Professional Documents
Culture Documents
1
Uploaded by
Delia StaricaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1
Uploaded by
Delia StaricaCopyright:
Available Formats
Transfer of Advances in Sciences into Dental Education
Bone Scintigraphy as an Adjunct for
the Diagnosis of Oral Diseases
Rívea Inês Ferreira, D.D.S., M.Sc.; Solange Maria de Almeida, D.D.S., Ph.D.;
Frab Norberto Bóscolo, D.D.S., Ph.D.; Allan Oliveira Santos, M.D.;
Edwaldo E. Camargo, M.D., Ph.D.
Abstract: Bone scintigraphy is a very sensitive method for the detection of osteoblastic activity of the skeleton. The technique
consists of imaging the uptake of bone-seeking radiopharmaceuticals, particularly technetium-99m labeled diphosphonates, in the
mineral component of bone, which consists of hydroxyapatite crystals and calcium phosphate, as well as in the organic matrix
such as collagen fibers. Plain radiographs, computed tomography, and magnetic resonance imaging are classified as structural
imaging modalities, whereas bone scintigraphy is a functional method. In many cases, radionuclide imaging techniques are the
only means by which early physiologic changes that are a direct result of biochemical alteration may be assessed, before signifi-
cant bone mineral changes can be detected by other means. Since many oral diseases may cause metabolic changes in the
oromaxillofacial complex, it would be of great value to use bone scintigraphy to evaluate more completely some conditions
involving the bones in the region to formulate more appropriate treatment plans. Based upon the current literature, the authors
discuss the possible applications of bone scintigraphy as a diagnostic and treatment planning adjunct for oral diseases. Bone
scintigraphy has proven particularly useful in the study of malignant lesions and in the evaluation of vascularized bone grafts used
for maxillofacial reconstructions.
Dr. Ferreira is a Ph.D. student, Department of Oral Diagnosis, Division of Oral and Maxillofacial Radiology, Piracicaba School of
Dentistry; Dr. Almeida is Assistant Professor, Department of Oral Diagnosis, Division of Oral and Maxillofacial Radiology,
Piracicaba School of Dentistry; Dr. Bóscolo is Professor and Chairman, Department of Oral Diagnosis, Division of Oral and
Maxillofacial Radiology, Piracicaba School of Dentistry; Dr. Santos is Nuclear Physician, Department of Radiology, Division of
Nuclear Medicine, School of Medical Sciences; and Dr. Camargo is Professor and Chairman, Department of Radiology, Division
of Nuclear Medicine, School of Medical Sciences—all at the State University of Campinas, São Paulo, Brazil. Direct correspon-
dence and requests for reprints to Dr. Rivea I. Ferreira, Área de Radiologia – FOP/UNICAMP, Av. Limeira, 901, Areião –
Piracicaba/SP, São Paulo, Brazil 13.414-903; (55 19) 3251-2334 phone/fax; riveaines@yahoo.com.
Key words: bone scintigraphy, oral diseases, radionuclides, dentistry
Submitted for publication 4/23/02; accepted 9/30/02
undetected until the development of physical symp-
C
onventional and digital radiographs remain
toms, the early diagnosis of a variety of jaw lesions
the most available tool for the detection of
is difficult. Conversely, bone scans have the ability
some conditions affecting teeth and bones of
to show reactive modifications in osteoblastic activ-
the oral cavity. Radiographic examinations display
ity that would not appear on radiographic images,
differences in density within an anatomic region and
but do not show morphologic changes. Although its
produce images of relatively high resolution. How-
resolution is not as high as that of radiographs, bone
ever, in view of the fact that conventional radiologic
scintigraphy may be positive if there is, approxi-
techniques demonstrate bony changes when there has
mately, a 10 percent increase in the osteoblastic ac-
been an alteration of 30 to 50 percent of the bone
tivity above normal.2 In many clinical conditions,
mineral content, determination of the extent of some
bone scintigraphy will demonstrate abnormalities
bony lesions by radiologic means alone may become
long before the radiographs. In other situations, it
somewhat erroneous.1 Thus, the x-ray imaging de-
may demonstrate abnormal changes that may rein-
pendence on differential absorption essentially lim-
force a questionable radiographic finding. It may also
its this modality to the tissue electron density, which
help to determine the metabolic activity within a bone
in turn is presented as structural or anatomic changes.
lesion or at its margins.
Since morphological alterations may simply be later
Scintigraphic images are obtained utilizing the
effects of a biochemical process that has remained
intravenous administration of a radiopharmaceutical,
December 2002 ■ Journal of Dental Education 1381
particularly technetium-99m labeled diphosphonates. nations are frequently performed to evaluate trauma,
Technetium-99m have a physical short half-life of inflammatory disease, and primary bone tumors.
six hours, 140keV gamma energy, and the radionu- SPECT studies entail acquiring rotating delayed static
clide-labeled tracers are used in quantities whose images, generally sixty-four projections over 360º,
emitted radiation doses are far below the amounts followed by computer reconstruction to provide three-
that are toxic to human cells.3 The bone-imaging dimensional multiplanar slices in the axial, coronal,
agents circulate through the bloodstream until they and sagittal planes, relative to the patient’s body.
are either incorporated into sites of active bone turn- Because of the complex three-dimensional anatomy
over or are excreted in the urine.3 The mechanism with extensive overlap of bony structures, the facial
whereby labeled phosphonates are incorporated into bones and base of the skull may be difficult to evalu-
bone is not well understood. Our knowledge of the ate with planar bone scan images. In terms of SPECT
mechanisms of deposition of the diphosphonates is applications, for instance, temporomandibular joints’
still incomplete. Phosphate compounds are thought internal derangement could be investigated by means
to adsorb to the amorphous bone. In an in vitro bind- of SPECT images.
ing assay, the competitive adsorption of technetium- Bone is an extraordinarily dynamic tissue. Con-
99m labeled diphosphonates to pure hydroxyapatite stant turnover in response to metabolic or mechani-
is forty times greater than to pure organic bone ma- cal demands results in a steady state between new
trix. Thus, its uptake correlates well with the rate of bone formation and resorption. Radionuclide bone
mineralization.4 scanning takes advantage of this constant physiologic
Image acquisition involves a computed scintil- activity. Most morbid processes involving bone re-
lation camera that records the gamma rays emitted sult in increased turnover or new bone formation.6
by the patient. The camera has a scintillation crystal Scintigraphically, areas of increased bone metabo-
that fluoresces at the time of interaction with the lism are evidenced and appear as areas of increased
gamma rays. This fluorescence is detected by photo- radiotracer uptake, namely “hot spots.” Decreased
multiplier tubes, which transform the flashes of light uptake is associated with metabolically inactive bone,
into electronic signals to produce an image that is lack of osteogenesis, or an absent vascular supply.
displayed on a computer monitor. With regard to the role of bone turnover in the dis-
According to Eggli and Tulchinsky,5 there are ease process, scintigraphic findings of decreased
a number of ways to perform a bone scan study. The uptake indicate lack of reparative response and sug-
method chosen is typically influenced by the clinical gest the presence of a highly aggressive lesion.7 Zones
diagnosis to be evaluated. Bone-imaging techniques of photon-deficient or photopenic abnormalities,
include, basically, standard bone scan (whole-body where there is diminished or absent uptake, are called
scanning or whole-body spot views), three-phase “cold spots.”6
bone scan, and single photon emission computed Despite the relatively low specificity, previous
tomography (SPECT). Standard bone scans involve studies have shown that bone scintigraphy has the
the acquisition of static images three hours after tracer potential to provide valuable information concerning
administration. Delayed static images may be useful the diagnosis and follow-up of several oral conditions
in the evaluation of benign conditions, such as condy- such as: primary or metastatic malignancies, benign
lar hyperplasia. Three-phase study comprises a flow neoplasms, cystic lesions, inflammatory and infectious
assessment, a blood pool image, and delayed static processes, metabolic diseases, fibro-osseous dyspla-
views acquisition. The dynamic flow study requires sias, hyperplasias, and bone graft viability.1,7-14
rapid sequential images for sixty seconds during the
intravenous administration of the radiotracer. This is
followed by a blood pool image reflecting tissue hy-
peremia and is acquired immediately after the flow
Primary and Metastatic
study. Three hours after radiotracer administration, Malignancies
the bony uptake of technetium-99m labeled
diphosphonates is maximal, and a significant pro- It is well known that the maxilla and mandible
portion of the unbound tracer will have been excreted are possible sites for the development of malignant
by the kidneys. Therefore, the final delayed static neoplasms, which, on the basis of histological fea-
images are acquired at this time. Three-phase exami- tures, are broadly classified into carcinomas and sar-
1382 Journal of Dental Education ■ Volume 66, No. 12
account for less than 1 percent of the overall inci-
dence of bone metastases.15 Nevertheless, bone me-
tastases to the oral cavity account for approximately
90 percent of all oral metastatic lesions.15 More than
70 percent of these occur in the mandible, usually in
the molar-premolar regions, where the greatest
amount of bone marrow is located.15,16 Adenocarci-
nomas of the breast, prostate, thyroid gland, lung,
kidney, uterus, colon, and stomach are the primary
tumors most frequently metastasizing to the maxil-
lofacial region.15-18
Söderholm et al.19 reported that the periosteum
has been thought to form a barrier against cancerous
invasion of the mandibular bone. However, mandibu-
lar bone involvement may occur at an early stage
through small defects in the bony cortex of the al-
veolar process. Since the gingiva is only a few milli-
Figure 1. Anterior, posterior, and right and left lateral
views, showing an area of intense uptake in the left
meters thick, even a tiny lesion may rapidly spread
maxilla that corresponds to an osteosarcoma to the bone.
Considering that malignant tumors in the oral
comas. Carcinomas found in the jaw may have origi- cavity are less common than at other sites in the body
nated from lesions of the oral mucosa, arise from and the patient’s signs and symptoms may be con-
epithelial residues in the jaw, develop by malignant fused with those related to benign lesions such as
transformation of a benign lesion, such as a cyst or odontogenic tumors, the early diagnosis of carcino-
an ameloblastoma, or be metastatic deposits from mas and sarcomas of the jaw often poses clinical
primary tumors in distant sites. On the other hand, challenges. Indeed, the definitive method to diagnose
the great majority of sarcomas are recognized as malignant neoplasms is histopathologic examination.
malignant lesions arising from the mesenchymal tis- However, the
However, the superior sensitivity
sensitivity of bone scintigra-
sue components of the jaw. phy in providing valuable information for preopera-
Oral malignant neoplasms represent approxi- tive assessment of the malignant lesions’ extent has
mately 5 percent of all malignant neoplasms in the been reported by many authors.11,13,15-20
body.15 One to 8 percent are considered to be due to The most frequently encountered scintigraphic
metastases.16 Because of the scarcity of bone mar- pattern in malignant bone lesions is that of one or
row in the maxilla and mandible, lesions in the jaw multiple randomly distributed foci of intensely in-
Figure 2. The oblique view suggests that the osteosarcoma, illustrated in Figure 1, has extended to the maxillary
tuberosity
December 2002 ■ Journal of Dental Education 1383
creased radiotracer uptake, the so-called “hot spots” eases may be identified if the nuclear physicians are
(Figures 1 and 2). aware of this possibility and request appropriate den-
tal examination for the affected patients.
The usefulness of the bone scan as a diagnos-
Inflammatory and Infectious tic aid for inflammatory responses of the temporo-
mandibular joints (TMJ) is somewhat controver-
Processes sial.2,11,21 However, attempts have been made to
improve the evaluation of the metabolic and physi-
Inflammation represents a dynamic process that ological status of TMJ bony structures. In fact, bone
takes place in the connective tissue as a reaction to scans may demonstrate inflammatory reactions that
intrinsic and/or extrinsic agents. Accordingly, some take place in TMJ bony structures, as illustrated in
oral conditions such as osteomyelitis, traumatic inju- Figure 4. Pogrel et al.22 designed a prospective study
ries, osteoarthritis, periapical lesions, and periodontal to compare single-photon emission computed tomog-
disease play an important role in bone metabolism and raphy (SPECT) imaging with lateral planar images
result in a positive bone scan image. Figure 3 illus- for quantitative assessment of pathologic processes
trates the features of an acute osteomyelitis, as dem- of the mandibular condyle. These authors not only
onstrated by an intense technetium-99m labeled highlighted the efficiency of the SPECT technique,
diphosphonate uptake in the right posterior maxillary but also suggested that it could replace planar im-
region, that developed following a tooth extraction. ages. SPECT bone scanning offers both enhanced
Diagnostic approaches of pulpo-periapical dis- image contrast resolution and more accurate local-
eases usually are based on the patient’s symptoms ization of active disease as it provides three-dimen-
and mainly on clinical and radiographic findings, sional information, allowing the interpreters to visu-
rather than on bone scan imaging. Nevertheless, bone alize in transaxial, coronal, and sagittal slices,
scintigraphy may disclose periapical lesions because structures that would overlap on planar views.
the radionuclide uptake may precede radiographic Bouquot and LaMarche23 undertook a retro-
alterations by months. Baumgartner and Eggli10 re- spective investigation of some processes that they
ported the detection of a periapical lesion of endo- diagnosed as ischemic osteonecrosis in patients with
dontic origin in the mandible during a routine bone histories of endodontic treatment, tooth extraction,
scan used as a follow-up to cancer therapy. Matteson or fixed partial denture pontics in areas of idiopathic
et al.8 explained that some undiscovered dental dis- pain. According to these authors, ischemic osteone-
crosis, which is the result of a wide variety of local
and systemic disorders that eventually lead to is-
chemia and infarction of the cancellous bone, is of-
ten undiagnosed due to the high proportion of false-
negative radiographic images. On the other hand,
bone scans may reveal occult abnormalities as “hot
spot” areas in the subpontic bone.23
Fibro-Osseous Dysplasias
Fibrous dysplasias of the jaw are believed to
be benign, self-limiting, but non-encapsulated, le-
sions occurring mainly in young subjects. Histologi-
cally, they are characterized by the replacement of
normal bone by a cellular fibro-osseous tissue con-
taining islands or trabeculae of metaplastic bone.
Although jawbone fibrous dysplasias are usually
Figure 3. Anterior, posterior, and right and left lateral monostotic lesions, they may occasionally be part of
images, showing increased uptake of technetium-99m a polyostotic process.24 Enlargement of the lesions is
labeled diphosphonate, which reflects the activity of slow and insidious and persists until cessation of
an infectious process
1384 Journal of Dental Education ■ Volume 66, No. 12
ht and
Figure 4. Right and left
left lateral
lateral views
views showing
showing an
an area
area of
of intense
intense uptake
uptake in
in the
the left TMJ, in
left TMJ, in a
a patient
patient with
with degenerative
degenerative
joint disease
growth, even n though in some cases it may continue and, thus, helping to avoid a loss of surrounding
od. The treatment of choice is conserva-
into adulthood. bone from graft necrosis or infection. It is espe-
tive osseous contouring by surgery, and its goal for cially useful in reconstruction of the jaw that usu-
ns should be correction of esthetic and
larger lesions ally involves a vascularized bone autograft, because
roblems.24
functional problems. 24 clinical monitoring of the transplanted bone is dif-
graphs are usually adequate for the diag-
Radiographs ficult. Kärcher et al.99 reported their experience with
ver, bone scintigraphy is often useful to
nosis; however, the use of three-phase bone scintigraphy in assess-
establish the extent and activity of maxillofacial le- ing the post-operative viability of seven vascular-
ure 5 shows a planar image of an adult
sions.11 Figure ized bone grafts. According to these authors, in all
patient for whom surgical treatment was considered. successful cases, a positive bone scan correlated
ossible to determine if growth of the le-
It was not possible with a viable bone graft.
graft. Two negative exams, show-
ased, and thus the patient was referred
sion had ceased,
for a nuclear medicine bone scan. The focal “hot spot”
in the right mandibular body demonstrated that the
till metabolically active.
lesion was still
Bone Graft Viability
integrated implants are now accepted as
Osseointegrated
a modality treatment to replace missing teeth for
of
easing segment of the population. The
an ever-increasing
his kind of rehabilitation relies on the
success of this
quality and amount of remaining osseous tissue. It is
sometimes necessary to apply bone grafts to ensure
adequate bone ne support for the implants. Bone grafts
ployed to replace parts of the jaw com-
are also employed
promised by y problems such as periodontal disease,
trauma, tumor or infiltration, cystic lesions, serious in-
fections, or congenital defects
defects.
11 Figure 5. Anterior view showing a focal area of
Harbert mentioned that bone scintigraphy
increased uptake localized to the right mandible body,
provides a means of predicting graft failure before which demonstrates that the fibrous dysplasia still has
radiographic or clinical changes become apparent an active growth pattern
December 2002 ■ Journal of Dental Education 1385
ing photopenic defects, corresponded to nonviable ing perspective, detection of skeletal physiology is
grafts that had to be removed. the greatest strength of bone scintigraphy.
Recently, Schimming et al.14 discussed the use Bone scintigraphy is a physiologic method,
of computer-aided three-dimensional reconstruction which is more sensitive than radiography. In terms
of SPECT images in the assessment of vascularized of diagnostic approach, the major disadvantage of
bone grafts, in the early post-operative period and bone scintigraphy, in relation to radiography, is its
approximately two weeks after surgery. The authors nonspecificity. It is reasonable to assume, therefore,
stated that modern-day SPECT scanning of the head that an integrated approach of correlating the results
and neck area, including computer-aided three-di- of both procedures might reduce the individual limi-
mensional SPECT reconstruction, is useful to evalu- tations of each.
ate microvascular success or failure and that com- Carrera and Collier Jr.6 explained that all diag-
puter-aided three-dimensional SPECT reconstruction nostic tests, including imaging modalities, serve three
adds significantly to the value of planar bone scin- fundamental purposes in evaluating bone diseases:
tigraphy and conventional SPECT images, particu- detection, characterization, and staging. Structural
larly because it allows a better description of the bone imaging modalities such as radiography, CT, and MRI
graft, since it provides images with even higher con- should be used in conjunction with bone scintigra-
trast, without any superimposing effects.14 However, phy, which shows modifications in the osteoblastic
because of bone remodeling immediately after sur- activity. A good example is the diagnosis of condy-
gery, it is not a completely reliable method for the lar hyperplasia, on the basis of radiographic exami-
early assessment of microvascular patency in vascu- nation, in patients having facial asymmetry with de-
larized bone grafts. viation of the mandible. One goal of TMJ
scintigraphy is to, in fact, determine whether bone
growth has ceased prior to treatment. Patients with
Discussion equal uptake on the right and the left sides show no
further progression of the asymmetry and may un-
Although a variety of health care profession- dergo treatment.25
als may provide a multitude of diagnostic and thera- Scintigraphic bone studies may be important
peutic services, the dentist undertakes the responsi- in determining the extent of some benign lesions such
bility of ordering the appropriate treatment for the as odontogenic keratocyst, ameloblastoma, and od-
oral diseases or referring the patient to another spe- ontogenic myxoma.1,7 With respect to the malignant
cialist. Therefore, dentists should have a basic knowl- neoplasms, these entities usually display an elevated
edge of the principles of diagnostic imaging modali- radionuclide uptake, and the disease process may ex-
ties and possible clinical applications. tend considerably beyond the zone of visible bone
Routinely, after a comprehensive case history destruction shown on the radiographs. Thus, bone scin-
and clinical examination, dentists prescribe radiog- tigraphy may be useful in justifying larger resections
raphy. To investigate diseases related to the teeth and in order to achieve complete excision and avoid re-
maxillofacial bones, radiographs are currently more currence.7 According to Meidan et al.,26 bone scan-
available and less expensive than bone scintigraphy ning is also a valuable test in the follow-up of peri-
and patients are more willing to undergo radiogra- implant bone tissue. But a relatively less expensive
phy than scintigraphy. On the other hand, bone scin- and invasive method, digital subtraction radiography
tigraphy is of proven value as an additional diagnos- (DSR), has also proven reliable in assessing dental
tic tool in radiographic examinations of skeletal implants osseointegration.27 Specifically in this case,
disorders. Each imaging modality provides its own in our opinion, bone scan should not be indicated.
specific information. Imaging studies such as radi- In conclusion, dentists should be aware that,
ography, computed tomography (CT), magnetic reso- similar to other imaging methods, bone scintigraphy
nance imaging (MRI), and ultrasound (US) serve to has its advantages and disadvantages and may some-
display both normal and morbid anatomy and physi- times fail in completely solving a diagnostic prob-
ology.6 This is important because a fundamental part lem. For a proper diagnostic approach and follow-
of classic clinical evaluation and many forms of treat- up, morphologic and physiologic imaging modalities,
ment also rely on anatomic localization and charac- in combination, should support each other in offer-
terization of diseases. From a multimodality imag-
1386 Journal of Dental Education ■ Volume 66, No. 12
ing valuable information in the diagnosis of maxil- 14. Schimming R, Juengling FD, Lauer G, et al. Evaluation of
lofacial jaw bone lesions. microvascular bone graft reconstruction of the head and
neck with 3-D 99mTc-DPD SPECT scans. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod 2000;90:679-85.
15. Stavropoulos MF, Ord RA. Lobular adenocarcinoma of
REFERENCES breast metastatic to the mandibular condyle. Oral Surg
1. Lurie AG, Puri S, James RB, et al. Radionuclide bone Oral Med Oral Pathol 1993;75:575-8.
imaging in the surgical treatment planning of odontoge- 16. Aniceto GS, Peñín AG, Pages RM, et al. Tumors meta-
nic keratocysts. Oral Surg Oral Med Oral Pathol static to the mandible: analysis of nine cases and review
1976;42:726-30. of the literature. J Oral Maxillofac Surg 1990;48:246-51.
2. Craemer TD, Ficara AJ. The value of the nuclear medical 17. Carmichael FA, Mitchell DA, Dyson DP. Case report: two
scan in the diagnosis of temporomandibular joint disease. contrasting radiological presentations of prostatic adeno-
Oral Surg Oral Med Oral Pathol 1984;58:382-5. carcinoma in the jaws. Dentomaxillofac Radiol 1996;25:
3. Subramanian G. Radiopharmaceuticals for bone scanning. 283-6.
In: Collier Jr BD, Fogelman I, Rosenthall L, eds. Skeletal 18. Glaser C, Lang S, Pruckmayer M, et al. Clinical manifes-
nuclear medicine. St. Louis: Mosby, 1996:9-20. tations and diagnostic approach to metastatic cancer of
4. Francis MD, Horn PA, Tofe AJ. Controversial mechanism the mandible. Int J Oral Maxillofac Surg 1997;26:365-8.
of technetium-99m deposition on bone. J Nucl Med 19. Söderholm AL, Lindqvist C, Hietanen J, et al. Bone scan-
1981;22:72. ning for evaluating mandibular bone extension of oral
5. Eggli DF, Tulchinsky M. Normal planar bone scan. In: squamous cell carcinoma. J Oral Maxillofac Surg
Collier Jr BD, Fogelman I, Rosenthall L, eds. Skeletal 1990;48:252-7.
nuclear medicine. St. Louis: Mosby, 1996:23-44. 20. Ventä I, Oikarinen VJ, Söderholm AL, et al. Third molars
6. Carrera GF, Collier Jr BD. A multi-modality approach to confusing the diagnosis of carcinoma. Oral Surg Oral Med
bone imaging. In: Collier Jr BD, Fogelman I, Rosenthall Oral Pathol 1993;75:551-5.
L, eds. Skeletal nuclear medicine. St. Louis: Mosby, 21. Harris SA, Rood JP, Testa HJ. Post-traumatic changes of
1996:73-84. the temporo-mandibular joint by bone scintigraphy. Int J
7. Josell SD, Reiskin AB, Gross BD. Dentigerous cyst with Oral Maxillofac Surg 1988;17:173-6.
mural ameloblastoma. J Am Dent Assoc 1979;99:634-6. 22. Pogrel MA, Kopf J, Dodson TB, et al. A comparison of
8. Matteson SR, Staab EV, Fine JT. Bone-scan appearance single-photon emission computed tomography and pla-
of benign oral pathologic conditions. J Oral Surg nar imaging for quantitative skeletal scintigraphy of the
1980;38:759-63. mandibular condyle. Oral Surg Oral Med Oral Pathol Oral
9. Kärcher H, Füger G, Borbely L. Bone scintigraphy of Radiol Endod 1995;80:226-31.
vascularized bone transfer in maxillofacial surgery. Oral 23. Bouquot JE, LaMarche MG. Ischemic osteonecrosis un-
Surg Oral Med Oral Pathol 1988;65:519-22. der fixed partial denture pontics: radiographic and mi-
10. Baumgartner JC, Eggli D. The use of bone imaging to croscopic features in 38 patients with chronic pain. J
detect a periapical lesion of endodontic origin. J Endod Prosthet Dent 1999;81:148-58.
1989;15:493-5. 24. Langlais RP, Langland OE, Nortjé CJ, eds. Diagnostic
11. Harbert JC. The musculoeskeletal system. In: Harbert JC, imaging of the jaws. Philadelphia: Williams & Wilkins,
Eckelman WC, Newmann RD, eds. Nuclear medicine: 1995:565-615.
diagnosis and therapy. New York: Thieme, 1996:801-63. 25. Cisneros GJ, Kaban LB. Computerized skeletal scintig-
12. Frederiksen NL. Specialized radiographic techniques. In: raphy for assessment of mandibular asymmetry. J Oral
White SC, Pharoah MJ, eds. Oral radiology: principles Maxillofac Surg 1984;42:513-20.
and interpretation. St. Louis: Mosby, 1999:217-40. 26. Meidan Z, Weisman S, Baron J, et al. Technetium 99m-
13. Schimming R, Juengling FD, Lauer G, et al. Computer- MDP scintigraphy of patients undergoing implant pros-
aided 3-D 99mTc-DPD-SPECT reconstruction to assess thetic procedures: a follow-up study. J Periodontol
mandibular invasion by intraoral squamous cell carci- 1994;65:330-5.
noma: diagnostic improvement or not? J Craniomaxillofac 27. Brägger U. Use of radiographs in evaluating success, sta-
Surg 2000;28:325-30. bility and failure in implant dentistry. Periodontol 2000
1998;17:77-88.
December 2002 ■ Journal of Dental Education 1387
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- InfluenzaDocument11 pagesInfluenzayara mariwanNo ratings yet
- Essential Intrapartum and Newborn CareDocument25 pagesEssential Intrapartum and Newborn CareMaria Lovelyn LumaynoNo ratings yet
- Kettle Bell Workout MovesDocument1 pageKettle Bell Workout MovesRabiatul AdawiyahNo ratings yet
- DRR11 12 Ic D 34Document3 pagesDRR11 12 Ic D 34allanrnmanalotoNo ratings yet
- Inspiring Leaders April 2023Document54 pagesInspiring Leaders April 2023Jay MenonNo ratings yet
- Job Satisfaction of Employees in Multispecialty Hospitals in Delhi and NCRDocument11 pagesJob Satisfaction of Employees in Multispecialty Hospitals in Delhi and NCRVenkatram PrabhuNo ratings yet
- METHOD STATEMENT Sluice Gates InstallDocument9 pagesMETHOD STATEMENT Sluice Gates Installjameel100% (2)
- The 14 IDEA Disability Categories DefinedDocument7 pagesThe 14 IDEA Disability Categories DefinedRico Bautista SongSongCoupleNo ratings yet
- Usp 40 1229.2 Moist Heat Sterilization of Aqueous LiquidsDocument6 pagesUsp 40 1229.2 Moist Heat Sterilization of Aqueous LiquidsJHON ALEXANDER BEDOYA BUILES100% (1)
- Psypysch Group One ActivityDocument15 pagesPsypysch Group One ActivityShannon Erika Drew A. EdañoNo ratings yet
- Pharmacology of Drugs Acting On Renal SystemDocument20 pagesPharmacology of Drugs Acting On Renal SystemBestha Chakri100% (2)
- Major Assignment #1 Revise Rough DraftDocument4 pagesMajor Assignment #1 Revise Rough DraftIsaac TafoyaNo ratings yet
- Paralegal Training on IDP RightsDocument2 pagesParalegal Training on IDP RightsMc Vharn CatreNo ratings yet
- Elc590: English For Oral Presentations: Resource Materials 3: Monroe's Motivated SequenceDocument22 pagesElc590: English For Oral Presentations: Resource Materials 3: Monroe's Motivated Sequencesarah adrianaNo ratings yet
- Colonialism and Development Final Version-1Document29 pagesColonialism and Development Final Version-1salma AkhtarNo ratings yet
- CH Components of Food AssignmentDocument3 pagesCH Components of Food AssignmentRuma GhoshNo ratings yet
- Solution Manual For Dosage Calculations A Multi Method Approach 0132158620Document13 pagesSolution Manual For Dosage Calculations A Multi Method Approach 0132158620RandallValdezypfqw100% (86)
- Cooking MEALlenials’ Korean Spam Fried Rice Feasibility StudyDocument153 pagesCooking MEALlenials’ Korean Spam Fried Rice Feasibility StudyJinella CastanedaNo ratings yet
- Maimonides Medical Center - 2021-2022Document1 pageMaimonides Medical Center - 2021-2022sal palNo ratings yet
- CDC Clear Communication Index: User GuideDocument36 pagesCDC Clear Communication Index: User GuideJesse ManekNo ratings yet
- ESADocument31 pagesESAssourabNo ratings yet
- Q2 2023 Embassy Suites by Hilton Fact SheetDocument2 pagesQ2 2023 Embassy Suites by Hilton Fact SheetcraZyFFNo ratings yet
- True and False FoodsDocument3 pagesTrue and False FoodsCheree (Cherry) SeoNo ratings yet
- Mastering The Art in Dental ImpressionsDocument13 pagesMastering The Art in Dental ImpressionsJuán A. Nina Leon100% (1)
- Health BrochureDocument2 pagesHealth BrochureMaryanne Rose Pado ElderNo ratings yet
- Physio Personal Statement 2Document1 pagePhysio Personal Statement 2YB chiu100% (1)
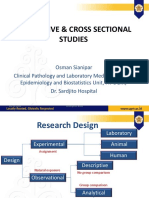
- Lecture 5 Research Design Observational Studies (Descriptive and Cross Sectional) - Dr. Dr. Osman Sianipar, DMM., MSC., Sp. PK (K) (2022)Document49 pagesLecture 5 Research Design Observational Studies (Descriptive and Cross Sectional) - Dr. Dr. Osman Sianipar, DMM., MSC., Sp. PK (K) (2022)Sheila Tirta AyumurtiNo ratings yet
- General Laboratory Safety TrainingDocument33 pagesGeneral Laboratory Safety TrainingLouis Fetilo FabunanNo ratings yet
- Chogtu 2015Document7 pagesChogtu 2015Maskur Fahmi ÄdibasNo ratings yet
- MSDS Acrylite Acrylic SheetDocument6 pagesMSDS Acrylite Acrylic SheetMateusPauloNo ratings yet