Professional Documents
Culture Documents
Article Wjpps 1498803742
Uploaded by
Farah MawazirOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Article Wjpps 1498803742
Uploaded by
Farah MawazirCopyright:
Available Formats
WORLD JOURNAL OF PHARMACY AND PHARMACEUTICAL SCIENCES
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
SJIF Impact Factor 6.647
Volume 6, Issue 7, 239-260 Review Article ISSN 2278 – 4357
DIABETIC FOOT ULCER: A REVIEW
*Vishwas A.T.L.1, Dr. Bhanushree D. M.2, Chethan B.2, Vinutha M. D.3 Prashanthi B.3,
Nandan H. N.4
Department of Pharmacy Practice, Bharathi College of Pharmacy, Bharathi Nagara, Mandya.
Article Received on ABSTRACT
24 April 2017, Diabetic foot problems are common throughout the world, resulting in
Revised on 14 May 2017,
Accepted on 03 June 2017
major medical, social and economic consequences for the patients,
DOI:10.20959/wjpps20177-9446 their families and society. Foot ulcers affect 15% of diabetic patients
during their lifetime. Foot ulcers are more likely to be of neuropathic
*Corresponding Author’ origin and therefore eminently preventable. Infected diabetic foot
Vishwas A.T.L. ulcers are a major cause of hospitalization in diabetic patients and most
Department of Pharmacy non-traumatic amputations are associated with diabetic foot infections.
Practice, Bharathi College of
The most commonly used classification systems are the Wagner-Ulcer
Pharmacy, Bharathi Nagara,
Mandya.
Classification system and the University of Texas Wound
Classification. The management of diabetic foot ulcer (DFU) should be
optimized by using a multidisciplinary team, due to a holistic approach to wound
management is required. Based on studies, blood sugar control, wound debridement,
advanced dressings and offloading modalities should always be a part of DFU management.
Treatment of chronic wounds should be essentially directed against the main etiologic factors
responsible for the wound. Amputations are usually the treatment of last resort but
occasionally can be considered early to allow for faster mobilization and rehabilitation. This
article will focus the causes, pathogenesis and recommended management pathways of
diabetic foot ulcers.
KEYWORDS: Diabetes mellitus, Amputation, Neuropathic, Debridement, Etiology.
INTRODUCTION
Diabetes mellitus (DM) is one of the main problems in health systems and a global public
health threat that has increased dramatically over the past two decades.[1] In India
approximately 61.2 million people are diabetic and it is expected to increase to 101.2 million
www.wjpps.com Vol 6, Issue 7, 2017. 239
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
by 2030.[2] In addition, people with T2DM are often accompanied by complications, such as
cardiovascular diseases, diabetic neuropathy, nephropathy, and retinopathy.[3]
Foot ulcers are the most common medical complications of patients with diabetes, with an
estimated prevalence of 12-15% among all individuals with diabetes.[4] The term ―Diabetic
foot ulcer‖ is used to define a clinical condition, but simply put it is merely a wound on the
foot of a patient who is diabetic.[5] Diabetic foot ulcers are responsible for more
hospitalizations than any other complication of diabetes. Ulcerations can have potential
devastating complications as they cause up to 90% of lower extremity amputations in patients
with diabetes.[4]
Infection in foot wounds should be defined clinically by the presence of inflammation or
purulence, and then classified by severity. This approach helps clinicians make decisions
about which patients to hospitalize or to send for imaging procedures or for whom to
recommend surgical interventions. Many organisms, alone or in combinations, can cause
DFI, but gram-positive cocci (GPC), especially staphylococci, are the most common.[6]
Diabetic foot complications are the most common cause of non-traumatic lower extremity
amputations in the industrialized world.[7] They are complex infections and the prognosis is
influenced by many factors, depending on the ulcer (location, extension, whether chronic or
not, previous amputation, ischemia grade), and the patient (age, renal impairment, time of
onset of diabetes, associated co-morbidity). All these must be taken into account when
establishing its treatment.[8]
EPIDEMIOLOGY
Globally, diabetic foot infections are the most common skeletal and soft-tissue infections in
patients with diabetes. The incidence of diabetic foot infections is similar to that of diabetes
in various ethnic groups and most frequently affect elderly patients. There are no significant
differences between the sexes. Mortality is not common, except in unusual circumstances.[9]
Even today, seven out of top ten countries with the largest number of diabetes patients are
low or Middle - income countries, including India, China, Russia, Brazil, Pakistan, Indonesia,
and Bangladesh among which the prevalence rates are 12.1% and 9.7% in India and China,
respectively.[41] The annual incidence of foot ulceration is estimated to be approximately 1% -
4% and its prevalence ranges from 4% to 10%, whereas, the lifetime risk for the development
of a diabetic foot ulcer in patients with diabetes ranges from 15% to as high as 25%.[10]
www.wjpps.com Vol 6, Issue 7, 2017. 240
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
Although the costs derived from DF ulcers and other infections are not accurately known, in
the U.S. it is estimated that an ulcer episode costs from $4,500 to $28,000 at two years after
diagnosis, with a mean of $5,500 per patient per year. Although mean hospital stay of an
amputation has decreased, it remains a costly procedure, ranging from $20,000 to $40,000
depending on the level of amputation, hospital stay, or patient co-morbidities. More up-to-
date and similarly high values are available for Europe.[8]
A National Rural Diabetes Survey was done between 1989 and 1991 in different parts of the
Indian‘s rural populations which showed diabetic prevalence as 2.8 per cent. The prevalence
of 6.1 percent in individuals aged above 40 years was unexpectedly high at that time for rural
area with low socio-economic status and decreased health awareness.[11]
ETIOLOGY OF DIABETIC FOOT ULCER
In most patients, peripheral neuropathy and peripheral arterial disease (PAD) (or both) play a
central role and DFUs are therefore commonly classified as (Table 1).
a) Neuropathic
b) Ischaemic
c) Neuroischaemic ( Figures 1-3)[12]
Table 1: Typical features of DFUs according to etiology[13]
Feature Neuropathic Ischaemic Neuroischaemic
Reduced or absent Sensation may be
Sensation sensation to touch, present but decreased Degree of sensory
vibration, pain, and if there is associated loss
pressure neuropathy
Cold or decreased
Foot temperature Warm Cool
temperature
On the plantar aspects Distal/tips of the toes,
Margins of the
Ulcer location (forefoot 80%) of the heel, or margins of the
foot and toes
foot/toes foot
Present and often
Absent or markedly Cool with absent
Foot pulses bounding. Dilated,
reduced pulses
prominent veins
Commonly seen on the Not usually. If
Minimal callus
Callus present weight-bearing areas present, distal eschar
Prone to necrosis
and is generally thick or necrosis
Dry skin and High risk of
Other Delayed healing
fissuring Infection
www.wjpps.com Vol 6, Issue 7, 2017. 241
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
Figure 1: Neuropathic DFU Figure 2: Ischaemic DFU Figure 3: Neuroischaemic DFU
SITES OF AND CAUSES OF DIABETIC FOOT ULCERS
The site of ulcer, etiology and treatment methodology varies according to the population of
different region. Several reported that several factors were contributing to the outcome of
DFU, which is irrespective of similar type of care treatment.[11] Diabetic foot ulcers usually
develop in areas of the foot that are exposed to either friction and sustained pressure, and/ or
areas of the foot that are exposed to repetitive trauma e.g. rubbing of toes on the stitching of a
shoe. The most common foot ulcer sites are.
• The heel
• On the underside of the toes
• The tips of any prominent toes (usually the 1st or 2nd toe)
• The tips of deformed toes (e.g. tips of hammer toes).[5]
PATHOGENESIS OF DIABETIC FOOT ULCER
DFU is characterized by a classical triad of neuropathy, ischemia, and infection. Due to the
impaired metabolic mechanisms in DM, there is an increased risk of infection and poor
wound healing due to a series of mechanisms which include decreased cell and growth factor
response, diminished peripheral blood flow and decreased local angiogenesis. Thus, the feet
are predisposed to peripheral vascular disease, damage of peripheral nerves, deformities,
ulcerations and gangrene (Figure 5).[14]
a) Neuropathy
Peripheral neuropathy in diabetes is one of the major causes of foot ulcers. Studies reported
that metabolic abnormalities due to hyperglycemia cause neuropathy. There are various other
factors accounting for origination of neuropathy, like pre-diabetes neuropathy, abnormalities
in fatty acid metabolism, activation of protein kinase-C pathway, formation of advanced
glycated end products, myoinisitol, polyol pathway, production of nerve growth factor and
production of antibodies to neural tissues. The four prime mechanisms causing
hyperglycemic nerve damage are elevated levels of intracellular advanced glycated end
www.wjpps.com Vol 6, Issue 7, 2017. 242
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
products, activation of protein kinase C, increased hexosamine pathway flux and polyol
pathway.[15]
Peripheral neuropathy may predispose the foot to ulceration through its effects on the
sensory, motor and autonomic nerves.
The loss of protective sensation experienced by patients with sensory neuropathy renders
them vulnerable to physical, chemical and thermal trauma.
Motor neuropathy can cause foot deformities (such as hammer toes and claw foot), which
may result in abnormal pressures over bony prominences.
Autonomic neuropathy is typically associated with dry skin, which can result in fissures,
cracking and callus. Another feature is bounding pulses, which is often misinterpreted as
indicating a good circulation.
Loss of protective sensation is a major component of nearly all DFUs. It is associated with a
seven–fold increase in risk of ulceration.[12]
b) Peripheral vascular disease
Peripheral vascular disease (PVD) is an atherosclerotic occlusive disease of lower extremity.
Diabetes is an important risk factor for PVD. PVD is an important prejudiced cause towards
development of foot ulcers in about 50% of cases. Patients with diabetes have a higher
incidence of atherosclerosis, thickening of basement membranes of capillaries, hardening of
arteriolar walls and endothelial proliferation. Atherosclerotic blockage of large and medium-
sized arteries, such as femoropopliteal and aortoiliac vessels leads to acute or chronic
ischemia.[15] Atherogenesis is the developmental process of atheromatous plaques. It is
characterized by a remodeling of arteries leading to subendothelial accumulation of fatty
substances called plaques.[11] In combination with digital artery disease, ulcers can develop
and instantaneously progress to gangrene due to inadequate blood flow. Decreased arterial
perfusion causes abate in peripheral pulses and patient comes to a risk of ulceration, infection
with impaired healing rates and finally leading to chronic state involving gangrene and
amputation.[15] It is important to remember that even in the absence of a poor arterial supply,
microangiopathy (small vessel dysfunction) contributes to poor ulcer healing in
neuroischaemic DFUs.[12] DM is associated with a near 3-fold increased risk of accelerated
atherosclerosis, which is histologically identical to that seen in the non-diabetic population.
This underlines the importance of identifying and aggressively managing associated vascular
www.wjpps.com Vol 6, Issue 7, 2017. 243
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
risk factors, such as obesity, cigarette smoking, dyslipidemia, hypertension, and sedentary
behavior.[16]
c) Neuroarthropathy
Charcot neuroarthropathy (CN) is a chronic painless progressive degenerative arthropathy
resulting from the disturbance in sensory innervations of the affected joint. The impairment
of the autonomic nervous system due to DM causes an increase in local blood supply and the
resting blood flow is much higher than in the normal patient. The sudden increase in blood
flow causes calcium to dissolve, leading to osteoclastic activity of the bone and thus
damaging the bone. Another theory is that the repetitive minor trauma to the insensate joints
leads to fracture and disintegration.[14] In peripheral blood monocytes isolated from Charcot
patients, the osteoclast formation was significant increased compared to diabetic patients and
healthy controls. The osteoclastic resorption increased after addition of receptor activator of
RANKL) via release
of proinflammatory cytokines as TNF-alfa. Central role in this process of local inflammation
is trauma. Trauma will induce pro-inflammatory cytokines like TNF-alfa and RANKL will be
expressed. Due to loss in pain perception by the distal neuropathy, the TNF-alfa release will
persist and the RANKL pathway is persistently stimulated (Figure 4).[17]
www.wjpps.com Vol 6, Issue 7, 2017. 244
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
Figure 4: Diabetic neuroarthropathy, or Charcot foot, is believed to be a neurologically-
mediated complication of diabetes, with the development modified by musculoskeletal
stress. The result is osseous fragmentation and joint subluxation with often significant
morphologic changes in the architecture of the foot.[18]
d) Infection
Once the protective layer of skin is broken, the deep tissues are exposed to bacterial coloni-
zation.
Staphylococcus aureus and ß-hemolytic streptococci are the first microorganisms to colonize
and acutely infect breaks in the skin. Chronic wounds develop more complex polymicrobial
microbiology, including aerobic Gram-negative rods and anaerobes. Anaerobes are rarely the
sole pathogen, but they often participate in a mixed infection with aerobes, especially in cases
of deep tissue infection. These mixed infections provide an optimal opportunity for microbial
synergy, which increases the net pathogenic effect and hence the severity of infection.
www.wjpps.com Vol 6, Issue 7, 2017. 245
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
Accordingly, the composition of the polymicrobial wound flora is likely to be more important
than the presence of specific pathogens.[16]
e) Other risk factors
Recent studies have indicated multiple risk factors associated with the development of DFU.
These risk factors are as follows: gender (male), duration of diabetes longer than 10 years,
advanced age of patients, high Body Mass Index, and other co-morbidities such as
retinopathy, glycated hemoglobin level (HbA1C), foot deformity, high plantar pressure and
inappropriate foot self-care habits.[1]
Figure 5: Diabetic foot ulcer (DFU) pathophysiology. DFU results from a complex
interaction of a number of risk factors.[16]
CLASSIFICATION OF DIABETIC FOOT
There is no one universally accepted classification system. Most systems employ a matrix of
grades based upon depth and size of wound.[8] There are three main diabetic foot
classification system are discussed that are commonly used in clinical diagnosis of diabetic
foot.[11]
www.wjpps.com Vol 6, Issue 7, 2017. 246
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
These were
a) Wagner-Meggitt Classification
b) Depth-Ischemic classification
c) University of Texas classification
Wagner Meggitt Classification
One of the oldest well-known classifications was proposed by Wagner and Meggitt in the
1970s. This classification is most commonly known as the ―Wagner Classification‖ in the
United States and its uses six grades in classifying diabetic foot lesions.[7] This system is
basically anatomical with gradations of superficial ulcer, deep ulcer, abscess osteitis,
gangrene of the fore foot, and gangrene of the entire foot. Only grade 3 addresses the problem
of infection. In this system foot lesions are divided into different grades starting from grade 0
to grade 5. Grade 0 includes high risk foot but no active lesion and grade 5 includes gangrene
of entire foot. But this system does not mention about ischemia or neuropathy and that is the
drawback of this system (Table 2).[11]
Table 2: Wagner-Meggitt Classification System.
Grade Lesion
Grade0 No open Lesion
Grade1 Superficial ulcer
Grade2 Deep ulcer to tendon or joint capsule
Grade3 Deep ulcer with abscess, osteomyelitis, or joint sepsis
Grade4 Local gangrene- fore foot or heel
Grade5 Gangrene of entire foot
Texas Classification
A more recently proposed and popularized DFU classification is the University of Texas
Health Science Center San Antonio (UT) classification system. This system incorporates a
matrix structure of four grades of wound depth with subgroups to denote the presence of
infection, ischemia or both. Wounds with frank purulence and/or two or more local signs of
inflammation such as warmth, erythema, lymphangitis, lymphadenopathy, edema, pain and
loss of function may be classified as ‗infected.‘ Lower extremity vascular insufficiency is
made by a combination of one or more clinical signs or symptoms of claudication, rest-pain,
absent pulses, dependent rubor, atrophic integument, absence of pedal hair or pallor on
elevation coupled with one of more non-invasive values such as a transcutaneous oxygen
(TCPO2) <40 mmHg, ankle brachial index (ABI) <0.8 or absolute toe systolic pressure <45
mmHg (Table 3).[19]
www.wjpps.com Vol 6, Issue 7, 2017. 247
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
Table 3: Texas Classification.
Grade 0 Grade 1 Grade 2 Grade 3
Preulcerative or Superficial wound Wound Wound
postulcerative not involving penetrating penetrating
Stage 1
lesions completely tendon, capsule or tendon or to bone or
epithelialized bone capsule joint
Stage 2 Infection Infection Infection Infection
Stage 3 Ischaemia Ischaemia Ischaemia Ischaemia
Infection and Infection and Infection and Infection and
Stage 4
Ischaemia Ischaemia Ischaemia Ischaemia
Depth-Ischemic Classification
This classification is a modification of Wagner–Meggit system. The purpose of this
classification system is to make the classification more accurate, balanced and easier to
distinguish between wound and vascularity of foot, to elucidate the difference among the
grades 2 and 3, and to advance the correlation of treatment to the grade (Table 4).[15]
Table 4: Depth-Ischemic Classification.
Depth Ischemia
Definition Definition
Grade Grade
At risk, foot with previous ulcer
0 A No ischemia
that may cause new ulcer
1 Superficial non-infected ulcer B Ischemia no gangrene
Deep ulcer with tendon or joint
2 C Partial forefoot gangrene
exposed (+/ _ infection)
Extensive ulcer with bone
3 D Total foot gangrene
exposed or deep abscess
DIAGNOSIS OF DIABETIC FOOT ULCER
Patients with a DFU should be assessed by the team within one working day of presentation
or sooner in the presence of severe infection. Patients with a DFU need to be assessed
holistically to identify intrinsic and extrinsic factors. This should encompass a full patient
history including medication, co-morbidities and diabetes status.[20] It should also take into
consideration the history of the wound, previous DFUs or amputations and any symptoms
suggestive of neuropathy or peripheral arterial disease.[12]
a) History and Physical examination
First, the physician enquire patient about their symptoms and will examine them. This
examination should include the patient's vital signs (temperature, pulse, blood pressure, and
respiratory rate), examination of the sensation in the feet and legs, an examination of the
circulation in the feet and legs, a thorough examination of any problem areas.[9] A thorough
www.wjpps.com Vol 6, Issue 7, 2017. 248
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
medical and foot history must be obtained from the patient. The history should address
several specific diabetic foot issues (Table 5).[18]
Medical History
Foot Specific History
Global History
General Wound / ulcer history
Location
Duration
Diabetes-duration
Inciting event or trauma
Glycemic
Recurrence
management/control Daily activities
Infection
Cardiovascular, renal and Footwear
Hospitalization
ophthalmic evaluations Chemical exposures
Wound care
Other co-morbidities Callus formation
Off- loading techniques
Treating physicians Previous foot
Wound response
Nutritional status infections, surgery
Patient compliance
Alcohol, tobacco and Neuropathic
drugs Interference with wound care
symptoms
(family or social problems for
Current medications Claudication or rest
patient)
Allergies pain
Previous foot trauma or surgery
Previous hospitalizations/
Presence of edema
surgery
Charcot foot- previous or active
Charcot treatment
b) X-rays
X-rays studies of the feet or legs were performed to assess for signs of damage to the bones
or arthritis, damage from infection, foreign bodies in the soft tissues. Gas in the soft tissues,
indicates gangrene - a very serious, potentially life-threatening or limb-threatening
infection.[9]
c) Examination of ulcer
A sterile stainless steel probe is used for assessing the ulcer to determine the depth and if
there is sinus tracts present. The location, size, shape, depth, base and margins of the ulcer
should be examined clinically. Presence of granulation tissue or slough should be looked for
in the floor of the ulcer to determine subsequent management. Diagnosing a soft tissue
infection in patient with diabetes is sometimes difficult, as the signs of inflammation of the
overlying ulcer may be absent. The infection is mainly diagnosed based on presence of
clinical signs and symptoms such as redness, warmth, tenderness, purulent secretions and
fever. Palpation of the bone at the base of the ulcer with a sterile, blunt stainless steel probe
has been suggested as positive predictor of underlying osteomyelitis.[14]
www.wjpps.com Vol 6, Issue 7, 2017. 249
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
d) Neurological testing
Peripheral neuropathy is the most common component cause in the pathway to diabetic foot
ulceration. The clinical exam recommended, however, is designed to identify loss of
protective sensation (LOPS) rather than early neuropathy. Five simple clinical tests (Table 6)
each with evidence from well conducted prospective clinical cohort studies are considered
useful in the diagnosis of LOPS in the diabetic foot. The task force agrees that any of the five
tests listed could be used by clinicians to identify LOPS, although ideally two of these should
be regularly performed during the screening exam-normally the 10-g monofilament and one
other test. One or more abnormal tests would suggest LOPS, while at least two normal tests
(and no abnormal test) would rule out LOPS. However, identification of the patient with
LOPS can easily be carried out without Biothesiometer or other expensive equipment.[21]
Table 6: Simple bed side clinical tests.
SI. NO Clinical Tests
1 10-g monofilaments
2 Pinprick sensation
3 Ankle reflexes
4 Tuning fork test
5 Vibration perception threshold testing
e) Ultrasound
Doppler ultrasound to see the blood flow through the arteries and veins in the lower
extremities. The test is not painful and involves the technician moving a non-invasive probe
over the blood vessels of the lower extremities.[9]
f) Laboratory investigations
Clinical laboratory tests that may be needed in appropriate clinical situations include fasting
or random blood glucose, glycohemoglobin (HbA1c), complete blood count (CBC) with or
without differential, erythrocyte sedimentation rate (ESR), serum chemistries, C-reactive
protein, alkaline phosphatase, wound and blood cultures and urinalysis. Caution must be
exercised in the interpretation of laboratory tests in these patients, because several reports
have documented the absence of leukocytosis in the presence of severe foot infections. A
common sign of persistent infection is recalcitrant hyperglycemia despite usual anti
hyperglycemic regimens.[18]
www.wjpps.com Vol 6, Issue 7, 2017. 250
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
g) Angiogram
If the vascular surgeon determines that the patient has poor circulation in the lower
extremities, an angiogram may be performed in preparation for surgery to improve
circulation. With an angiogram, a catheter is inserted through the artery in the groin and dye
is injected while x-rays are taken.[9]
DIABETIC FOOT INFECTIONS
Foot infections in persons with diabetes are an increasingly common problem and are
associated with potentially serious sequelae. The continued rise in incidence of diabetes in
developed, and to an even greater degree in many lesser-developed, countries, the increasing
body weight of many diabetic patients and their greater longevity all contribute to the growth
of this problem.[6] Foot infections are common in patients with diabetes and are associated
with high morbidity and risk of lower extremity amputation. Diabetic foot infections are
classified as mild, moderate, or severe. Gram-positive bacteria, such as Staphylococcus
aureus and beta-hemolytic streptococci, are the most common pathogens in previously
untreated mild and moderate infection. Severe, chronic, or previously treated infections are
often polymicrobial.[22] All infections begin as a slight problem may progress to involve deep
tissues, joints or bones especially if not managed. The infection complicates the pathological
depiction of diabetic foot. Study on diabetic foot ulcers reported that the presence of infection
increase the risk of a lower extremity amputation by 50% compared to ulcer patients without
infection. Around 60% of infected foot ulcers are headed by loss of lower limb, and becomes
one of the most awful outcomes in diabetic foot patients.[15]
ETIOLOGY OF DIABETIC FOOT INFECTIONS
The microorganisms involved in the etiology of DF infection vary depending on the type of
infection and specific patient situations.[8]
Etiology of diabetic foot infections.
Infection Microorganisms
Cellulitis Staphylococcus aureus
Erysipelas Beta-hemolytic streptococci (A, B, C and G)
Staphylococcus aureus
Ulcer untreated with antibiotics
Beta-hemolytic streptococci (A, B, C and G)
Staphylococcus aureus
Methicillin-resistant Staphylococcus aureus
Ulcer treated with antibiotics or
Coagulase-negative staphylococci
long-term (generally polymicrobial)
Streptococcus spp.
Enterococcus spp.
www.wjpps.com Vol 6, Issue 7, 2017. 251
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
Enterobacteriaceae
Pseudomonas aeruginosa1
Other nonfermenting gram-negative bacilli2
Corynebacterium spp.2
Candida spp.2
Anaerobic gram-positive cocci
Necrotizing fascitis or
Enterobacteriaceae
myonecrosis (generally
Nonfermenting gram-negative bacilli
polymicrobial)
Anaerobes
PATHOPHYSIOLOGY OF DIABETIC FOOT INFECTIONS
Several factors predispose diabetic patients to developing a DFI, including neuropathy,
vasculopathy and immunopathy. Peripheral neuropathy occurs early in the pathogenesis of
diabetic foot complications and is considered the most prominent risk factor for diabetic foot
ulcers8. Patients with diabetes lose the protective sensations for temperature and pain,
impairing awareness of trauma such as abrasions, blistering, or penetrating foreign body.
Motor neuropathy can result in foot deformities (e.g., claw toe) that contribute to local
pressure from footwear, making skin ulceration even more likely. Once the skin is broken
(typically on the plantar surface), the underlying tissues are exposed to colonization by
pathogenic organisms. The resulting wound infection may begin superficially, but with delay
in treatment and impaired body defense mechanisms caused by neutrophil dysfunction and
vascular insufficiency, it can spread to the contiguous subcutaneous tissues and to even
deeper structures.[22]
MICROBIOLOGY
Various aspects of wound microbiology are responsible for development of foot infection.
These include microbial load, diversity of microbes, existence of infective organisms and
synergistic association amongst microbial species. Infection is said to occur when microbial
load is greater than 105 organisms per gram of tissue.[15] The most common pathogens in
acute, previously untreated, superficial infected foot wounds in patients with diabetes are
aerobic gram-positive bacteria, particularly Staphylococcus aureus and beta-hemolytic
streptococci (group A, B, and others). Infection in patients who have recently received
antibiotics or who have deep limb-threatening infection or chronic wounds are usually caused
by a mixture of aerobic gram-positive, aerobic gram-negative (e.g., Escherichia coli, Proteus
species, Klebsiella species), and anaerobic organisms (e.g., Bacteroides species, Clostridium
species, Peptococcus and Peptostreptococcus species). Anaerobic bacteria are usually part of
mixed infections in patients with foot ischemia or gangrene. Methicillin-resistant
www.wjpps.com Vol 6, Issue 7, 2017. 252
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
Staphylococcus aureus (MRSA) is a more common pathogen in patients who have been
previously hospitalized or who have recently received antibiotic therapy. MRSA infection
can also occur in the absence of risk factors because of the increasing prevalence of MRSA in
the community.[22]
INFECTION CONTROL
The selection of antibiotic therapy for diabetic foot infection involves decisions about choice
of empiric and definitive antibiotic agent, route of administration, and duration of treatment.
Initial empiric antibiotic therapy should be based on the severity of the infection, history of
recent antibiotic treatment, previous infection with resistant organisms, recent culture results,
current Gram stain findings, and patient factors (e.g., drug allergy).[22] Select specific
antibiotic agents for treatment based on the likely or proven causative pathogens, their
antibiotic susceptibilities, the clinical severity of the infection, and evidence of efficacy for
DFI and costs. A course of antibiotic therapy of 1-2 weeks is usually adequate for most soft
tissue diabetic foot infections.[23]
Antimicrobial preparations used in chronic wound care include topical antiseptics, topical
antibacterials, and systemic antibiotics, all recently reviewed. Many preparations described in
these reviews can effectively control bacterial growth; however, they can be toxic for host
tissues. Currently, there is no conclusive evidence that one antibiotic or antiseptic is superior
to any other achieving efficient elimination of infection and decreasing time to healing.[24]
Mild to moderate infections with localized cellulitis can be treated on an outpatient basis with
oral antibiotics such as cephalexin, amoxicillin with clavulanate potassium, moxifloxacin, or
clindamycin. The antibiotics should be started after initial cultures are taken and changed as
necessary.[25]
PREVENTION OF DIABETIC FOOT ULCERS
Prevention of diabetic foot ulcers begins with identifying patients at risk.[22] Primary
prevention is the aim of diabetes management, but secondary prevention is the goal of
effective foot ulcer care. The recurrence rates are high and ulcer healing must be
accompanied by a well-coordinated program of secondary prevention.[5]
Optimal glycaemic control which can dramatically reduce the recurrence of foot ulcers.
Meticulous attention to foot care and proper management of foot injuries.
Daily inspection of the feet.
www.wjpps.com Vol 6, Issue 7, 2017. 253
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
Gentle cleansing with a mild soap and water.[5]
All patients with diabetes should have an annual foot examination that includes
assessment for anatomic deformities, skin breaks, nail disorders, loss of protection
sensation, diminished arterial supply and inappropriate footwear.
Educating patients and caretakers about proper foot care and periodic self-foot
examinations are effective interventions to prevent ulceration.[22]
Wearing correct, well-fitting footwear that provides adequate support.
Appropriate management of minor wounds and referral for any minor non healing wound
Avoid walking barefoot.[5]
Skin is kept moisturized with the application of topical moisturizers after washing the feet
gently with soap and water.
Other co-morbidities like hypertension and hyperlipidaemia which predispose to vascular
occlusion should be treated.[26]
Other effective clinical interventions include optimizing glycemic control, smoking
cessation, debridement of calluses, and certain types of prophylactic foot surgery.[22]
MANAGEMENT DIABETIC FOOT ULCERS
Standard care for DFU is ideally provided by a multidisciplinary team by ensuring glycemic
control, adequate perfusion, local wound care and regular debridement, off-loading of the
foot, control of infection by appropriate antibiotics and management of comorbidities.
Educating patients helps in preventing ulcers and their recurrence.[26]
The essential components of management are.
a. Treating underlying disease processes
b. Ensuring adequate blood supply
c. Local wound care, including infection control
d. Pressure offloading.[12]
Debridement
Debridement consists of removal of all necrotic tissue, peri-wound callus and foreign bodies
down to viable tissue. Proper debridement is necessary to decrease the risk of infection and
reduce peri-wound pressure, which can impede normal wound contraction and healing. There
are different kinds of debridement which includes surgical, enzymatic, autolytic, mechanical,
and biological.[25]
www.wjpps.com Vol 6, Issue 7, 2017. 254
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
Autolytic
Autolytic debridement uses the body‘s own natural enzymes to break down and digest
necrotic tissue. Autolytic debridement also involves the use of moisture in semi-occlusive or
occlusive dressings to aid in the efficiency of liquefying devitalized tissue. Dressings for
autolytic debridement include hydrocolloids, hydrogels and films. The hydrogels were
significantly more effective than gauze dressings or standard care in healing diabetic foot
ulcers.[27]
Biological
Sterile maggots of the green bottle fly (Lucilia sericata) are placed directly into the affected
area and held in place by a close net dressing. The larvae have a ferocious appetite for
necrotic material while actively avoiding newly formed healthy tissue.[28]
Mechanical
Although it is a simple and an inexpensive tool, it can remove both viable and also non-viable
tissues leading to pain in sensate foot. The wet gauze dressing is applied to the wound bed
and then kept to dry. The necrotic debris embedded in the gauze is mechanically stripped
from the wound bed on gauze removal.[10]
Enzymatic debridement
Enzymatic debridement speeds up the process and an ointment is applied to the wound,
which contains special enzymes to accelerate the removal of the devitalised or dead tissue
from the wound bed.[5]
Dressing
Ideally, dressings should confer moisture balance, protease sequestration, growth factor
stimulation, antimicrobial activity, oxygen permeability, and the capacity to promote
autolytic debridement that facilitates the production of granulation tissues and the re-
epithelialization process. Wound dressing can be categorized as passive, active, or
interactive. Passive dressings are used as protective functions and for acute wounds because
they absorb reasonable amounts of exudates and ensure good protection. Active and
interactive dressings are capable of modifying the physiology of a wound by stimulating
cellular activity and growth factors release. The main categories of dressings used for DFU
are as follows: films, hydrogels, hydrocolloids, alginates, foams, and silver-impregnated.[1]
New advanced dressings are being researched, for example Vulnamin© gel made of amino
www.wjpps.com Vol 6, Issue 7, 2017. 255
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
acids and hyaluronic acid are used along with elastocompression has shown favourable
results. Promogran© by Johnson and Johnson‘s is a freeze dried matrix composed of collagen
and oxidized regenerated cellulose. When in contact with wound exudates, it forms a
biodegradable gel that physically binds and inactivates matrix metalloproteases that affects
wound healing.[14]
Offloading
Total contact cast (TCC), removable cast walkers, custom shoes, half-shoes, soft heel shoes,
padded socks, and shoe inserts, wheelchairs, crutches etc. have been used for offloading the
foot to prevent and treat the DFUs. The aim is to reduce the plantar pressure by redistributing
it to a larger area, to avoid shear and friction, and to accommodate the deformities.[26]
Inadequate offloading leads to tissue damage and ulceration. The gold standard is the total
contact cast (TCC). This is a well moulded, minimally padded foot and lower leg cast that
distributes pressures evenly over the entire plantar surface of the foot. It ensures compliance
because it is not easy for the patient to remove. Using a TCC in patients with a unilateral
uncomplicated plantar ulcer can reduce healing time by around six weeks1. Inappropriate
application of TCCs may result in new ulcers, and TCCs are contraindicated in deep or
draining wounds or for use with noncompliant, blind, morbidly obese, or severely vascularly
compromised patients.[25]
Medical treatment
Strict glycaemic control should be maintained with the use of diabetic diet, oral
hypoglycaemic agents and insulin. Infections of the soft tissue and bone are the leading cause
of hospital admissions in patients with DFUs. Antibiotics are preferably given intravenously
for limb threatening infections. Gabapentin and pregabalin have been used for symptomatic
relief for painful neuropathy in DM. Aldose reductase inhibitors are being studied and have
shown to be effective in inhibiting progression of peripheral neuropathy. Autonomic
dysfunction may require the use of beta-blockers. Medical management of symptoms of
vascular insufficiency like intermittent claudication includes Cilostazol or Pentoxifylline
besides exercise therapy.[14]
Adjuvant therapy
Hyperbaric oxygen therapy (HBOT) has shown promise in the treatment of serious cases of
non-healing DFU, which are resistant to other therapeutic methods. HBOT involves
intermittent administration of 100% oxygen, usually in daily sessions. During each session,
www.wjpps.com Vol 6, Issue 7, 2017. 256
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
patients breathed pure oxygen at 1.4-3.0 absolute atmospheres during 3 periods of 30 min
(overall 90 min) intercalated by 5 min intervals in a hyperbaric chamber.[1] Hyperbaric
oxygen therapy (HBOT) has the advantage of reduction of tissue hypoxia, edema, increase
angiogenesis and erythrocytes deformability, antimicrobial effects and increase fibroblastic
activity. HBOT is approved as an adjunctive treatment to be used in chronic non-healing
ulcers by the Undersea and Hyperbaric Medical Society.[10] Low energy lasers have also been
used as an adjunctive therapy for DFUs. They act by increasing microcirculation and
improving healing of the ischemic DFU. Growth factors for example recombinant human
platelet derived growth factor (rhPDGF), topical platelets and platelet rich plasma have also
been used in treating DFUs and have shown favourable results.[14]
Surgical management
Revascularization surgery
As diabetes is chronic and progressive, it makes sense to have conservative surgical
approaches that include surgical revascularization. A successful surgical bypass of larger
vessel disease may enable more conservative treatment of the diabetic foot.[28]
Revascularization by open surgery of occlusive disease of the distal arteries is carried out
mainly by bypass with autologous material (preferably saphenous vein). In turn, endovascular
surgery techniques mainly include percutaneous transluminal angioplasty (PTA), which may
be combined with stenting, laser and plaque volume reduction techniques. The exponential
increase of the use of these endovascular procedures, compared with open surgical
revascularisation, is primarily due to the greater benefit with respect to the secondary risk of
low percentages of morbidity and mortality associated with the percutaneous techniques.
Mixed techniques (open + endovascular surgery) may be used.[8]
Wound closure
Wound closure is attempted once the ulcer is clean with healthy granulation tissue. Primary
closure is possible for small wounds; tissue loss can be covered with the help of skin graft,
flap or commercially available skin substitutes. Split-thickness skin grafts are preferred over
full thickness grafts DFUs with exposed tendon, ligament or bone require coverage with
muscle flaps. Flaps can be either local (for smaller wounds) or freeflaps (for large area).
Latissimus dorsi, gracilis or rectus abdominis are the commonly used free flaps. The
limitations of standard flaps include donor site morbidity, difficulty in shaping the flaps and
interference with footwear.[26]
www.wjpps.com Vol 6, Issue 7, 2017. 257
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
Amputation
Amputation may be indicated in the following circumstances.
Ischaemic rest pain that cannot be managed by analgesia or revascularization
A life-threatening foot infection that cannot be managed by other measures
A non-healing ulcer that is accompanied by a higher burden of disease than would result
from amputation. In some cases, for example, complications in a diabetic foot render it
functionally useless and a well performed amputation is a better alternative for the
patient.
Patients at high risk for ulceration (such as patients who have undergone an amputation for a
DFU) should be reviewed 1–3 monthly by a foot protection team. At each review patients'
feet should be inspected and the need for vascular assessment reviewed.[12]
CONCLUSION
Diabetic foot complication is the most devastating complication of diabetes. This article is a
clinical overview of diabetic foot ulcer and diabetic foot infection. Physician plays an
important role in management of aetiological factors like vasculopathy, neuropathy and
infection is essential to get good outcomes. The main components of management that can
ensure successful and rapid healing of DFU includes wound debridement, advanced dressing,
offloading, surgery, and advanced therapies, which are used clinically. Physician plays an
important role in prescribing Guideline-based treatment for diabetic foot infections and the
employment of multidisciplinary teams would help improve outcome and minimize
amputations.
REFERENCE
1. Leila Yazdanpanah, Morteza Nasiri, Sara Adarvishi. Literature review on the
management of diabetic foot ulcer. World journal of diabetes, 2015; 6(1): 37-53.
2. Saba Noor, Mohammad Zubair, Jamal Ahmad. Diabetic foot ulcer—A review on
pathophysiology, classification and microbial etiology. Diabetes & Metabolic Syndrome:
Clinical Research & Reviews, 2015; 9: 192–199.
3. Yanling Wu, Yanping Ding, Yoshimasa Tanaka and Wen Zhang.. Risk Factors
Contributing to Type 2 Diabetes and Recent Advances in the Treatment and Prevention.
International Journal of Medical Sciences, 2014; 11(11): 1185-1200.
4. Orthopedics one articles, 132-140.
www.wjpps.com Vol 6, Issue 7, 2017. 258
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
5. Bronwyn Green, Andy Zoepke. Diabetes and Diabetic Foot Ulcers: An often hidden
problem. S Afr Pharm J, 2013; 55(6): 515-518.
6. Benjamin A. Lipsky,1 Anthony R. Berendt,2 Paul B. Cornia,3 James C. Pile et al. 2012
Infectious Diseases Society of America Clinical Practice Guideline for the Diagnosis and
Treatment of Diabetic Foot Infections. IDSA Guidelines, 2012; 54(12): 132–173.
7. Amit Kumar C Jain, Sunil Joshi. Diabetic Foot Classifications: Review of Literature.
Medicine Science, 2013; 2(3): 715-721.
8. Francisco Lozano and Albert Clará (SEACV). Diego Alcalá (AEC); Albert Clará, José
Ignacio Blanes, Consensus document on treatment of infections in diabetic foot. Rev Esp
Quimioter, 2011; 24(4): 233-262.
9. Vishnu Datta M, D.V Gowda, Karthik shanmukha. Complications and risk management
of diabetic foot ulcer: A review. Journal of Scientific and Innovative Research, 2014;
3(3): 363-371.
10. Noha Amin, John Doupis. Diabetic foot disease: From the evaluation of the ―foot at risk‖
to the novel diabetic ulcer treatment modalities. World journal of diabetes, 2016; 7(7):
153-164.
11. Mohammad Zubair1, Abida Malik2, Jamal Ahmad. Diabetic foot ulcer: A review.
American Journal of Internal Medicine, 2015; 3(2): 28-49. B.
12. Paul Chadwick, Michael Edmonds, Joanne McCardle, David Armstrong et al. Best
Practice Guidelines: Wound Management in Diabetic Foot Ulcers. Wounds International,
2013.
13. Diabetic foot ulcers – treatment and prevention. A coloplast quick guide, 2-30.
14. Simerjit Singh, Dinker R Pai and Chew Yuhhui. Diabetic Foot Ulcer – Diagnosis and
Management. Clinical Research on Foot & Ankle, 2013; 1(3): 1-9.
15. Saba Noor, Mohammad Zubair, Jamal Ahmad. Diabetic foot ulcer—A review on
pathophysiology, classification and microbial etiology. Diabetes & Metabolic Syndrome:
Clinical Research & review, 2015; 9: 192–199.
16. JJ Mendes, J Neves. Diabetic Foot Infections: Current Diagnosis and Treatment. The
Journal of Diabetic Foot Complications, 2012; 4(2): 26-45.
17. Thanh Dinh. Global perspective on diabetic foot ulcerations. 2011.
www.intechopen.com.1-278.
18. Robert G. Frykberg, DPM, MPH, Thomas Zgonis, DPM, David G. Armstrong. Diabetic
foot disorders: A clinical practice guideline (2006 revision). The Journal of foot and ankle
surgery, 2006; 45(5): 1-66.
www.wjpps.com Vol 6, Issue 7, 2017. 259
Vishwas et al. World Journal of Pharmacy and Pharmaceutical Sciences
19. Kimberlee B. Hobizal, DPM and Dane K. Wukich, MD. Diabetic foot infections: current
concept Review. Diabetic Foot & Ankle, 2012; 3: 1-8.
20. Sign 116 Management of diabetes. A national clinical guideline, 2010; 1-161.
21. Ashok Damir. Clinical Assessment of Diabetic Foot patient. JIMSA, 2011; 24(4):
199-203.
22. Mazen S. Bader. Diabetic Foot Infection. American Family Physician, 2008; 78(1):
72-79.
23. B. A. Lipsky, J. Aragon-Sanchez, M. Diggle, J. Embil et al., IWGDF Guidence on the
diagnosis and management of foot infections in persons with diabetes. 2015 International
Working Group on the Diabetic Foot.
24. Tatiana N. Demidova-Rice, Michael R. Hamblin and Ira M. Herman. Acute and Impaired
Wound Healing: Pathophysiology and Current Methods for Drug Delivery, Part 1:
Normal and Chronic Wounds: Biology, Causes, and Approaches to Care. Adv Skin
Wound Care. Author manuscript, 2012; 25(7): 1-21.
25. Ingrid Kruse, DPM, and Steven Edelman, MD. Evaluation and Treatment of Diabetic
Foot Ulcers. Clinical diabetes, 2006; 24(2): 91-93.
26. Simerjit Singh, Dinker R Pai and Chew Yuhhui. Diabetic Foot Ulcer – Diagnosis and
Management. Clinical Research on Foot & Ankle. Clin Res Foot Ankle, 2013; 1(3): 2-9.
27. Assessment and Management of Foot Ulcers for People with Diabetes 2nd edition.
Clinical Best Practice Guidelines, March 2013; 1-156.
28. Elroy P Weledji and Pius Fokam. Treatment of the diabetic foot – to amputate or not?
Weledji and Fokam BMC Surgery, 2014; 14(83): 1-6.
www.wjpps.com Vol 6, Issue 7, 2017. 260
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- History TakingDocument23 pagesHistory TakingAliMalik0% (1)
- House OfficerDocument32 pagesHouse Officerapi-3705046100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- 3 Pressure Ulcer (Bedsores) Nursing Care Plans - NurseslabsDocument12 pages3 Pressure Ulcer (Bedsores) Nursing Care Plans - NurseslabsJOSHUA DICHOSONo ratings yet
- Manage Open Tibial FracturesDocument51 pagesManage Open Tibial FracturesStar Cruise100% (1)
- Week 9 - Ch. 31 - SkinDocument31 pagesWeek 9 - Ch. 31 - SkinMary SingletonNo ratings yet
- NHS Fife Assessment Chart For Wound ManagementDocument3 pagesNHS Fife Assessment Chart For Wound ManagementBrian Harris100% (1)
- Wound Essentials 8 1 Debridement Consensus Recommendations For PracticeDocument5 pagesWound Essentials 8 1 Debridement Consensus Recommendations For PracticeAndaz MortinNo ratings yet
- Hospital Burn CareDocument9 pagesHospital Burn CareAgung Rizka PratamaNo ratings yet
- Diabetic Foot UlcerDocument44 pagesDiabetic Foot UlcerCandy Lee100% (1)
- Wound AssessmentDocument19 pagesWound Assessmentdrsonuchawla100% (1)
- ZZZ PDFDocument2 pagesZZZ PDFFarah MawazirNo ratings yet
- Potato-Mushroom Gratin Recipe - Bon Appetit PDFDocument2 pagesPotato-Mushroom Gratin Recipe - Bon Appetit PDFFarah MawazirNo ratings yet
- Osteoarthritis Causes, Risk Factors, and TreatmentDocument4 pagesOsteoarthritis Causes, Risk Factors, and TreatmentFarah MawazirNo ratings yet
- Safari - 22 Oct 2018 at 9:05 PM 2Document1 pageSafari - 22 Oct 2018 at 9:05 PM 2Farah MawazirNo ratings yet
- Safari - 22 Oct 2018 at 9:05 PM 2Document1 pageSafari - 22 Oct 2018 at 9:05 PM 2Farah MawazirNo ratings yet
- Safari - 22 Oct 2018 at 9:05 PM 2Document1 pageSafari - 22 Oct 2018 at 9:05 PM 2Farah MawazirNo ratings yet
- Microbiology of Diabetic Foot Infections in A Teaching Hospital in Malaysia: A Retrospective Study of 194 CasesDocument6 pagesMicrobiology of Diabetic Foot Infections in A Teaching Hospital in Malaysia: A Retrospective Study of 194 CasesFarah MawazirNo ratings yet
- Potato Au GratinDocument2 pagesPotato Au GratinFarah MawazirNo ratings yet
- QR Management of Dengue Infection in Adults Malaysia (2nd Edition)Document8 pagesQR Management of Dengue Infection in Adults Malaysia (2nd Edition)Zul IsmailNo ratings yet
- Y 5Document1 pageY 5Farah MawazirNo ratings yet
- DynaMed Plus - Bronchiolitis PDFDocument1 pageDynaMed Plus - Bronchiolitis PDFFarah MawazirNo ratings yet
- DynaMed Plus - BronchiolitisDocument62 pagesDynaMed Plus - BronchiolitisFarah MawazirNo ratings yet
- Safari - 2 Aug 2018 at 12:15 AM PDFDocument1 pageSafari - 2 Aug 2018 at 12:15 AM PDFFarah MawazirNo ratings yet
- Scan 23 Jul 2017, 8.48 PMDocument3 pagesScan 23 Jul 2017, 8.48 PMFarah MawazirNo ratings yet
- DynaMed Plus - Bronchiolitis PDFDocument1 pageDynaMed Plus - Bronchiolitis PDFFarah MawazirNo ratings yet
- Scan 11 Jul 2017, 3.09 PM PDFDocument7 pagesScan 11 Jul 2017, 3.09 PM PDFFarah MawazirNo ratings yet
- Safari - 2 Aug 2018 at 12:16 AM PDFDocument1 pageSafari - 2 Aug 2018 at 12:16 AM PDFFarah MawazirNo ratings yet
- DynaMed Plus - Bronchiolitis PDFDocument1 pageDynaMed Plus - Bronchiolitis PDFFarah MawazirNo ratings yet
- Scan 5 Jul 2017, 3.47 PMDocument2 pagesScan 5 Jul 2017, 3.47 PMFarah MawazirNo ratings yet
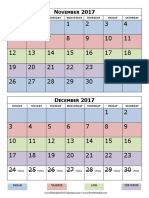
- 2017 Calendar Two Months Per PageDocument1 page2017 Calendar Two Months Per PageFarah MawazirNo ratings yet
- Safari - 2 Aug 2018 at 12:15 AM PDFDocument1 pageSafari - 2 Aug 2018 at 12:15 AM PDFFarah MawazirNo ratings yet
- Scan 1 Aug 2017, 11.10 AM PDFDocument2 pagesScan 1 Aug 2017, 11.10 AM PDFFarah MawazirNo ratings yet
- Scan 1 Aug 2017, 11.10 AMDocument2 pagesScan 1 Aug 2017, 11.10 AMFarah MawazirNo ratings yet
- Scan 11 Jul 2017, 3.09 PMDocument7 pagesScan 11 Jul 2017, 3.09 PMFarah MawazirNo ratings yet
- Surgery On CallDocument2 pagesSurgery On CallFarah Mawazir0% (2)
- 2015 AHA Guidelines Highlights EnglishDocument36 pages2015 AHA Guidelines Highlights EnglishshiloinNo ratings yet
- Sample Test 4 PtA Text BookletDocument8 pagesSample Test 4 PtA Text BookletAparnnaNo ratings yet
- Wound Dressing PDFDocument6 pagesWound Dressing PDFaprilia siregarNo ratings yet
- EU STIMULAN Digital Brochure MA0074R6Document20 pagesEU STIMULAN Digital Brochure MA0074R6Nitin JunejaNo ratings yet
- Altrazeal® Application Guide 2.0 VFDocument2 pagesAltrazeal® Application Guide 2.0 VFdeeepNo ratings yet
- James Neisler ComplaintDocument25 pagesJames Neisler ComplaintMichael_Lee_RobertsNo ratings yet
- Kelly 2005 British Journal of Oral and Maxillofacial SurgeryDocument1 pageKelly 2005 British Journal of Oral and Maxillofacial SurgerylalajanNo ratings yet
- Iatrogenic Segmental Defect How I Debride.3Document7 pagesIatrogenic Segmental Defect How I Debride.3Hizkyas KassayeNo ratings yet
- First Middle East Experience WDocument8 pagesFirst Middle East Experience WAsmat BurhanNo ratings yet
- MUEDocument269 pagesMUEKian GonzagaNo ratings yet
- December, 11th 2013: What Is An Emergency?Document11 pagesDecember, 11th 2013: What Is An Emergency?Sawsan Z. JwaiedNo ratings yet
- Exam 2Document4 pagesExam 2Azra MuzafarNo ratings yet
- Papaya Wuond DressingDocument4 pagesPapaya Wuond Dressingapi-3801331No ratings yet
- E W C O F: Arly Ound ARE IN PEN RacturesDocument3 pagesE W C O F: Arly Ound ARE IN PEN RacturesMatheis Laskar PelangiNo ratings yet
- Pressure Ulcer Prevention & Management: Carol Compas, RN, BSN Jeff Edwards, RNDocument65 pagesPressure Ulcer Prevention & Management: Carol Compas, RN, BSN Jeff Edwards, RNsalehkpNo ratings yet
- All About Maggot Therapy 2nd ViewDocument10 pagesAll About Maggot Therapy 2nd Viewsuvarchala123No ratings yet
- Acute Wound CareDocument0 pagesAcute Wound CareMihaela MitroiNo ratings yet
- Ms 1 Lec Integumentary Disorders 1Document35 pagesMs 1 Lec Integumentary Disorders 1Denise LacapNo ratings yet
- Bovine Digit Surgical TechniqueDocument16 pagesBovine Digit Surgical TechniqueWendyNo ratings yet
- Huge Carbuncle of The Neck With Intracranial ExtenDocument5 pagesHuge Carbuncle of The Neck With Intracranial ExtenAbhishek pandeyNo ratings yet
- Blue Ocean Medical Products Uni NPWT Dressing Kit Application GuideDocument2 pagesBlue Ocean Medical Products Uni NPWT Dressing Kit Application Guideapi-310597983No ratings yet
- Conservative Sharp Wound DebridementDocument7 pagesConservative Sharp Wound DebridementMaria Theszha ANo ratings yet
- Wound Infection Following Repair of Abdominal Wall HerniaDocument13 pagesWound Infection Following Repair of Abdominal Wall HerniadadupipaNo ratings yet