Professional Documents
Culture Documents
ARB CPR Complying With USP 797
Uploaded by
virtechCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ARB CPR Complying With USP 797
Uploaded by
virtechCopyright:
Available Formats
The following article was published in ASHRAE Journal, February 2007.
© Copyright 2007 American Society of Heating, Refrigerating
and Air-Conditioning Engineers, Inc. It is presented for educational purposes only. This article may not be copied and/or distributed elec-
tronically or in paper form without permission of ASHRAE.
Complying With USP 797
Designing
Hospital Pharmacy
HVAC Systems
By Christopher P. Rousseau, P.E., Member ASHRAE; and Adam R. Bare, P.E., Associate Member ASHRAE
T
he furor over compliance with United States Pharmacopoeia Definitions
Several terms in USP 797 are unusual,
(USP) General Chapter 797, Pharmaceutical Compound- or are used in a different manner than is
normal in the HVAC industry. A brief
ing—Sterile Preparations,1 has somewhat subsided with the Joint overview of some of these terms provides
better understanding of the standard and a
Commission for Accreditation of Healthcare Organizations’ decision common vocabulary for discussion.
L a m i n a r A i r f l ow Wo rk b e n c h
not to enforce its requirements. As of this writing, at least 10 states (LAFW) can be either a laminar flow
clean bench or a biological safety cabi-
require compliance (in whole or in part). However, many facilities net.
Anteroom is a clean space located
may desire to comply now to prepare for future federal, state or between the entrance to the buffer room
and other spaces, with a wall separating
industry regulations. Operational modifications are the primary it from the buffer room.
Ante Space is a clean space in the
means of compliance, but the pharmacy’s HVAC system also must pharmacy, logistically, but not physically,
separated from the buffer room.
be evaluated. USP 797 offers some confusing requirements for
About the Authors
HVAC system designers, but compliance in an existing facility is Christopher P. Rousseau, P.E., is a partner and
Adam R. Bare, P.E., is a senior associate at New-
not as difficult as it may seem. comb & Boyd in Atlanta.
36 ASHRAE Journal ashrae.org February 2007
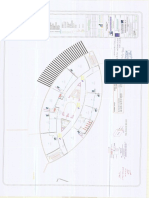
A B Demarcation Line
C
Workbench
Non-ISO
LAFW
LAFW
Anteroom (ISO Buffer Room
(ISO Class 5) Anteroom Buffer Room
Class 8) (ISO Class 8) (ISO Class 8)
Ante Space Buffer Zone
(ISO Class 8) (ISO Class 8)
Hands-Free Hands-Free
Door Door
Workbench
Non-ISO
LAFW
LAFW
ISO Class 8 ISO Class 8
Environment Environment
D ISO Class 5 E ISO Class 5
Barrier Isolator Barrier Isolator
Figure 1: A) Scenario 1, workbenches in ISO Class
Non-ISO Rated Ante/Buffer Room
5 cleanroom; B) Scenario 2, LAFWs in ISO Class 8
Space (ISO Class 8)
clean space, with ante space; C) Scenario 3, LAFWs in
ISO Class 8 cleanroom, with anteroom; D) Scenario 4,
barrier isolator in Non-ISO rated space; E) Scenario
5, barrier isolator in ISO Class 8 clean space.
Barrier Isolator (a glove box) is designed to provide clean configuration has a significant impact on the HVAC system.
makeup air to the workspace and a seamless barrier between The variables involved are risk level, type of equipment used
the workspace and the operator. (LAFW, vs. barrier isolator), and the cleanliness classification
Buffer Area/Zone/Room is a clean space containing the of the pharmacy. The basic configurations are:
primary engineering control equipment, and to which the sec- • An ISO Class 5 clean space, with no LAFW or barrier
ondary engineering controls are applied. isolator equipment (Figure 1a);
Cleanroom is any space where provisions are made to control • An LAFW located in an ISO Class 8 clean space with an
particulates and/or microbes concentrations at or below speci- ante space, but without an anteroom (Figure 1b);
fied limits (typically the buffer area, antespace, or anteroom). • An LAFW located in an ISO Class 8 clean space with an
It corresponds to ASHRAE’s definition of “clean space.” anteroom (Figure 1c);
Compounded Sterile Preparations (CSP) are products • A barrier isolator located in a non-ISO rated space (Figure
administered to patients that require some type of manipulation 1d); and
prior to administration. • A barrier isolator located in an ISO Class 8 space (Figure
ISO Class2 is a measurement of room air cleanliness. ISO 1e).
Class 5 corresponds to Class 100; ISO Class 7 to Class 10,000; Scenario 1 (Figure 1a) is unlikely to be implemented. This
and ISO Class 8 to Class 100,000. Class numbers correspond to arrangement is expensive initially from the standpoint of
the number of particles per ft³ at 0.5 microns or larger. finishes, and operationally from the standpoint of cleaning
Primary Engineering Controls are measures taken to pro- the space and controlling operator-generated particulates.
duce the environment in a LAFW or barrier isolator. Laminar flow clean benches, biological safety cabinets and
Risk Level (low, medium or high) pertains to the risk of the barrier isolators are all specifically designed to provide the
product becoming contaminated, not to a danger presented to required ISO Class 5 space, and can minimize the impact of
the operator. the room finishes and operator procedures on the sterile pro-
Secondary Engineering Controls are measures taken to cesses. This option does provide the most flexibility in that
produce the environment in the spaces occupied by staff and low, medium and high-risk procedures can all be performed
the LAFW or barrier isolator. on the benchtop without the spatial limitations of an LAFW
or barrier isolator.
Space Configuration Scenario 2 (Figure 1b) is probably the best option for
Several ways exist to configure the pharmacy, equipment and most existing facilities. Modifications can be made to the
the HVAC system to meet USP 797 requirements. The specific HVAC system to achieve the ISO Class 8 classification, and
February 2007 ASHRAE Journal 37
the room can be configured to provide a buffer space for the measures (both HVAC-related and not) that are used to control
actual preparation work, and an ante space for storage and these sources of particulates.
product organization work. This scenario will work for low
and medium risk CSPs. Control Measures (Non-HVAC)
Scenario 3 (Figure 1c) is the same as Scenario 2 except a Operator Procedures. While not the focus of this article,
wall is added to physically separate the buffer space from the the standard operating procedures (SOPs) that the pharmacy
ante space. This would allow the performance of high-risk pro- operators follow must be carefully assessed, and periodically
cedures. However, as can be determined from the operational reassessed to ensure that the worker’s particulate generation
sections of USP 797, most high-risk procedures can be avoided is minimized as much as possible. USP 797 includes recom-
with procedural modifications. mended SOPs that pharmacies should use as a baseline. Some
Scenario 4 (Figure 1d) makes use of a barrier isolator to activities yield increased particulate generation rates, such
compensate for the lack of an ISO Class 8 room. This would as gowning and writing.3 Those types of activities should be
be an advantageous option if it were cost prohibitive to achieve confined to the antearea, or outside of the pharmacy altogether.
an ISO Class 8 space with the existing room configuration For worker activities that must occur within the clean space,
or HVAC system. Another advantage is that procedures at all the operations should be configured so as to minimize the par-
three risk levels can be performed. The disadvantage is the ticulate generation to the maximum extent possible.
limitation on throughput caused by the additional operator USP 797 requires that the air quality, on a particulate count
time required to perform procedures in a glovebox. basis, be checked in the LAFWs, barrier isolators, buffer rooms,
Scenario 5 (Figure 1e) is basically the same as Scenario 4, anteareas, and anterooms at least every six months. Airborne
but the room is arranged to have an ISO Class 8 classification. microorganisms are required to be evaluated monthly at various
This arrangement is recommended (but not required) by USP locations (weekly for high risk). When the results from the envi-
797 when a barrier isolator is used. However, this scenario is ronmental monitoring indicate that the counts of particulates are
unlikely because, once the expense of an ISO Class 8 room too high, or that the colony-forming units are trending upwards,
is incurred, a need no longer exists to use a barrier isolator, the SOPs are often the first place to look for resolution.
unless it is required for personnel protection from hazardous Surfaces and Materials. All permanent surfaces, including
or infectious agents. An LAFW will allow compliance at a ceilings, walls and floors, should be monolithic, nonshedding,
lower cost. and washable. All penetrations through the room barrier by
Most existing hospital pharmacies are served by central conduits, lights, diffusers, sprinkler heads, etc., should be
air-handling systems. If the system also serves patient care completely sealed. The devices themselves should be sealed
space, the air-handling unit probably already has high- and washable. All mobile materials and equipment in the clean
efficiency final filters. Even if it does not serve patient care space, such as supply carts and workers’ garments, need to be
areas, it probably already has a higher than normal level of nonshedding.
filtration. Therefore, for most healthcare applications, Scenarios Cleaning Procedures. The cleaning supplies and procedures
2 and 3 are the most technically feasible and affordable, while that are used to sterilize the clean areas must be closely reviewed
still yielding an efficient workspace. Therefore, the remainder of to minimize any particulate or microbial generation during the
this article will focus on how to achieve compliance with USP cleaning procedure, and any residual generation that occurs
797 assuming that the intended result is an ISO Class 8 clean after (i.e., such as from off-gassing). The processes should be
space, with LAFWs providing the ISO Class 5 compounding reviewed thoroughly and coordinated with the facility’s envi-
environment. ronmental systems department. In many cases it is determined
that low-shedding type mop heads need to be used to maintain
How to Achieve an ISO Class 8 Clean Space an ISO Class 8 environment. As with the operator SOPs, clean-
Once the decision has been made that the pharmacy should ing procedures often are reassessed when the results from the
meet a cleanliness level that meets or exceeds ISO Class 8, the environmental monitoring indicate increased particulate or
design team must consider many factors. One might assume microorganism levels.
that, since the ISO standard applies to concentrations of par-
ticulates in the air, this must be primarily an HVAC engineer- Control Measures (HVAC)
ing issue. To the contrary, the necessary provisions to achieve Supply Air Quality. The air being supplied to the pharmacy
ISO Class 8 affect the pharmacy staff first, and the facility’s must be cleaner than the desired air quality of the room itself
architecture (i.e., space planning, finishes, etc.) second. to mitigate the generation of particulates inside of the room
To yield an ISO Class 8 clean space, all sources of particulates (e.g., by workers). Means of calculating the required level of
must be controlled. Examples of these sources are the workers, filtration exist that would be required for the supply air given a
any shedding surfaces (permanent or mobile), the compounding room change rate, a particulate concentration of the air entering
process itself, the supply air to the pharmacy, and infiltration the filters, an internal particulate generation rate, and a desired
through doors, cracks and penetrations. The following are some room air quality. However, since the internal particulate genera-
38 ASHRAE Journal ashrae.org February 2007
tion rates are difficult to predict, 99.97% efficient HEPA filters at the face of the LAFW.5 In general, to maximize the room
typically are used since they are known to successfully yield ventilation effectiveness the HVAC designer should take care
ISO Class 8 spaces for most applications. The HEPA filters can in selecting diffuser locations in relation to where the air will
be located centrally, such as in the air-handling unit, or locally, be exhausted, and low exhaust is not normally necessary.
such as at the pharmacy supply diffusers. Twenty-five percent Room Pressurization. To prevent particulates from infiltrat-
efficient prefilters should be located somewhere upstream of the ing through doors, cracks and penetrations, the clean spaces
HEPA filters to increase the usable life of the more expensive must be kept at positive pressure in relation to neighboring
HEPA filters. Also, the conditions of the HEPA filters need to spaces. The ultimate intent is that the location where the sterile
be routinely checked for loading; the increased air pressure compounding occurs is at the highest pressure, and the room
drop caused by the loading of HEPA filters can have a profound pressures cascade lower farther away from the most sterile
impact on the supply air volume, which in turn can impact room location. The differential pressure across a room barrier causes
pressurization levels. airflow to move in the desired
If the air-handling system direction, which is from the
Airflow (From Ceiling Plenum or Duct)
is dedicated to the pharmacy, cleaner space to the dirtier
consideration should be given space. The target should be a
to locating the HEPA filters in minimum pressure differential
Supply Duct
the air-handling unit. This re- Speed Controller across each room barrier of
Pre-Filter (Optional)
duces maintenance cost (since 0.01in. w.g. (2.5 Pa).6
filters are easier to change in Blower HEPA Digital differential pressure
a mechanical room than in a Filter monitors should be provided
ceiling plenum or clean space at the entrance to the buffer
and typically fewer filters are room and/or anteroom. These
used when located centrally). Ceiling devices can send a signal to the
Additionally, variable fre- Airflow building automation system,
(To Room)
quency drives on the supply which enables the differential
fans can enhance system Figure 2: Fan/filter unit. pressure to be trended over
performance since a constant time, thereby highlighting a
airflow can be delivered while compensating for the loading of degrading differential pressure before it becomes an operational
the HEPA filters. When HEPA filters are centrally located, take problem. Digital monitors with alarms are discouraged when
care to ensure that contaminants are not introduced downstream there is not an anteroom before the buffer room, since when-
of those filters. For example, duct lining and sound attenuators ever the door has been opened to the buffer room its pressure
should not be used downstream of the filters. If humidification will equalize with the adjacent space, causing frequent alarms.
is required to be added to achieve design humidity levels, the If digital monitors are not preferred or applicable, designers
humidifiers should use clean steam. might elect to provide physical indicators (i.e., ball-in-tubes,
Room Air Changes. The number of air changes required to or flutter-strips), to signal pharmacy operators that there is a
achieve ISO Class 8 can vary depending on room geometry, potential contamination problem.
supply air quality, and the projected level of internal particulate Room Temperature and Humidity Control. Occupant
generation. If the supply air passes through HEPA filters before comfort is always a concern, but the temperature and humidity
being introduced into the space, then 20 to 30 air changes per must also be kept low enough to prevent workers from sweating,
hour is typically sufficient to achieve ISO Class 8.4 which increases human particulate and microbial generation
Room Airflow Distribution. The characteristics of the rates. The garb that workers are projected to wear must be
airflow within a pharmacy are an integral aspect of the clean explored during design, since thicker garments will warrant
space’s performance. Airflow patterns are essential in keeping lower room air temperatures. In the absence of specific design
the particulate counts down throughout the space, and also criteria, whenever possible, HVAC designers should ensure
help to effectively wash particulates away from the workers. that the system can produce buffer room temperatures at least
Low velocity, non-aspirating-type diffusers and displacement as low as 68°F (20°C), with the relative humidity maintained
ventilation design should be used to help prevent air turbu- at or below 50% RH. These conditions are required due to the
lence in the room. The placement of LAFWs and diffusers is additional garb worn by workers, similar to that in an operat-
also important. ing room.7
LAFWs should be located in non-traffic paths and away from
doors to prevent movement of operators and the opening/closing Implementation in Existing Facilities
of doors from influencing the airflow patterns at the face of the Hospital renovations are inherently complicated. Mainte-
LAFW. Diffusers should be mounted away from LAFWs, such nance of operations, infection control, and unknown existing
that the supply air velocity does not exceed 50 fpm (0.25 m/s) conditions contribute to this complexity. A pharmacy renova-
40 ASHRAE Journal ashrae.org February 2007
Hospital renovations are inherently complicated. Maintenance of
operations, infection control, and unknown existing conditions con-
tribute to this complexity.
tion for USP 797 compliance involves these items, plus the der of the air-handling unit zone. A better approach is the use
additional technical challenges associated with higher levels of fan/filter units (Figure 2). The fan provides the additional
of air filtration, higher air change rates, differential pressure, static pressure needed to compensate for filter air pressure drop.
and additional exhaust requirements. Ceiling plenum space and acoustical considerations will require
The addition of a new air-handling unit is often the simplest evaluation. The integral blower generates a considerable amount
solution, but for many facilities might not be the most cost- of noise, particularly at the manufacturers’ recommended
effective solution. In that case, perhaps the most difficult feature maximum airflows (typically equivalent to 100 fpm [0.5 m/s]
to include is HEPA filtration of the supply air. HEPA filters im- through the diffuser face), which can be mitigated by using
pose a significant air pressure drop on an existing air-handling more fan/filter units at lower face velocities.
unit. Many facilities may be tempted to merely install HEPA Prefilters only should be provided with the fan/filter units
filter diffusers. However, this will cause either less-than-desired if the inlet air has not already passed through roughing filters,
airflow in the pharmacy, or balancing problems in the remain- such as if the air is being drawn directly from the plenum space,
Advertisement formerly in this space.
42 ASHRAE Journal ashrae.org February 2007
since the prefilters present maintenance and access issues. For air-handling unit, existing ductwork downstream of the filters
example, if a fan/filter unit has a prefilter that can only be ac-should be cleaned and existing duct lining removed.
cessed from an ISO Class 8 space (such as through a ceiling If the existing air-handling system cannot be rebalanced to
access panel or light fixture), the space will be briefly exposed provide additional airflow in the pharmacy, the challenge of
to the dirty air in the ceiling plenum, and the pharmacy will haveproviding additional air changes can be solved in much the
to be temporarily shut down for the amount of time needed to same way as the filtration issues. The fan/filter units discussed
replace the filters and to bring the space particulate counts backpreviously also can provide the additional airflow recirculated
down to ISO Class 8 levels. If HEPA filters are located at the from the space. Unlike most health-care applications where
patient safety and infection control are
the primary issues, the concern in the
pharmacy is primarily particulate con-
trol. Therefore, ventilation air quantities
are not as important, and the additional
supply air can be recirculated through the
local HEPA filters, and not through the
central air-handling unit.
Maintaining the pharmacy at a posi-
tive pressure with respect to all adjacent
spaces (not just the adjacent spaces with
a communicating door) is typically just
a matter of balancing the space for more
supply air than return air. Some sealing
of cracks in the room enclosure may be
required. If any LAFWs are exhausted to
the outside, obtaining positive pressure is
more of a challenge.
The lower temperature and humidity
requirements due to operator clothing
can be a challenge for an existing air-
handling system. The additional supply
air changes provided for particulate
control will help, but probably will not
be sufficient. A lower supply air tempera-
ture will likely be required. This could
possibly be achieved by rebalancing the
Advertisement formerly in this space.
chilled water flow to the cooling coil. If
not, a new cooling coil may be required.
If the supply air temperature is reduced,
the impact on existing reheat coil capacity
must also be evaluated.
Future Issues
Currently, a change to USP 797 has
been proposed that would increase the
buffer area requirements from ISO Class
8 to ISO Class 7.8 This change would
have a significant impact on the HVAC
systems and would require different solu-
tions than those outlined here. The two
sources noted as the basis for this change
deal primarily with the manufacturing
process. It is not clear that this change
would provide substantial improvement
in protecting the sterility of CSPs.
44 ASHRAE Journal ashrae.org February 2007
Unlike most health-care applications where patient safety and infec-
tion control are the primary issues, the concern in the pharmacy is
primarily particulate control.
Conclusion <797>, Pharmaceutical Compounding—Sterile Preparations.
While an initial reading of USP 797 might be intimidating, 2. ISO 14644-1-1999, Classification of Air Cleanliness.
compliance is not that difficult. The ISO Class 8 requirements, 3. 2003 ASHRAE Handbook—HVAC Applications, Chapter 16,
while substantially cleaner than typical office space, are not that Clean Spaces, 3.
much cleaner than normal patient care spaces. Fortunately for 4. 2003 ASHRAE Handbook—HVAC Applications, Chapter 16,
Clean Spaces, 11.
HVAC system designers, with a little planning and attention
5. 2003 ASHRAE Handbook—HVAC Applications, Chapter 14,
to detail, an existing pharmacy facility may be brought into Laboratories, 5.
compliance. The pharmacy professionals have the more difficult 6. Bare, A.R. 2006. “Pressurization strategies for biocontainment.”
task of complying with the new procedural issues. 2007 R&D Laboratory Design Handbook (11):59–63.
7. American Institute of Architects. 2006. AIA Guidelines for
References Design and Construction of Health Care Facilities.
1. United States Pharmacopoeia. 2004. USP General Chapter 8. www.usp797.org.
Advertisement formerly in this space.
46 ASHRAE Journal ashrae.org February 2007
You might also like
- Clean Room Classifications (ISO 8, ISO 7, ISO 6, ISO 5) - MecartDocument1 pageClean Room Classifications (ISO 8, ISO 7, ISO 6, ISO 5) - Mecartboss852No ratings yet
- ISO 4427-5 2007 (E) - Character PDF Document PDFDocument12 pagesISO 4427-5 2007 (E) - Character PDF Document PDFgustavoNo ratings yet
- Defining Restricted Access Barrier SystemsDocument4 pagesDefining Restricted Access Barrier SystemsIvan PopovicNo ratings yet
- 00-3 About This ManualDocument4 pages00-3 About This Manualjonsilver64No ratings yet
- Iso 8536 5 2004Document9 pagesIso 8536 5 2004Katerin MartínezNo ratings yet
- Iso 15065-2005Document9 pagesIso 15065-2005Javier Orellana MenachoNo ratings yet
- Abx SPS Evolution PDFDocument286 pagesAbx SPS Evolution PDFMD. ASHRAFUL100% (1)
- Cleanroom Classifications (Iso 8, Iso 7, Iso 6, Iso 5)Document5 pagesCleanroom Classifications (Iso 8, Iso 7, Iso 6, Iso 5)Yuvraj KumarNo ratings yet
- Iso 5576 - 1997Document39 pagesIso 5576 - 1997jesoneliteNo ratings yet
- ISO 6743-11 - 1990 - Part. 11 - Family P - Pneumatic ToolsDocument4 pagesISO 6743-11 - 1990 - Part. 11 - Family P - Pneumatic ToolsMassimiliano VolaNo ratings yet
- Preview - ISO+8510 2 2006Document4 pagesPreview - ISO+8510 2 2006stefaniacappielloNo ratings yet
- International StandardDocument12 pagesInternational StandardRajesh ThakurNo ratings yet
- Apos For Hipap Instruction Manual Complete PDFDocument190 pagesApos For Hipap Instruction Manual Complete PDFdavidNo ratings yet
- ISO-5496-2006 - Iniciação e Treinamento de Avaliadores para A Detecção e Reconhecimento de OdoresDocument11 pagesISO-5496-2006 - Iniciação e Treinamento de Avaliadores para A Detecção e Reconhecimento de Odoresananda.gouveaNo ratings yet
- Iso 286 1 2010Document13 pagesIso 286 1 2010Carmen CespedesNo ratings yet
- Iso 105-A08-2001Document10 pagesIso 105-A08-2001sandip277No ratings yet
- ISO 6743-5 - 2006 - Part. 5 - Family T - TurbinesDocument9 pagesISO 6743-5 - 2006 - Part. 5 - Family T - TurbinesMassimiliano VolaNo ratings yet
- ISO 16890 2019 12 16 FinalDocument2 pagesISO 16890 2019 12 16 FinalAlexis PradoNo ratings yet
- ISO-21016-2007Document11 pagesISO-21016-2007weerachaiwNo ratings yet
- Iso4427 5Document12 pagesIso4427 5anishsrNo ratings yet
- ISO - TR - 20173 - 2009 - EN - PDF For Material GroupingDocument11 pagesISO - TR - 20173 - 2009 - EN - PDF For Material GroupingS.K.AGRAWALNo ratings yet
- Certificate / Certificat ZertifikatDocument2 pagesCertificate / Certificat Zertifikatdave chaudhuryNo ratings yet
- Cleaning Validation MACO Swab Rinse OvaisDocument5 pagesCleaning Validation MACO Swab Rinse OvaisOvais08100% (9)
- Cleaning Validation MACO Swab Rinse Ovais PDFDocument5 pagesCleaning Validation MACO Swab Rinse Ovais PDFAnonymous yBhOAi5UHNo ratings yet
- NEWS - HEPA FILTER SCAN TEST CONSIDERATIONS FOR ISOLATION ROOMSDocument1 pageNEWS - HEPA FILTER SCAN TEST CONSIDERATIONS FOR ISOLATION ROOMSfernandoNo ratings yet
- Iso 8510 1 1990Document8 pagesIso 8510 1 1990altug deniz CantekinNo ratings yet
- ISO 7090-2000 (Plain Washer, Chamfered)Document10 pagesISO 7090-2000 (Plain Washer, Chamfered)BaoNo ratings yet
- Iso 1409 2006Document9 pagesIso 1409 2006Phạm Thu HuyềnNo ratings yet
- Iso 877 1 2009Document11 pagesIso 877 1 2009Maria Guadalupe Acevedo CruzNo ratings yet
- RABS and Isolators Barrier TechnologyDocument44 pagesRABS and Isolators Barrier TechnologySilke IgemannNo ratings yet
- DDI0408I Cortex A9 Fpu r4p1 TRMDocument27 pagesDDI0408I Cortex A9 Fpu r4p1 TRMKhanh LeNo ratings yet
- Iso 8796.2004Document10 pagesIso 8796.2004ashasinovNo ratings yet
- cobas8000-DataManager - Host Interface Manual10205 PDFDocument286 pagescobas8000-DataManager - Host Interface Manual10205 PDF박수희No ratings yet
- International Standard: IS0 System of Limits and FitsDocument7 pagesInternational Standard: IS0 System of Limits and FitsUsman FarooqNo ratings yet
- Cobas E411 Manual-Unlocked PDFDocument88 pagesCobas E411 Manual-Unlocked PDFZeinab Znd0% (1)
- Engineering Drawing Abbreviations and Symbols - WikipediaDocument31 pagesEngineering Drawing Abbreviations and Symbols - WikipediaAhmodu JibrilNo ratings yet
- International Standard: Sensory Analysis - General Guidance For The Design of Test RoomsDocument8 pagesInternational Standard: Sensory Analysis - General Guidance For The Design of Test Roomssebastian diazNo ratings yet
- ISO-11469-2000 Material MarkingDocument8 pagesISO-11469-2000 Material MarkingGerald CelisNo ratings yet
- ISO 817 2014 Amd 1 2017Document8 pagesISO 817 2014 Amd 1 2017EdwinMedinaBejarano0% (2)
- AOS 10.4.0.1 Release NotesDocument21 pagesAOS 10.4.0.1 Release NotesKelton C CrouchNo ratings yet
- UntitledDocument512 pagesUntitledvodouisantNo ratings yet
- BR EN Linea ZefiroDocument19 pagesBR EN Linea ZefiroHeinson VariasNo ratings yet
- ISO 6743-15 - 2007 - Part. 15 - Family E - Internal Combustion Engine OilsDocument9 pagesISO 6743-15 - 2007 - Part. 15 - Family E - Internal Combustion Engine OilsMassimiliano VolaNo ratings yet
- 2 Understanding Cleanroom Classification PDFDocument22 pages2 Understanding Cleanroom Classification PDFTECHNO DATENo ratings yet
- Iso 3449-2005Document20 pagesIso 3449-2005victorberrospiNo ratings yet
- Iso 679 2009Document12 pagesIso 679 2009HanifNo ratings yet
- ISO 11607 1 - Amend - 2014 07Document16 pagesISO 11607 1 - Amend - 2014 07suryadi tirta widjaya67% (3)
- Engineering Drawing AbbreviationDocument35 pagesEngineering Drawing AbbreviationAminur RahmanNo ratings yet
- 7.1 - Regulatory - FS209E and ISO Cleanroom StandardsDocument6 pages7.1 - Regulatory - FS209E and ISO Cleanroom StandardsAnonymous i8hifn7No ratings yet
- Iso 105 A03 2019Document8 pagesIso 105 A03 2019vnc phonghoaNo ratings yet
- Wavin: Range 600 Inspection Chambers: Product Technical GuideDocument16 pagesWavin: Range 600 Inspection Chambers: Product Technical GuideXAVIER RUBIONo ratings yet
- International Standard: Paints and Varnishes - Standard Panels For TestingDocument8 pagesInternational Standard: Paints and Varnishes - Standard Panels For TestingTülay UçukNo ratings yet
- I-OPE-RA-003 - Rope Access Operating - Rev.7 (Em Revisao)Document36 pagesI-OPE-RA-003 - Rope Access Operating - Rev.7 (Em Revisao)Rael Zorzo MichelsNo ratings yet
- Portuguese IATF 16949 Frequently Asked Questions October 2017Document12 pagesPortuguese IATF 16949 Frequently Asked Questions October 2017Rafael NogueiraNo ratings yet
- 17-08-24 AppliedBiosafetyMeeting PRAES Schmidlin GmuenderDocument32 pages17-08-24 AppliedBiosafetyMeeting PRAES Schmidlin GmuenderPulkitNo ratings yet
- BS Iso 3411-2007Document18 pagesBS Iso 3411-2007marksuseNo ratings yet
- Engineering Drawing Abbreviations and SymbolsDocument18 pagesEngineering Drawing Abbreviations and SymbolsDhinesh Kumar R (Baju)No ratings yet
- SystemVerilog for Hardware Description: RTL Design and VerificationFrom EverandSystemVerilog for Hardware Description: RTL Design and VerificationNo ratings yet
- Diagnostic Communication with Road-Vehicles and Non-Road Mobile MachineryFrom EverandDiagnostic Communication with Road-Vehicles and Non-Road Mobile MachineryRating: 1 out of 5 stars1/5 (1)
- Static Analysis of Software: The Abstract InterpretationFrom EverandStatic Analysis of Software: The Abstract InterpretationNo ratings yet
- AV Jolie Ville Expo Heat DissipationDocument3 pagesAV Jolie Ville Expo Heat DissipationvirtechNo ratings yet
- FM DataSheets - Cause and Effect of Fire and ExplosionsDocument22 pagesFM DataSheets - Cause and Effect of Fire and Explosionsyunying21No ratings yet
- 7-0 Causes and Effects of Fires and ExplosionsDocument21 pages7-0 Causes and Effects of Fires and ExplosionsvirtechNo ratings yet
- Hor in Mep 002 Rev.00Document4 pagesHor in Mep 002 Rev.00virtechNo ratings yet
- AV Jolie Ville Expo Heat DissipationDocument3 pagesAV Jolie Ville Expo Heat DissipationvirtechNo ratings yet
- 30-04-2018 JV BMS Specs PDFDocument98 pages30-04-2018 JV BMS Specs PDFvirtechNo ratings yet
- HvacDocument26 pagesHvacvirtechNo ratings yet
- E20s HAP50 - Manual HAP PDFDocument144 pagesE20s HAP50 - Manual HAP PDFAnonymous XhkjXCxxsT100% (1)
- Room Pressure For Critical EnvironmentsDocument6 pagesRoom Pressure For Critical Environmentsvirtech100% (1)
- 03-Kim Spitler Delahoussaye 02 Pt1Document3 pages03-Kim Spitler Delahoussaye 02 Pt1virtechNo ratings yet
- Carrier E20s HAP50 ManualDocument1 pageCarrier E20s HAP50 ManualvirtechNo ratings yet
- MEP ChecklistDocument8 pagesMEP ChecklistvirtechNo ratings yet
- HVAC Kim Spitler Delahoussaye 02 Pt11Document10 pagesHVAC Kim Spitler Delahoussaye 02 Pt11mohdnazirNo ratings yet
- KKMC MH Aec Eep DG 14202 015 (C)Document1 pageKKMC MH Aec Eep DG 14202 015 (C)virtechNo ratings yet
- Guidelines of Septic Systems DesignDocument1 pageGuidelines of Septic Systems DesignvirtechNo ratings yet
- Drain Hvac S.F C PDFDocument1 pageDrain Hvac S.F C PDFvirtechNo ratings yet
- Guidelines of Septic Systems DesignDocument16 pagesGuidelines of Septic Systems DesignJowie100% (1)
- M 334 ContentDocument62 pagesM 334 ContentvirtechNo ratings yet
- Al Batha Sep2017Document1 pageAl Batha Sep2017virtechNo ratings yet
- 2010 - ASHRAE Journal, Greening Hospitals, Kaiser Permanente - ArticleDocument8 pages2010 - ASHRAE Journal, Greening Hospitals, Kaiser Permanente - ArticlevirtechNo ratings yet
- Ecology UnitDocument14 pagesEcology UnitvirtechNo ratings yet
- IC-8 Chilled Water SequenceDocument4 pagesIC-8 Chilled Water Sequencevirtech0% (1)
- Refer To Service Building Requirements LayoutDocument1 pageRefer To Service Building Requirements LayoutvirtechNo ratings yet
- BS en 752-1 1996Document16 pagesBS en 752-1 1996virtechNo ratings yet
- PD Cen-Tr 15589-2014 PDFDocument16 pagesPD Cen-Tr 15589-2014 PDFvirtechNo ratings yet
- Internal Gas Piping Design and Installation GuidelinesDocument27 pagesInternal Gas Piping Design and Installation Guidelinesvirtech67% (3)
- Fan Selection GuideDocument4 pagesFan Selection GuidevirtechNo ratings yet
- VLC Install GuideDocument34 pagesVLC Install GuidevirtechNo ratings yet
- Frru004 Mom4Document2 pagesFrru004 Mom4virtechNo ratings yet
- Centrifugal Aftermarket Solutions BrochureDocument8 pagesCentrifugal Aftermarket Solutions BrochureJose Renato MendesNo ratings yet
- AHU-Guideline 01 General Requirements Fo PDFDocument24 pagesAHU-Guideline 01 General Requirements Fo PDFkayden chinNo ratings yet
- DISJUNTOR DE MÉDIA TENSÃO COOPER VN2-24E+Brochure PDFDocument16 pagesDISJUNTOR DE MÉDIA TENSÃO COOPER VN2-24E+Brochure PDFedmarrobNo ratings yet
- Lars Part Ix - Safety Managment System Requirements-SmsDocument24 pagesLars Part Ix - Safety Managment System Requirements-SmssebastienNo ratings yet
- Thermochemistry: Purpose of The ExperimentDocument20 pagesThermochemistry: Purpose of The ExperimentAngel LacsonNo ratings yet
- SyllabusDocument2 pagesSyllabusjackychen101No ratings yet
- LN Tutorial Services - Machine Design, Materials & Shop PracticesDocument4 pagesLN Tutorial Services - Machine Design, Materials & Shop PracticesEngr Amethyst RiegoNo ratings yet
- PW DebugDocument2 pagesPW DebugAimeeFieldsNo ratings yet
- Wetex Middle East Exhibitors 2016Document7 pagesWetex Middle East Exhibitors 2016Dinkar JoshiNo ratings yet
- Boiler FormulasDocument5 pagesBoiler FormulasAnonymous 6Mb7PZjNo ratings yet
- Rcs454: Python Language Programming LAB: Write A Python Program ToDocument39 pagesRcs454: Python Language Programming LAB: Write A Python Program ToShikha AryaNo ratings yet
- Romanian Power Grid Substation Refitting StrategyDocument16 pagesRomanian Power Grid Substation Refitting StrategyParmeshwar MbNo ratings yet
- A Triangle Area Based Nearest Neighbors Approach To Intrusion DetectionDocument8 pagesA Triangle Area Based Nearest Neighbors Approach To Intrusion DetectionHomeed AlzhraniNo ratings yet
- Physical and Chemical Changes Lab ReportDocument5 pagesPhysical and Chemical Changes Lab ReportWilliam CarriereNo ratings yet
- Farris 2700 ManualDocument12 pagesFarris 2700 ManualNelson AlvarezNo ratings yet
- Coke Bottle Tutorial For MayaDocument42 pagesCoke Bottle Tutorial For MayadumbledoreaaaaNo ratings yet
- HTML DOM TutorialDocument11 pagesHTML DOM Tutorialapi-3819971100% (1)
- Excavation Safety GuideDocument62 pagesExcavation Safety Guideallen 5222100% (1)
- Indigo GdpiDocument1 pageIndigo Gdpimanoj agrawallaNo ratings yet
- Description Wincc Project Scanner enDocument9 pagesDescription Wincc Project Scanner enDugPigeonNo ratings yet
- Slump and Compacting Factor Test Values and Uses in Concrete WorkabilityDocument2 pagesSlump and Compacting Factor Test Values and Uses in Concrete WorkabilityNick GeneseNo ratings yet
- Competency-Check-H e I ADocument20 pagesCompetency-Check-H e I Abaldo yellow4No ratings yet
- Static Electricity and Charge AccumulationDocument75 pagesStatic Electricity and Charge AccumulationArjav DesaiNo ratings yet
- DrillingMotors MKT 001 01Document10 pagesDrillingMotors MKT 001 01Aman Aayra SrivastavaNo ratings yet
- Galaxy Electrical: Zener DiodesDocument3 pagesGalaxy Electrical: Zener Diodesdragon-red0816No ratings yet
- Price ListDocument2 pagesPrice ListCHeng SOngco TAlosigNo ratings yet
- Hotpoint Service Manual Fridge FreezerDocument36 pagesHotpoint Service Manual Fridge FreezerMANUEL RODRIGUEZ HERRERA100% (1)
- PNG382 FT en 11Document2 pagesPNG382 FT en 11Misu1983No ratings yet
- HE Hydra Jar Manual 6-80Document31 pagesHE Hydra Jar Manual 6-80Yuri KostNo ratings yet
- Basic Electronics PowerpointDocument16 pagesBasic Electronics PowerpointEarle Sean MendozaNo ratings yet