Professional Documents
Culture Documents
PHARMACOLOGY: PRELIMINARIES ROUTES AND PROCESSES
Uploaded by
Romie Solacito0 ratings0% found this document useful (0 votes)
105 views4 pagesUIC - MLS
Original Title
Basic Pharmacology - Medical Technology
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentUIC - MLS
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
105 views4 pagesPHARMACOLOGY: PRELIMINARIES ROUTES AND PROCESSES
Uploaded by
Romie SolacitoUIC - MLS
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
PHARMACOLOGY: PRELIMINARIES o Disadvantages: unsuitable for oily substances;
Romie Solacito, MLS3C bolus injection may result in adverse effects;
INTRODUCTION most substances must be slowly injected; strictly
Pharmacology – the body of knowledge concerned aseptic techniques needed
with action of chemical on biologic systems Subcutaneous – depends on drug diluents: aqueous
Drugs – any substances that brings about a change in solution – prompt; depot preparations – slow and
biologic function through its chemical actions sustained
Pharmacy – the science of Identification, selection, o Advantages: suitable for slow-release drugs;
preservation standardization, compounding, and ideal for some poorly soluble suspensions
dispensing of medical substance. o Disadvantages: Pain or necrosis if drug is
Pharmacodynamics – the study of the biological irritating; unsuitable for drugs administered
therapeutic effects of drugs; what the drug does to large volumes
the body Intramuscular – depends on drug diluents: Aqueous
Pharmacokinetics – deals with the proper selection solution – prompt; depot preparation – slow and
and use of drugs for the prevention and treatment of sustained
disease o Advantages: Suitable if drug volume is
Toxicology – it’s the science of poison; substance moderate; suitable for oily vehicles and certain
that cause harmful, dangerous or fatal symptoms in irritating substances; preferable to intravenous if
living substance. patient must self-administer
Factors that influences proper dose of a drug: o Disadvantages: Affects certain lab tests (creatine
o Age kinase); can be painful; can cause intramuscular
o Pharmacogenetics haemorrhage (precluded during anticoagulation
o Body Weight therapy)
o Body Surface Area Transdermal/Patch – Slow and sustained
o Sex o Advantages: Bypasses the first-pass effect;
o Pathologic State convenient and painless; ideal for drugs that are
o Tolerance lipophilic and have oral bioavailability; ideal for
o Concomitant drug therapy drugs that are quickly eliminated from the body
o Time and condition of administration o Disadvantages: Some patients are allergic to
o Dosage form and route of administration patches, which can cause irritation; drug must be
highly lipophilic; may cause delayed delivery of
PHARMACOKINETICS drug to pharmacological site of action; limited to
Route of Drug Administration drugs that can be taken in small daily doses
Oral – Variable; affected by many factors Rectal – Erratic and variable
o Advantages: safest and most common, o Advantages: partially bypasses first-pass effect;
convenient, and economical route of bypasses destruction by stomach acid; ideal if
administration drug cause vomiting; ideal in patients who are
o Disadvantages: Limited absorption of some vomiting, or comatose
drugs; food may affect absorption; patient o Disadvantages: Drugs may irritate the rectal
compliance is necessary; drugs nay be mucosa; not a well-accepted route
metabolized before systemic adsorption. Inhalation – Systemic absorption may occur; this is
not always desirable
Intravenous – absorption not required
o Advantages: can have immediate effects; ideal if o Advantages: Absorption is rapid: can have
dosed in large volumes; suitable for irritating immediate effects; ideal for gases; effective for
substances and complex mixtures; valuable in patients with respiratory problems; dose can be
emergency situations; dosage titration titrated; localized effect to target lungs: lower
permissible; ideal for high molecular weight doses used compared to that with oral or
proteins and peptide drugs. parenteral administration; fewer systemic side
effects
o Disadvantages: Most addictive route (drug can
be enter the brain quickly); patient may have
difficulty regulating dose; some patients may
have difficulty using inhalers
Sublingual – Depends on the drugs: Few drugs (i.e.
nitroglycerin) have rapid, direct systemic adsorption;
most drugs erratically or incompletely absorbed
o Advantages: Bypasses first-pass effect; bypasses
destruction by stomach acid; drug stability
maintained because the pH of saliva relatively
neutral; may cause immediate pharmacological
effects
e. Expression of P-glycoprotein
o Disadvantages: Limited to certain types of drugs;
f. Route of administration
limited to drugs that can be taken in small doses;
may lose part of the drug dose if swallowed
Transport Processes – mechanism of drug movement
across cell membrane
1. Passive Transport/Diffusion – most dominant;
movement of particles from higher concentration to
lower concentration; non-energy requiring; factors
affecting the processes: surface area, concentration,
thickness, and diffusion coefficient (permeability) – g. Bioavailability – measure the rate and extent of
particle size and liposolubility drug entry into the systemic circulation. Two
2. Carrier-Mediated Transport – Utilize carrier proteins methods of determining Bioavailability:
features: selectivity, subject to Cumulative Urinary Excretion
competition/inhibition and saturability. Types: Drug Plasma Concentration: uses time data,
a. Facilitated Diffusion – along a concentrated and most commonly used
gradient h. Factors that influence bioavailability:
b. Active Transport – energy requiring
First-pass hepatic metabolism
c. Convective Transport – solvent-drag movement
Solubility of drug
3. Endocytosis/Picocytosis/Exocytosis – Cell drinking,
Chemical instability
vesicle mediated, not requiring to be in aqueous
Nature of the drug formulation
solution, energy requiring, and ADEK
2. Distribution – the process of drug movement from
Drug Pathway the systemic circulation to the different body
compartments and into the site of Action
1. Absorption – rate and extent of drug entry into the
a. Affected by two physiologic parameters
systemic circulation. Factors influencing absorption
Cardiac output – volume pumped by the heart
a. Effects of pH on drug absorption
per minute
b. Blood flow to the absorption site
Regional blood flow – fraction of cardinal
c. Total surface area available for absorption
output
d. Contact time at the absorption surface
b. Two distribution parameters:
High Gastric Emptying Time, Low Gastric
Protein binding – binding of drugs to plasma
Emptying Rate = Low Rate of Absorption
proteins and tissues
Binding to plasma proteins
Binding to tissues proteins
Volume of distribution – hypothetical volume
of the body fluid necessary to dissolve a given
dose of drug or amount of drug to a Hepato-biliary Excretion
concentration equal to the plasma Pulmonary Excretion
(Application: estimated loading dose)
3. Metabolism – Sites: Liver (major), intestine, blood Dose-Time Relationship
plasma (esterases), and kidneys (dihydropeptidases) Half Life – the time taken for the concentration of
a. Exceptions: drug in the blood or plasma to decline to half of
Prodrug – inactive drug introduce to the body original value or the amount of drug in the body to
to make active. be reduced by 50%.
Allopurinol – Alloxanthine Loading Dose – one or series of doses that may be
Enalapril – Enalaprilat given at the onset of therapy with the aim of
Chloramphenicol palmitate – achieving the target concentration rapidly.
Chloramphenicol Maintenance Dose – the rate of drug administration
Active metabolites is adjusted such that the rate of input equals to rate
Benzodiazepine Diazepam – Oxazepam loss
Toxic Metabolites
Paracetamol – NAPQI (Hepatotoxicity)/N- PHARMADYNAMICS
acetyl-p-benzoquinone Imine General Mechanism of Drug Action
b. Objective: to make the drug polar, inactive,
Receptor (i.e. antagonist, agonist)
excretable form
Physical (i.e. sunblock)
c. First Pass Metabolism – initial metabolism that
Chemical (i.e. hyperacidity)
happens before the drug reaches the systemic
Physiological (i.e. antibiotic, dimercaprol)
circulation
d. Enzyme Inducers – stimulate expression of Receptor - Like a dynamite
metabolizing enzymes
If drug is prodrug? efficacy and toxicity Single Transduction:
o The drug – receptor complex
If the parent drug is active with inactive
o Receptor State
metabolite? Efficacy
o Major Receptor Families
If with toxic metabolite? Toxicity
A. Ligand – Gated Ion Channels (i.e cholinergic nicotinic
e. Enzyme Inhibitors – Reduce expression of
receptor)
metabolizing enzymes
B. G Protein – Coupled Receptors (i.e. Beta
f. Genetic Polymorphism – genetic differences in
adenoreceptors)
expression of enzymes
C. Enzyme – Linked Receptors (i.e. Insulin Receptors)
g. Categories for enzyme expression:
D. Intracellular Receptors (i.e. Steroid Receptors)
Extensive Metabolizers – produce
normal/adequate amount of enzymes Dose Response Relationship
Ultra-Rapid Metabolizers – produce more than
Graded dose – response relations
the normal amount of enzymes
o Potency – measure of the amount of drug
Poor Metabolizers – Produces less than the
necessary to produce an effect of a given
normal amount of enzymes
magnitude.
4. Elimination (Output) – Final loss of drug from the
o Efficacy – the magnitude of response of a drug
body; elimination = metabolism + excretion.
causes when it interacts with a receptor;
a. Minor:
dependent on the number of drug-receptor
Gastrointestinal Excretion
complexes formed and the intrinsic activity of
Skin – through sweat
the drug.
Mammary Excretion
o Intrinsic Activity - its ability to activate the
b. Major:
receptor and cause a cellular response
Renal excretion – renal excretion processes
Filtration
Tubular Secretion
o NOTE: Efficacy is a more clinically useful Enzyme induction – during metabolism is
characteristic that the drug potency, since a drug accelerated and is cause of therapeutic
with greater efficacy is more therapeutically b. failure. (i.e. of enzyme inducers:
Effect of Drug Concentration on Receptor Binding phenobarbital, phenytoin, carbamazepine,
rifampicin, and St. John’s Wort)
Drug + Receptor = Drug Receptor Complex – Biologic
Enzyme Inhibition – by this biotrans of drugs
effect
is delayed and is cause of increased
The Relationship of Drug Binding to Pharmacology intensity, and sometimes toxicity. (i.e.
Effect cimetidine, Flucazole, Erythromycin,
Ketoconazole, grapefruit juice.)
The magnitude of the response is proportional o Interaction during Excretion – some drugs
to the amount of receptors bound or occupied interact with others of the site of excretion;
The Emax occurs when all receptors are bound probenecid and penecilin interaction
The binding of the drug to the receptor exhibits Pharmacodynamics
no cooperativity o Drug Synergism
Intrinsic Activity Additive Effects – equivalent to the
summation of their individual
1. Full Agonist – mimic endogenous substances; drug pharmacological action A + B = AB
binds to a receptor and produces a biological Potentiation Effects – the net effect of
response that mimics the response to the two drugs used together is greater than
endogenous ligand. the sum of individual effects AB > A + B
2. Partial Agonist – cannot produce the same o Drug Antagonism – opposing actions of two
maximum efficacy as a full agonist drugs on the same physiological system
3. Inverse Agonist – reverse the activity of receptor, o Importance of drug antagonism
and exert the opposite pharmacological effect of Correcting adverse effects of drugs
agonist. Treating drug poisoning
4. Antagonists – binds to a receptor with high affinity Predicting drug combinations which
but possess zero intrinsic activity; can decrease the reduce drug efficacy.
effect of an agonist when present by blocking the o Types of Antagonism
drug’s ability to bind to the receptor; bind allosteric Based on bond formation:
site to change the structure Reversible
Drug Interaction Irreversible
Based on surmountability:
Drug Incompatibility – Serious loss of potency that Competitive
occurs between an infusion fluid and a drug that is Non-Competitive
added to it Based on mechanism:
Pharmaceutical – drug in compatibility – serious loss Pharmacologic Antagonism
of potency that occurs between an infusion fluid and Physiologic Antagonism
a drug that is added to it. Chemical Antagonism
Pharmacokinetics
o Interaction drug absorption – drug may interact
in the gastrointestinal tract resulting in either
decreased or increased absorption
o Interaction during distribution – a drug which is
extensively bound to plasma protein can be
displaced from its sites by another drug or
displacement from other tissue binding sites.
o Interaction during Biotransformation:
You might also like
- Pharmacology Notes #1 DRUG ACTIONDocument4 pagesPharmacology Notes #1 DRUG ACTIONAyumi StarNo ratings yet
- Anatomy and Physiology of The StomachDocument7 pagesAnatomy and Physiology of The StomachEmmi Maliza HutagaolNo ratings yet
- Pharmacology Notes Chapter 1 IntroDocument4 pagesPharmacology Notes Chapter 1 Introridley45No ratings yet
- Anatomy and Physiology of BloodDocument10 pagesAnatomy and Physiology of Bloodaoi_rachelle100% (1)
- Biochem Laboratory Activity 2Document4 pagesBiochem Laboratory Activity 2Kristine PangahinNo ratings yet
- Stool Analysis (D/R) TestDocument8 pagesStool Analysis (D/R) TestAbed AbusalemNo ratings yet
- Demonstration of The Reflex Pathway in FrogsDocument12 pagesDemonstration of The Reflex Pathway in FrogsRuwiniRajakarunaNo ratings yet
- AntibioticsDocument22 pagesAntibioticsEllen Castillo MarianoNo ratings yet
- Respiratory SystemDocument89 pagesRespiratory SystemSuzuke Mae Nijo100% (1)
- CC1 Lab Fin V2Document22 pagesCC1 Lab Fin V2Melody PardilloNo ratings yet
- AntidoteDocument5 pagesAntidoteMaynard ArandaNo ratings yet
- DIGESTIVE SYSTEM BREAKDOWNDocument7 pagesDIGESTIVE SYSTEM BREAKDOWNtheodore_estradaNo ratings yet
- Kidney Nephron Structure and FunctionDocument4 pagesKidney Nephron Structure and Functionxanxan4321No ratings yet
- Common Parasitic Infections - Life Cycles and TreatmentsDocument7 pagesCommon Parasitic Infections - Life Cycles and TreatmentsAj MillanNo ratings yet
- Anatomy and Physiology With Pathophysiology TransesDocument10 pagesAnatomy and Physiology With Pathophysiology Transeshezekiah minNo ratings yet
- Anatomy and physiology of bloodDocument4 pagesAnatomy and physiology of bloodDylle Lorenzo ClaudioNo ratings yet
- Renal Anatomy & Physiology OverviewDocument5 pagesRenal Anatomy & Physiology OverviewChristopher BucuNo ratings yet
- Gram StainDocument5 pagesGram Stainادم PrabowoNo ratings yet
- 35 Drugs Used DyslipidemiaDocument58 pages35 Drugs Used DyslipidemiaNibshian Dela RosaNo ratings yet
- Serum ElectrolytesDocument2 pagesSerum ElectrolytesKervin CablaidaNo ratings yet
- Transfusion TherapyDocument29 pagesTransfusion Therapyoxidalaj100% (3)
- Heparin: A Highly Sulfated Glycosaminoglycan Used as an AnticoagulantDocument14 pagesHeparin: A Highly Sulfated Glycosaminoglycan Used as an Anticoagulantanirbanmanna88320100% (1)
- Hiv & Aids-Related Drugs: Pharma - Semis GutierrezDocument3 pagesHiv & Aids-Related Drugs: Pharma - Semis GutierrezYsabelle GutierrezNo ratings yet
- Hematology: - The Science Dealing With The FormationDocument104 pagesHematology: - The Science Dealing With The FormationYamSomandarNo ratings yet
- Fluids and ElectrolytesBlood TransfusionDocument6 pagesFluids and ElectrolytesBlood TransfusionMaria Erica Jan MirandaNo ratings yet
- (CLINPATH) Lipids and DyslipoproteinemiaDocument5 pages(CLINPATH) Lipids and DyslipoproteinemiaJolaine ValloNo ratings yet
- Pharmacology Notes #1Document2 pagesPharmacology Notes #1Ayumi StarNo ratings yet
- Practical 1-Far 161-FinishDocument10 pagesPractical 1-Far 161-FinishZulkifli Khairuddin100% (1)
- Genitourinary Tract InfectionsDocument80 pagesGenitourinary Tract Infectionsraene_bautistaNo ratings yet
- Pharmacology 1Document53 pagesPharmacology 1Dawn WRein LegaspiNo ratings yet
- Fluid Electrolyte Acid-Base BalanceDocument17 pagesFluid Electrolyte Acid-Base BalanceBethany HoffmanNo ratings yet
- Chap 14 Micropara ReviewerDocument25 pagesChap 14 Micropara RevieweryanNo ratings yet
- Biochemistry JD 2Document6 pagesBiochemistry JD 2failinNo ratings yet
- Microbiology-Specimens CollectionDocument31 pagesMicrobiology-Specimens Collectionapi-253201876100% (1)
- Compilation Medsurg PrelimsDocument29 pagesCompilation Medsurg PrelimsEunice CuñadaNo ratings yet
- FLUIDS AND ELECTROLYTES: MAINTAINING BALANCEDocument13 pagesFLUIDS AND ELECTROLYTES: MAINTAINING BALANCEhahahahaaaaaaa100% (1)
- PL1 3Document2 pagesPL1 3Dennis Valdez80% (5)
- Urinary System and Disorders IntroductionDocument23 pagesUrinary System and Disorders IntroductionHananya ManroeNo ratings yet
- Oral Drug Absorption Factors and ClassificationDocument11 pagesOral Drug Absorption Factors and ClassificationClarilaine JavierNo ratings yet
- Pancreatic Enzymes Help Digest CarbsDocument7 pagesPancreatic Enzymes Help Digest CarbsAngelaAmmcoNo ratings yet
- 10mm Frog Lungbud-AnusDocument11 pages10mm Frog Lungbud-Anusaa628100% (2)
- OsmometryDocument6 pagesOsmometryVERMADEEN0% (1)
- Gastrointestinal Tract System NotesDocument8 pagesGastrointestinal Tract System NotesCarl Elexer Cuyugan Ano100% (1)
- Different Types of VaccinesDocument4 pagesDifferent Types of VaccinesTenisha KnowlesNo ratings yet
- Semen Analysis (Seminal Cytology, Sperm CountDocument30 pagesSemen Analysis (Seminal Cytology, Sperm Countabdurae100% (1)
- PMLS FinalsDocument20 pagesPMLS FinalsPhilipp LibasoraNo ratings yet
- Biochemistry Week 3 - EnzymesDocument6 pagesBiochemistry Week 3 - EnzymesMicah JadeNo ratings yet
- TrematodesDocument9 pagesTrematodesLewis P. SanchezNo ratings yet
- Hematology 2 TEST QUESTIONSDocument4 pagesHematology 2 TEST QUESTIONSa a r o n b a u t i s t aNo ratings yet
- The HIV Life CycleDocument1 pageThe HIV Life Cycleapi-3732057100% (1)
- RBC CountsDocument16 pagesRBC Countsalmastar officeNo ratings yet
- Sporozoa 4Document27 pagesSporozoa 4ebenezermanzanormtNo ratings yet
- MLS312 - Module04 - Explore - Experiment#6 - 0962 - Calpahi - Justine JadeDocument4 pagesMLS312 - Module04 - Explore - Experiment#6 - 0962 - Calpahi - Justine JadeJustine Jade Atew CalpahiNo ratings yet
- The Intestinal NematodesDocument9 pagesThe Intestinal NematodesdhaineyNo ratings yet
- Direct Fecal Smear (Saline and Iodine Wet Mount Preparations)Document6 pagesDirect Fecal Smear (Saline and Iodine Wet Mount Preparations)Tom Anthony TonguiaNo ratings yet
- 1.introduction To PharmacologyDocument127 pages1.introduction To PharmacologyblacknurseNo ratings yet
- Pharmacologic PrinciplesDocument57 pagesPharmacologic PrinciplesYousef Jafar100% (1)
- NCM 106 Drugs and The BodyDocument46 pagesNCM 106 Drugs and The BodyYra JhaneNo ratings yet
- Pharmacology Transes - Unit 1Document13 pagesPharmacology Transes - Unit 1venturaphoenixNo ratings yet
- 3 Principles of Drug Actions and InteractionsDocument6 pages3 Principles of Drug Actions and InteractionsBernardMarkMateoNo ratings yet
- JNC 8Document2 pagesJNC 8ririnrahayumsNo ratings yet
- JNC 8 Guideline Algorithm for Treating HypertensionDocument2 pagesJNC 8 Guideline Algorithm for Treating HypertensionTaradifaNurInsi0% (1)
- CPG GoutDocument2 pagesCPG GoutRomie SolacitoNo ratings yet
- Philippine Clinical Practice Guidelines For The Management of Gout 2008Document7 pagesPhilippine Clinical Practice Guidelines For The Management of Gout 2008JedNo ratings yet
- Antistreptolysin oDocument13 pagesAntistreptolysin oRomie SolacitoNo ratings yet
- Clinical Chemistry: ChlorideDocument2 pagesClinical Chemistry: ChlorideRomie SolacitoNo ratings yet
- Electrolytes PDFDocument8 pagesElectrolytes PDFRomie SolacitoNo ratings yet
- JSC 130010Document14 pagesJSC 130010drprissaNo ratings yet
- Philippine Clinical Practice Guidelines On The Medical Management of Osteoarthritis of The KneeDocument15 pagesPhilippine Clinical Practice Guidelines On The Medical Management of Osteoarthritis of The KneeJames JavierNo ratings yet
- Clinical Chemistry: PotassiumDocument4 pagesClinical Chemistry: PotassiumRomie SolacitoNo ratings yet
- ISBB - Week 3Document8 pagesISBB - Week 3Romie SolacitoNo ratings yet
- Thyroid GlandDocument54 pagesThyroid GlandRomie SolacitoNo ratings yet
- Clinical Chemistry: CalciumDocument5 pagesClinical Chemistry: CalciumRomie SolacitoNo ratings yet
- ISBBDocument26 pagesISBBRomie SolacitoNo ratings yet
- Urine CrystalsDocument4 pagesUrine CrystalsRomie SolacitoNo ratings yet
- Introduction To ParasitologyDocument2 pagesIntroduction To ParasitologyRomie SolacitoNo ratings yet
- Copper Deficiency Anemia and Neutropenia Due To Ketogenic DietDocument11 pagesCopper Deficiency Anemia and Neutropenia Due To Ketogenic DietRomie SolacitoNo ratings yet
- Clinical Hematology Case StudyDocument6 pagesClinical Hematology Case StudyRomie SolacitoNo ratings yet
- Hematoxylin and Eosin ProcedureDocument1 pageHematoxylin and Eosin ProcedureRomie SolacitoNo ratings yet
- Microbiology Case Study: Cryptococcal MeningitisDocument16 pagesMicrobiology Case Study: Cryptococcal MeningitisRomie SolacitoNo ratings yet
- Immuno-Serology & Blood Banking Case Study: Systemic Lupus ErythematosusDocument6 pagesImmuno-Serology & Blood Banking Case Study: Systemic Lupus ErythematosusRomie SolacitoNo ratings yet
- Immuno-Serology & Blood Banking Case StudyDocument8 pagesImmuno-Serology & Blood Banking Case StudyRomie SolacitoNo ratings yet
- Yeast Invasion of Male's Central Nervous SystemDocument9 pagesYeast Invasion of Male's Central Nervous SystemRomie SolacitoNo ratings yet
- Immuno-Serology: Antistreptolysin 0Document13 pagesImmuno-Serology: Antistreptolysin 0Romie SolacitoNo ratings yet
- UIC Medical Laboratory Science Preliminary Defense on Anti-Streptolysin O TestDocument1 pageUIC Medical Laboratory Science Preliminary Defense on Anti-Streptolysin O TestRomie SolacitoNo ratings yet
- DNA to Cells: A Brief History of CytogeneticsDocument5 pagesDNA to Cells: A Brief History of CytogeneticsRomie SolacitoNo ratings yet
- MICROSCOPIC EXAMINATION OF URINE SEDIMENTDocument14 pagesMICROSCOPIC EXAMINATION OF URINE SEDIMENTRomie Solacito100% (1)
- AUBF - PreliminariesDocument5 pagesAUBF - PreliminariesRomie SolacitoNo ratings yet
- Immunology & Serology: Preliminaries: Romie Solacito, MLS3CDocument12 pagesImmunology & Serology: Preliminaries: Romie Solacito, MLS3CRomie Solacito100% (2)
- Manual Videoporteiro Tuya Painel de Chamada 84218Document6 pagesManual Videoporteiro Tuya Painel de Chamada 84218JGC CoimbraNo ratings yet
- P. L. MacKendrick - Roman ColonizationDocument9 pagesP. L. MacKendrick - Roman ColonizationAnyád ApádNo ratings yet
- Lessons From Nothing - Activities For Language Teaching With Limited Time and Resources (Cambridge Handbooks For Language Teachers) 2Document121 pagesLessons From Nothing - Activities For Language Teaching With Limited Time and Resources (Cambridge Handbooks For Language Teachers) 2Ryan Ryan100% (1)
- Electric Expansion Valve: Type ETS 12.5 - ETS 400Document18 pagesElectric Expansion Valve: Type ETS 12.5 - ETS 400Mustafa MouradNo ratings yet
- Housing Typologies & Development in The PhilippinesDocument5 pagesHousing Typologies & Development in The Philippinesmaria lourdes bautista100% (1)
- Importance of Bus Rapid Transit Systems (BRTSDocument7 pagesImportance of Bus Rapid Transit Systems (BRTSAnshuman SharmaNo ratings yet
- Lineas de Inyeccion 320c MaaDocument3 pagesLineas de Inyeccion 320c MaaHAmir Alberto Mojica MojicaNo ratings yet
- DIY Mini CNC Laser EngraverDocument194 pagesDIY Mini CNC Laser EngraverPier DanNo ratings yet
- Zoomorphology: Morphology and Function of The Tube Feet of (Echinodermata: Crinoidea)Document13 pagesZoomorphology: Morphology and Function of The Tube Feet of (Echinodermata: Crinoidea)Indra SatriaNo ratings yet
- Analyze The NatureDocument2 pagesAnalyze The Naturewaril30558No ratings yet
- Lesson Plans: Pre A1 Starters Reading & Writing Part 2 - Teacher's NotesDocument5 pagesLesson Plans: Pre A1 Starters Reading & Writing Part 2 - Teacher's NotesRon ChowdhuryNo ratings yet
- User's Manual: & Technical DocumentationDocument20 pagesUser's Manual: & Technical DocumentationPODOSALUD HUANCAYONo ratings yet
- Autism and Autism Spectrum Disorder Medical Hypothesis For Parasites Influencing AutismDocument3 pagesAutism and Autism Spectrum Disorder Medical Hypothesis For Parasites Influencing AutismCATHYNo ratings yet
- Guidelines For Writing MSC Synopsis or Research ProposalDocument24 pagesGuidelines For Writing MSC Synopsis or Research ProposalFahd100% (1)
- Relative ClausesDocument7 pagesRelative ClausesEvaluna MoidalNo ratings yet
- ConcreteDocument1 pageConcreteRyan_RajmoolieNo ratings yet
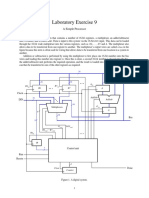
- Laboratory Exercise 9: A Simple ProcessorDocument8 pagesLaboratory Exercise 9: A Simple ProcessorhxchNo ratings yet
- A Formalist Approach To Robert FrostDocument6 pagesA Formalist Approach To Robert FrostAdel75% (4)
- Strategies of Literary TranslationDocument7 pagesStrategies of Literary TranslationMuhammad J H AbdullatiefNo ratings yet
- KA7630/KA7631: Fixed Multi-Output RegulatorDocument6 pagesKA7630/KA7631: Fixed Multi-Output RegulatorTecnico GenioNo ratings yet
- The Role of NNN in Zeolite Acidity and ActivityDocument25 pagesThe Role of NNN in Zeolite Acidity and ActivityRaj MehtaNo ratings yet
- IES VE Parametric Tool GuideDocument7 pagesIES VE Parametric Tool GuideDaisy ForstnerNo ratings yet
- Gartner - Predicts 2021 - Accelerate - Results - Beyond - RPA - To - Hyperautomation-2020Q4Document17 pagesGartner - Predicts 2021 - Accelerate - Results - Beyond - RPA - To - Hyperautomation-2020Q4Guille LopezNo ratings yet
- Class Discussion QuestionsDocument2 pagesClass Discussion Questionshank hillNo ratings yet
- Kyrin Trapp 1st Grade Language Arts Lesson PlanDocument4 pagesKyrin Trapp 1st Grade Language Arts Lesson PlanKyrin TrappNo ratings yet
- 3I'S (Week 7-8)Document15 pages3I'S (Week 7-8)AldrinJosephLacuarinNo ratings yet
- Antacid Booklet Final Sept 2015Document49 pagesAntacid Booklet Final Sept 2015MarianelaMolocheNo ratings yet
- HP Police Constable Question Paper 2015Document9 pagesHP Police Constable Question Paper 2015Rajat SharmãNo ratings yet
- Assignment IDocument4 pagesAssignment IDylan HsiehNo ratings yet
- 9.36 Project Summary FormDocument2 pages9.36 Project Summary FormTu Burin DtNo ratings yet