroatmatrixtrinityNo ratings yet
- WITH Notes - COMMUNICABLE DISEASE - PROF. ARCHIE ALVIZ - HANDOUTSDocument8 pagesWITH Notes - COMMUNICABLE DISEASE - PROF. ARCHIE ALVIZ - HANDOUTScammel ramosNo ratings yet
- FeverDocument29 pagesFeverYogesh KharcheNo ratings yet
- Malaria Prevention and TreatmentDocument20 pagesMalaria Prevention and TreatmentKamx MohammedNo ratings yet
- Agacnp 2Document124 pagesAgacnp 2academicexcellence21No ratings yet
- Dr. M. Hisham Pediatrics MCQ P.1: RespirationDocument12 pagesDr. M. Hisham Pediatrics MCQ P.1: Respirationعلي. احمد100% (1)
- Danger Signs in NewbornDocument8 pagesDanger Signs in NewbornPrabhu MagudeeswaranNo ratings yet
- Newborn Priorities in the First Day of LifeDocument8 pagesNewborn Priorities in the First Day of LifeMariecar GarazaNo ratings yet
- Approach To Common Medical SymptonsDocument46 pagesApproach To Common Medical SymptonsKoustav ChakrabortyNo ratings yet
- Paediatric Emergencies NotesDocument6 pagesPaediatric Emergencies NotesJana AldourNo ratings yet
- Case Conference Monday Morning Shift, October 8 2018Document34 pagesCase Conference Monday Morning Shift, October 8 2018latifahNo ratings yet
- Sga Lga Pre PosttermDocument41 pagesSga Lga Pre PosttermMaria Charis Anne IndananNo ratings yet
- Management Guidelines For Short Febrile Illness Including ILIDocument6 pagesManagement Guidelines For Short Febrile Illness Including ILIVenkata Nagaraj MummadisettyNo ratings yet
- Quiz LetDocument45 pagesQuiz LetA FishNo ratings yet
- USMLE High Yield Internal Medicine Notes-Part 2 2020Document19 pagesUSMLE High Yield Internal Medicine Notes-Part 2 2020usmlematerials.net0% (2)
- Infections - Eman AttaDocument7 pagesInfections - Eman AttaAhmed EhabNo ratings yet
- The Pediatrics HO GuideDocument44 pagesThe Pediatrics HO GuideAlex MatthewNo ratings yet
- Pediatric Nursing Common ProblemsDocument33 pagesPediatric Nursing Common ProblemsMaricel Agcaoili GallatoNo ratings yet
- Cardiovascular and Respiratory Nursing HandoutDocument8 pagesCardiovascular and Respiratory Nursing Handoutjon elleNo ratings yet
- CC 13 October 2017 (Demam Neutropenia) 2Document35 pagesCC 13 October 2017 (Demam Neutropenia) 2febrydwiNo ratings yet
- Fluid and Electrolyte TherapyDocument4 pagesFluid and Electrolyte TherapyKhirren RaoNo ratings yet
- Meningitis: O Highly Contagious People at RiskDocument3 pagesMeningitis: O Highly Contagious People at RiskJulx0No ratings yet
- Hydro Cep Hal UsDocument23 pagesHydro Cep Hal Usdhania patraNo ratings yet
- January 24 2006 TIME: 1hour Instructions To Candidates: Answer All Questions Answer Each Question in A Separate BookletDocument9 pagesJanuary 24 2006 TIME: 1hour Instructions To Candidates: Answer All Questions Answer Each Question in A Separate BookletAto Kwamena Sagoe100% (1)
- Peads - Diamond Blackfan AnemiaDocument40 pagesPeads - Diamond Blackfan AnemiaBaran PalanimuthuNo ratings yet
- Paediatrics NotesDocument111 pagesPaediatrics NotesShobhit Prasad100% (3)
- Pediatric Nursing Mukhtar AbobakerDocument4 pagesPediatric Nursing Mukhtar AbobakerAbo AmgadNo ratings yet
- Famco Important ChaptersDocument7 pagesFamco Important ChaptersFiryal BalushiNo ratings yet
- CC 2 Okt Hcu NeoDocument26 pagesCC 2 Okt Hcu NeolatifahNo ratings yet
- Pyogenic MeningitisDocument20 pagesPyogenic MeningitisClever BarbieNo ratings yet
- CC 22 Januari Gea AllDocument52 pagesCC 22 Januari Gea AlllatifahNo ratings yet
- Tetralogy of Fallot: Supervisor: Dr. Muhammad Ali, Sp.A (K) Presentator: Citra Aryanti 080100050 Marianto 080100112Document48 pagesTetralogy of Fallot: Supervisor: Dr. Muhammad Ali, Sp.A (K) Presentator: Citra Aryanti 080100050 Marianto 080100112Faskanita NadapdapNo ratings yet
- Case Report Serous MeningitisDocument39 pagesCase Report Serous MeningitismissyoanNo ratings yet
- Case Conference Sunday Night Shift, October 14 2018Document26 pagesCase Conference Sunday Night Shift, October 14 2018Hendra WardhanaNo ratings yet
- All Pediatrics 2Document200 pagesAll Pediatrics 2niemand daNo ratings yet
- EncephalitisDocument27 pagesEncephalitisHasRoni Fathurrahman100% (1)
- Pediatrics HESI Guide 2Document26 pagesPediatrics HESI Guide 2hellmanns1100% (15)
- Pediatric NursingDocument29 pagesPediatric NursingjeshemaNo ratings yet
- Meq PJPDocument19 pagesMeq PJPAtiqah ShahNo ratings yet
- Management of Organ Failure in Severe MalariaThe provided title "TITLE Management of Organ Failure in Severe MalariaDocument55 pagesManagement of Organ Failure in Severe MalariaThe provided title "TITLE Management of Organ Failure in Severe Malariastivana26No ratings yet
- Baca Dari PapdiDocument4 pagesBaca Dari PapdiAriane BeninaNo ratings yet
- MS - Endocrine SystemDocument11 pagesMS - Endocrine Systemknowamai567No ratings yet
- CC 8 Januari Gizi Buruk TSK HivDocument42 pagesCC 8 Januari Gizi Buruk TSK HivAisya FikritamaNo ratings yet
- CASE 1 pharmacotherapeuticsDocument14 pagesCASE 1 pharmacotherapeuticsOmair Mohammed 19No ratings yet
- Asuncion, Rachel Mae (Infectious Dse)Document3 pagesAsuncion, Rachel Mae (Infectious Dse)Rachel AsuncionNo ratings yet
- Written Output PRIME 3 - Cara, Mariel DanicaDocument3 pagesWritten Output PRIME 3 - Cara, Mariel DanicaMariel Danica CaraNo ratings yet
- CC 2 Mei 2017 PneumoniaDocument37 pagesCC 2 Mei 2017 PneumoniaAhimsa Yoga AninditaNo ratings yet
- Case Conference on Anemia PatientDocument35 pagesCase Conference on Anemia PatientAisya FikritamaNo ratings yet
- Top 10 leading causes of morbidity & mortality in the Philippines in 2007Document7 pagesTop 10 leading causes of morbidity & mortality in the Philippines in 2007Raisa Robelle Quicho100% (1)
- HY Mixed USMLE Review Part IIDocument22 pagesHY Mixed USMLE Review Part IIKiranNo ratings yet
- Nclex Questions - Pediatric NursingDocument8 pagesNclex Questions - Pediatric NursingAngelique Ramos PascuaNo ratings yet
- DCH - L2 - Child AbuseDocument10 pagesDCH - L2 - Child AbuseKeira IncognitusNo ratings yet
- DCH - L3 - DermatologyDocument1 pageDCH - L3 - DermatologyKeira IncognitusNo ratings yet
- Cultivation Guide For Temple Trees, Frangipani, Plumeria in Hawai'iDocument29 pagesCultivation Guide For Temple Trees, Frangipani, Plumeria in Hawai'iKeira IncognitusNo ratings yet
- Hsu He Profmed SalariesDocument24 pagesHsu He Profmed SalariesKhaled NagyNo ratings yet
- Star Chart - Southern Hemisphere - Mid November - Early EveningDocument1 pageStar Chart - Southern Hemisphere - Mid November - Early EveningKeira IncognitusNo ratings yet
- Sepsis Guidelines NICE PDFDocument1 pageSepsis Guidelines NICE PDFKeira IncognitusNo ratings yet
- Star Chart - Southern Hemisphere - Mid May - Early EveningDocument1 pageStar Chart - Southern Hemisphere - Mid May - Early EveningKeira IncognitusNo ratings yet
- 6-05 Migraine MechanismDocument1 page6-05 Migraine MechanismKeira IncognitusNo ratings yet
- PBL3 - Acid Fast BacilliDocument1 pagePBL3 - Acid Fast BacilliKeira IncognitusNo ratings yet
- Nursing Care Plan of The NewbornDocument4 pagesNursing Care Plan of The Newbornbowki namoNo ratings yet
- Hypertension Session Student ObjectivesDocument2 pagesHypertension Session Student ObjectivesAyman NabilNo ratings yet
- Marquis Et Al 2023 CT Approach To Lung InjuryDocument19 pagesMarquis Et Al 2023 CT Approach To Lung InjuryMinh đăng ĐỗNo ratings yet
- Neuropsychiatry of Headache PDFDocument185 pagesNeuropsychiatry of Headache PDFGuillermo GonzalezNo ratings yet
- Daftar PustakaDocument4 pagesDaftar PustakaRohmantuah_Tra_1826No ratings yet
- A Rare Case of Vanishing Lung SyndromeDocument3 pagesA Rare Case of Vanishing Lung SyndromeMUH. RAKIB YUNUSNo ratings yet
- Micro-Needling Consultation & Consent FormDocument8 pagesMicro-Needling Consultation & Consent FormVivi AnaNo ratings yet
- Class-10 English Communicative Paper Full Syllabus (2023-2024)Document6 pagesClass-10 English Communicative Paper Full Syllabus (2023-2024)makolsaima16060No ratings yet
- Epidemiology - COVID-19RebeccacgDocument10 pagesEpidemiology - COVID-19RebeccacgIheakachi IheakachiNo ratings yet
- Community DentistryDocument5 pagesCommunity DentistryDenis BaftijariNo ratings yet
- Eyeng SaryamDocument13 pagesEyeng Saryamrode sihombingNo ratings yet
- Vital Signs Assessment TableDocument2 pagesVital Signs Assessment Tableapi-250869701No ratings yet
- Toms River Regional School District Athletic Waiver and Release of Liability Form Related To COVID-19Document4 pagesToms River Regional School District Athletic Waiver and Release of Liability Form Related To COVID-19Asbury Park PressNo ratings yet
- Coma-Causes, Diagnosis, Treatment and ManagementDocument19 pagesComa-Causes, Diagnosis, Treatment and ManagementHabtamu AdimasuNo ratings yet
- APhA - The Pharmacy Technician, 4th EditionDocument51 pagesAPhA - The Pharmacy Technician, 4th EditionLina TasamaNo ratings yet
- CCSP GuidelinesDocument42 pagesCCSP GuidelinesAzhagendranNo ratings yet
- Child Health Nsg.Document2 pagesChild Health Nsg.YAMINIPRIYANNo ratings yet
- Epstein-Barr Virus and MonoDocument2 pagesEpstein-Barr Virus and MonoMihai PetrescuNo ratings yet
- Covid GuidelinesDocument1 pageCovid Guidelinesapi-509452068No ratings yet
- Dr. Dhani Redhono Hariosaputro, SP - PD-KPTI - Invasive Fungal Infection in SepsisDocument32 pagesDr. Dhani Redhono Hariosaputro, SP - PD-KPTI - Invasive Fungal Infection in SepsisOlivia DwimaswastiNo ratings yet
- RESNICK - Bone and Joint Imaging, 3rd Ed. CONTENIDODocument3 pagesRESNICK - Bone and Joint Imaging, 3rd Ed. CONTENIDOfabianNo ratings yet
- COVID-19 Vaccination Certificate from India's Ministry of HealthDocument1 pageCOVID-19 Vaccination Certificate from India's Ministry of HealthBEST COMPUTERSNo ratings yet
- Travelers DiarrheaDocument23 pagesTravelers Diarrheakakang chuNo ratings yet
- Nephrotic SyndromeDocument28 pagesNephrotic Syndromerupali khillareNo ratings yet
- Necrotizing FasciitisDocument5 pagesNecrotizing Fasciitisnsl1225No ratings yet
- SKRINING Dan Penerapannya Pada Proses Skrining ISPA Pasien Balita Di Daerah Banjarbaru PPT English VersionDocument11 pagesSKRINING Dan Penerapannya Pada Proses Skrining ISPA Pasien Balita Di Daerah Banjarbaru PPT English VersionYulia Afrina NstNo ratings yet
- Revised-Chapter 6 Case Study BDocument2 pagesRevised-Chapter 6 Case Study BAngelica PerezNo ratings yet
- IntroductionDocument10 pagesIntroductionNareman Alaa50% (2)
- MyChart - Test DetailsDocument2 pagesMyChart - Test DetailsMaría RepettoNo ratings yet
- Structures and Functions of the SkinDocument33 pagesStructures and Functions of the SkinVas LillaNo ratings yet