Professional Documents
Culture Documents
The Psychiatric History: Functions and Components
Uploaded by
Keifer TurtleOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Psychiatric History: Functions and Components
Uploaded by
Keifer TurtleCopyright:
Available Formats
2.
01 The Psychiatric History
Dr. Luis Sundiang | September 25, 2017
PSYCHIATRY
OUTLINE Help patient cope with his situation
Suggest changes to improve prognosis and minimize future
I. Functions of a Medical Interview risks
A. Assess Nature of the Problem
B. Develop and Maintain a Therapeutic D.MENTAL STATE EXAMINATION (from University of Bristol
Relationship Website: http://www.bristol.ac.uk/medical-
C. Communicate Information and Implement a school/hippocrates/psychiatry/mse_etc/ )
Treatment Plan This part is for the next lesson but the lecturer included it in ppt
D. Mental State Examination
II. Psychiatry history taking - Enables you to understand what your patient is
A. Introduction and Presenting Complaint experiencing.
B. Past Psychiatric history - Involves the following:
C. Past Medical history
D. Family history 1. Appearance and Behavior
E. Personal history o Involves objective observation your patient from
F. Premorbid personality
G. Difficult questions the first meeting and record the observations
H. Risk assessment accurately in less than 30 words
III. Components of Psychiatric History o Physical Appearance
A. Identifying data body build, (nutritional state)
B. Chief Complaint significant distinguishing features
C. Source and Reliability cleanliness (hair, teeth, nails)
D. History of Present Illness
Quality, style and state of clothing
E. Past Medical and Psychiatric History
F. Family history o General Attitude
G. Social History rapport
H. Anamnesis/Personal History attitude towards interview
IV. Quiz eye contact
o Motor Behavior
LEGEND restless, fidgety or apathetic, retarded
2. Speech
Remember Textbook Trans Editor Previous Trans
o Volume and speed
pressure of talk <-> retardation
o Construction
OBJECTIVES:
flight of ideas, rhyming, punning,
1. Know the functions and purpose of psychiatric interview and
incoherence
examination
o Enunciation
2. Learn the content and process of taking a psychiatric history
dysarthria, stammer
3. Integrate psychiatric history taking in your medical/ surgical
3. Mood or Affective State
interview and examination
o Subjective experience (ask!)
o objective impression
I. FUNCTIONS OF A MEDICAL INTERVIEW
elevated, euthymic, low, angry, cheerful,
A. ASSESS NATURE OF THE PROBLEM
distraught, despondent, resentful
Diagnose o congruity with speech content
Determine appropriate diagnostic procedures if warranted o stability
Formulate and propose management o emotional reactivity
Provide information on course and outcome o suicidal ideation or intent
4. Thoughts
B. DEVELOP AND MAINTAIN A THERAPEUTIC RELATIONSHIP o Content
(Establishing a Therapeutic Relationship) preoccupations?
Facilitate patient’s collaboration in diagnostic and treatment ideas of reference?
activities delusions?
Maintain flow of information exchange recurring, pervasive theme,
Relieve patient’s distress and suffering depressive ruminations
Provide satisfaction for patient and doctor grandiose ideas
self-referential ideation
C. COMMUNICATE INFORMATION AND IMPLEMENT A o obsessional thoughts
TREATMENT PLAN How to probe for obsessional thoughts (+
Help patient understand illness, diagnostic procedures, compulsive rituals): “Some people find
treatments, risks and outcome they have unpleasant and unwanted
Establish and maintain consensus with patient and facilitate thoughts or images coming into their
informed consent
GROUP #1: Eleazar M., Elefante, Elgar, Esperanza, Espinosa
EDITOR/S: Surname (Cellphone#) 1 of 5
mind, which can’t be resisted. Has that “Do you feel puzzled by strange
been a problem?” happenings that are difficult to account
o objective signs of thought disorder for?”
o subjective experience of thought disorder “Do familiar surroundings seem
Probing questions: “Can you think quite strange?”
clearly, or does there seem to be some 7. Cognition
kind of interference with your thoughts?” o Level of consciousness
Thought withdrawal: “Are your thoughts o Orientation
actually taken out or sent out of your Time, Place, Personal Identity
mind? Do they actually feel like that? So o Attention and concentration
that they are outside your head?” Test: Serial Sevens, months in reverse
Thought insertion: “Do there seem to be o Memory
thoughts in your mind which are not your immediate recall: digit span
own; which seem to come from recent: address
somewhere else?” remote: Personal History!
Thought broadcasting: “Do your thoughts o General knowledge + intelligence
seem to be somehow public; not private 8. Insight
to yourself, so that others can know what o Attitude towards illness
you are thinking?” “How do you see your difficulties?”
5. Perceptions “Do you feel there is something wrong
o defined as the ability to perceive the outside world with your nerves?”
that could be related to a complex, o Attitude towards treatment
neuropsychological process which involves the “What sort of treatment do you feel is
ability of the sense organs to detect and modulate needed?”
the raw data of our senses (sight, smell, noise), “How do you feel about: being in hospital
and the ability of the brain to decode that / taking tablets?”
information and produce an internal neuronal
representation of the outside world. II. PSYCHIATRY HISTORY TAKING
o to the person experiencing a hallucination, the (from University of Bristol Website: http://www.bristol.ac.uk/medical-
perception is real school/hippocrates/psychiatry/mse_etc/ )
o Auditory hallucinations: It is a clinical history in itself but with an in depth coverage of social
Get an exact description!! and developmental history.
Familiar or unfamiliar voices?
2nd or 3rd person? A. Introduction, Presenting Complaint and its History
Do the voices give commands? Keep it short and simple
If so, how does the patient react? If appropriate, use patients own word
o How to probe for auditory hallucinations: List relevant event leading up to the present problem
“We ask this question routinely of Knowledge of specific disorders required
everyone, because sometimes people
under stress seem to hear noises or B. Past Psychiatric and Medical History
voices when there is nobody around and
This includes treatment and admissions
no ordinary explanation is possible. Has
Either informal or under section
anything like this ever happened to you?”
o Loud thoughts (Gedankenlautwerden) Ask any previous episodes of deliberate self harm
“Do your thoughts seem to sound aloud If very long, summarize
in your head, almost as if somebody
standing near you could hear them?” C. Family History
o Thought echo (Écho de la pensées) Use genograms
"Does a thought in your mind seem to be Ask about their occupations and social status
repeated over again, like an echo?” Ask if there are family members with mental health problems
6. Delusions Ask if there are any suicides and suicide attempts among
o defined as a false, unshakable idea or belief which family members
is out of keeping with the patient's educational,
cultural and social background; it is held with D. Personal History I
extraordinary conviction and subjective certainty Early Child Hood
o can be: o Place and circumstances of birth
primary: ideas that arise are fully formed o Early milestone and development
secondary: attempt by the patient to o Family atmosphere and moves
make sense of their experiences Education
o How to probe for delusions: o Schools Attended
“Have you had the feeling that something o Attitudes to school
odd is going on that you can’t explain?” o Regularity of attendance
o Exams passed, age at leaving
[PYSCH] 2.01 The Psychiatric History 2 of 5
Occupational History Risk of violence
o Details of jobs o Not common
o Reasons for finding another job if applicable o Check if there is a history of violence
o Ask if they carry a weapon and ask them not to
E. Personal History II come to the hospital with weapons
Psychosexual Development o Paranoid delusion (misinterpretation of innocent
o Tailor to what’s appropriate and needed gesture as threatening; belief that they are in
o Orientation danger and being threatened; delusional voices
o Relationships that tells them to hurt another person)
o Family attitudes and instruction o Jealousy – very powerful emotion that can lead to
o First experiences violence
Present Social Circumstances
o Own or rented accommodations III. COMPONENTS OF THE PSYCHIATRIC HISTORY
o Financial problems, debts (this part is as presented by Dr. Sundiang in his lecture ppt)
Drug History The patient history is based on the subjective report of the
o Prescribed patient and in some cases the report of collaterals including
Asked for the dose and duration other health care providers, family and other caregivers
Compliance and check for side effects (Kaplan & Sadock).
o Illicit drug and alcohol use Notes:
Useful screening tool Below are the parts of the Initial Psychiatric Interview (in the
Be prepared to explore all features of book it is called initial psychiatric interview while Dr. Sundiang
dependency if necessary called it psychiatric history) based on Kaplan and Sadock:
Forensic History I. Identifying data
o We live in the age of risk assessment II. Source and reliability
o “Have you ever had any trouble with the police?” III. Chief Complaint
o History of violence IV. Present Illness
Get all the details, if present V. Past psychiatric history
Distinguish between violence against VI. Substance use/abuse
property or people VII. Past medical History
VIII. Family history
F. Premorbid Personality IX. Developmental and Social history
“When you are well, …” X. Review of Systems
Volition XI. Mental status examination
o “…how (what kind of person would you XII. Physical Examination
describe yourself?” XIII. Formulation
Mood XIV. DSM-5 diagnoses
o “… what’s your usual mood like?” XV. Treatment plan
Social
o “… how do you get on with other people?” A. Identifying Data
Cognitive This includes patient’s name, age, marital status, sex,
o (intellectual capacity) general knowledge handedness, occupation, nationality, birth order, religion,
Reaction patterns to stress educational attainment and living conditions
o “… how do you react to stress?” Ask also if this is the patient’s first admission or if the patient
has past admissions already
G. Risk Assessment
Risk of suicide B. Chief Complaint
o Symptoms of depression Verbatim: in the patient’s own words
o Ask if they are attempting suicide
Why he or she has come or been brought in for consult
o If there is risk of suicide, arrange appointment
Must be brief
o Manage the course of suicide
o Treat depression
C. Source and Reliability
o Can be cause by substance abuse and alcohol
abuse The other individuals present as collateral sources of
o Consider patient’s situation (marital problem, information
financial problem, and others) Write reliability of the sources as well
Risk of self-harm Patient’s pre-morbid and morbid personality
o Common (30%) D. History of Present Illness
o Use as a way to regulate their emotions Comprehensive and chronological picture of the events
o Develop collaborative relationship and find an leading up to the current moment in the patient's life
alternative way like being mindfulness by The account should include any other changes that have
encouraging them to express their emotional occurred during this same time period in the patient’s
feelings
[PYSCH] 2.01 The Psychiatric History 3 of 5
interests, interpersonal relationships, behaviors, personal
habits and physical health E. Social History
Include all significant symptomatology, precipitating factors, Substance abuse – history should include which substances
significant modifiers of the illness have been used, including alcohol, drugs, medications
o Possible organic factors, drug, and alcohol abuse (prescribed or not prescribed to the patient), and routes of
Pertinent positive and negative symptoms use. The frequency and amount of use should be
“Can you tell me in your own words what brings you here determined, keeping in mind the tendency for patients to
today?” minimize or deny use that may be perceived as socially
unacceptable
E. Past Medical and Psychiatric History o Smoking, alcohol, illicit drug use
Past Medical History Smoking: in pack-years
o Any medical, surgical, or obstetric problems the Alcohol: type of alcohol, how frequent, shared
patient has or had among friends, CAGE criteria
Medications (with doses) currently being Drugs: First use? Who influenced the patient
taken to use drugs? How often? How much? Effects
Treatments must also be included (anong klaseng “tama”), when was the last
o Hospitalizations use?
o Allergies to food and drugs G. Anamnesis/Personal History
o Past medical history is an important consideration In Kaplan and Sadock, this part is under developmental and
when determining potential causes of mental social history
illness as well as comorbid or confounding factors It is an important tool in determining the context of
and may dictate potential treatment options or psychiatric symptoms and illness and may, in fact, identify
limitations. some of the major factors in the evolution of the disorder
o Medical illness can precipitate a psychiatric Outline of a developmental History
disorder o Prenatal and Perinatal – developmental
Past Psychiatric History milestones should be noted
o Psychiatric diagnosis Full-term pregnancy or premature
Past suicide attempts Vaginal delivery or caesarean
o Psychiatric treatment Drugs taken by mother during pregnancy
When was the medication given? (prescription and recreational)
Duration? Dose? Therapeutic and Birth complications
adverse effects? Defects at birth
Psychotherapy, ECT Wanted/Unwanted and Planned/Unplanned
Admission at an in-patient facility? OPD Pregnancy
consult? Rehab center? o Infancy and Early Childhood
Consult with other mental health Birth – 3 years
professionals (psychologist, social Infant-mother relationship
worker, counselors) Problems with feeding and sleep
o Written records from institutions and past Significant milestones
caregivers may be considered Standing/walking
First words/two-word sentences
F. Family History Bowel and bladder control
Because many psychiatric illnesses are familial and a Other caregivers
significant number of those have a genetic predisposition, if Unusual behaviors (e.g., head-banging)
not cause, a careful review of family history is an essential o Middle childhood (3-11yrs)
part of the psychiatric assessment. Preschool and school experiences
A genogram is often useful for clarity Separations from caregivers
o To look for similar conditions in other family Friendships/play
members, as well as their treatment and Methods of discipline
responses Illness, surgery, or trauma
Medical, psychiatric, and substance abuse o Late Childhood and Adolescence
o Suicide attempts or completed suicide in the family Onset of puberty
List the psychotropic medications Academic achievement
o Which ones are effective vs not effective Organized activities (sports, clubs)
Family dynamics must also be taken into account Areas of special interest
o Who are the members living together? Romantic involvements and sexual
o Quality of relationship experience
Who is closest to the patient? Who is in Work experience
conflict with the patient? Drug/alcohol use
How the family members interact with Symptoms (moodiness, irregularity of
one other sleeping or eating, fights and arguments)
o Reactions to illness, support given
[PYSCH] 2.01 The Psychiatric History 4 of 5
o Young adulthood
Meaningful long-term relationships
Marital history
Sexual history
Academic and career decisions
Military experience
Work history
Prison/ Legal experience
Intellectual pursuits and leisure activities
Religion
Fantasies and Dreams
o Middle adulthood and old age
Changing family constellation
Social activities
Work and career changes
Aspirations
Major losses
Retirement and aging
REFERENCES
Lecture slides
Synopsis of Psychiatry 11th Ed. Kaplan and Sadock
http://www.bristol.ac.uk/medical-
school/hippocrates/psychiatry/mse_etc/
MINI-QUIZ
1. Which of the following statements is TRUE regarding psychiatric
interview?
a. The interview is the most important element in the
evaluation and care of persons with mental illness
b. A well conducted interview results in an understanding of
the neurobiological elements of the disorder
c. The results of which is usually confirmed by laboratory
testing and imaging
d. All of the above
2. Which of the following is NOT included in the identifying data?
Previous medications
b. Marital status
c. Occupation
d. Number of consults
3. Which of the following is FALSE regarding the chief complaint?
a. Recording should be done in a verbatim manner
b. Usually obtained only from the patient
c. It is the patient’s primary concern for consult
d. All of the above statements are true regarding chief
complaint
4. Anamnesis refers to:
a. Family history
b. Sexual history
c. Personal history
5. The purpose of the interview in history taking is
a. To gather information that will enable the examiner to
make a diagnosis and plan for treatment accordingly
b. To help the physician decide if the patient should be
admitted or sent home
c. To be able to know the latest events in the patient’s life
d. To be able to comfort and allow the patient to ventilate his
frustrations in life
ANSWERS: AABCA
[PYSCH] 2.01 The Psychiatric History 5 of 5
You might also like
- Psychiatric History and ExaminationDocument14 pagesPsychiatric History and ExaminationPaolo Bonifacio100% (13)
- Assessment and Evaluation: 2008 Edition Rhoda K Hahn, MD Lawrence J. Albers, MDDocument85 pagesAssessment and Evaluation: 2008 Edition Rhoda K Hahn, MD Lawrence J. Albers, MDAlbghdadi CristianNo ratings yet
- Clinical Evaluation of The Psychiatric PatientDocument4 pagesClinical Evaluation of The Psychiatric Patienthannjazz100% (1)
- Psych CardsDocument10 pagesPsych CardsJennifer Rodriguez95% (21)
- Patient Write-Up Example 2Document6 pagesPatient Write-Up Example 2Meliara101No ratings yet
- Psychiatry History Taking and Physical ExaminationDocument16 pagesPsychiatry History Taking and Physical ExaminationEma100% (17)
- Psychiatric History - MSEDocument7 pagesPsychiatric History - MSEDeepbluex100% (1)
- Psychiatric Mental Health Comprehensive Case StudyDocument14 pagesPsychiatric Mental Health Comprehensive Case Studyapi-546967314No ratings yet
- H&P Template SummaryDocument1 pageH&P Template SummaryWilliam Yang100% (1)
- Lab Monitoring For Psychiatric Medications: Reference TableDocument1 pageLab Monitoring For Psychiatric Medications: Reference TableTimothy Turscak100% (1)
- Psychiatric Mental Health Comprehensive Case StudyDocument13 pagesPsychiatric Mental Health Comprehensive Case Studyapi-546220765No ratings yet
- Clinical Interview For Psychiatric AssessmentDocument63 pagesClinical Interview For Psychiatric Assessmentaadupavi100% (1)
- Psychiatry HX TakingDocument4 pagesPsychiatry HX TakingP KasikrishnarajaNo ratings yet
- Mental Status Exam of Patient with Psychiatric HoldDocument4 pagesMental Status Exam of Patient with Psychiatric HoldJoan ChoiNo ratings yet
- Psychiatric EvaluationDocument3 pagesPsychiatric EvaluationLana AmerieNo ratings yet
- PSYCH 1.2A Mood DisordersDocument22 pagesPSYCH 1.2A Mood DisordersZazaNo ratings yet
- 7718 (07) Review of Cases - Anxiety DisordersDocument34 pages7718 (07) Review of Cases - Anxiety DisordersnewazNo ratings yet
- Antipsychotic Medication: Generic Name Trade Name Indications Contraindications Drug Interaction Side Effects Nursing ImplicationDocument6 pagesAntipsychotic Medication: Generic Name Trade Name Indications Contraindications Drug Interaction Side Effects Nursing ImplicationJaylord VerazonNo ratings yet
- Mental Status Examination Rapid Record Form: CatatoniaDocument3 pagesMental Status Examination Rapid Record Form: CatatoniaNicole TangcoNo ratings yet
- Varun Kumar, 2017 - Getting Started in PsychiatryDocument148 pagesVarun Kumar, 2017 - Getting Started in PsychiatryBernard FZ100% (1)
- HPI GuidelinesDocument5 pagesHPI GuidelinesHani NadiahNo ratings yet
- Psychiatric History SummaryDocument24 pagesPsychiatric History SummaryfahmiNo ratings yet
- 10 Cognitive DisordersDocument16 pages10 Cognitive DisordersFarrah MaeNo ratings yet
- Quick Reference Guide April 2019 PDFDocument2 pagesQuick Reference Guide April 2019 PDFAaron ShokarNo ratings yet
- Elements of The Psychiatric Assessment: Chief ComplaintDocument4 pagesElements of The Psychiatric Assessment: Chief ComplaintRaissa100% (1)
- 1.02 Psychiatric History and Mental Status Examination PDFDocument4 pages1.02 Psychiatric History and Mental Status Examination PDFEp-ep Jeffrey Sibayan Ramos100% (1)
- Disorders Duration/Onset Symptoms/Manifestations Treatment: Childhood DDocument7 pagesDisorders Duration/Onset Symptoms/Manifestations Treatment: Childhood DActeen Myoseen100% (1)
- Commonly Prescribed Psychotropic MedicationsDocument2 pagesCommonly Prescribed Psychotropic MedicationsDragutin PetrićNo ratings yet
- Elements of The Psychiatric AssessmentDocument5 pagesElements of The Psychiatric AssessmentdevNo ratings yet
- PsychiatryDocument95 pagesPsychiatryJarwoto RoestanajieNo ratings yet
- Case Presentation StyleDocument7 pagesCase Presentation StyleNiteshSinghNo ratings yet
- Psych-CLEAR: Psychopathology Made Clear and EasyDocument31 pagesPsych-CLEAR: Psychopathology Made Clear and EasynurulNo ratings yet
- 504 - Pediatric Psychopharmacology - General PrinciplesDocument54 pages504 - Pediatric Psychopharmacology - General PrinciplesAlvaro HuidobroNo ratings yet
- Psychiatry Notes Psychiatry Notes: Medicine (Queen Mary University of London) Medicine (Queen Mary University of London)Document28 pagesPsychiatry Notes Psychiatry Notes: Medicine (Queen Mary University of London) Medicine (Queen Mary University of London)Noman ButtNo ratings yet
- Psychiatric Evaluation Comprehensive SkeletonDocument4 pagesPsychiatric Evaluation Comprehensive SkeletonThomasean BrittenNo ratings yet
- Psychiatry Note BookDocument37 pagesPsychiatry Note BookMustafa Kamal BangashNo ratings yet
- DSM-IV Criteria MnemonicsDocument4 pagesDSM-IV Criteria Mnemonicsleonyap100% (1)
- Psych DrugsDocument3 pagesPsych DrugsSwarna BanikNo ratings yet
- Antipsychotics Mechanisms Indications SideEffectsDocument4 pagesAntipsychotics Mechanisms Indications SideEffectsRana MuhammadNo ratings yet
- Psychiatry textbook and reference guide collectionDocument4 pagesPsychiatry textbook and reference guide collectionIbrahimFikryNo ratings yet
- Janice Krug PMHNP ResumeDocument3 pagesJanice Krug PMHNP Resumeapi-416722296No ratings yet
- Drug List PsychopharmDocument23 pagesDrug List PsychopharmGeorge HananiaNo ratings yet
- PMH Nursing GuideDocument11 pagesPMH Nursing Guidejwasylow13No ratings yet
- 02 - 24 - Psychiatric Assessment PDFDocument7 pages02 - 24 - Psychiatric Assessment PDFAbi Sulit100% (1)
- Algorithm for Treating DepressionDocument12 pagesAlgorithm for Treating Depressioniwul kiwul KriwulNo ratings yet
- Psychiatry NotesDocument123 pagesPsychiatry NotesKyoheirwe vanessaNo ratings yet
- Psychiatric History and Mental Status Examination GuideDocument7 pagesPsychiatric History and Mental Status Examination GuideGabriel Gerardo N. Cortez100% (1)
- Psychiatric Assessment ToolDocument53 pagesPsychiatric Assessment ToolLori100% (3)
- Dopamine HypothesisDocument2 pagesDopamine HypothesisBo123456100% (2)
- Practical Psychopharmacology in Children and Adolescents: Anoop Vermani MD Fellow, Child and Adolescent PsychiatryDocument29 pagesPractical Psychopharmacology in Children and Adolescents: Anoop Vermani MD Fellow, Child and Adolescent PsychiatryShahinaz ShamsNo ratings yet
- Mobile Clinic Mobile PSE GuideDocument18 pagesMobile Clinic Mobile PSE GuideFrancisco Javier Salazar Núñez100% (1)
- NRNP PRAC 6665 and 6675 Focused SOAP Note ExemplarDocument6 pagesNRNP PRAC 6665 and 6675 Focused SOAP Note ExemplarLogan ZaraNo ratings yet
- Psychiatry Practice Boosters 2016: Insights from research to enhance your clinical workFrom EverandPsychiatry Practice Boosters 2016: Insights from research to enhance your clinical workNo ratings yet
- Prescribing Psychotropics: From Drug Interactions to PharmacogeneticsFrom EverandPrescribing Psychotropics: From Drug Interactions to PharmacogeneticsRating: 5 out of 5 stars5/5 (1)
- The Maudsley Prescribing Guidelines in PsychiatryFrom EverandThe Maudsley Prescribing Guidelines in PsychiatryRating: 5 out of 5 stars5/5 (1)
- Psychiatry Practice Boosters, Second Edition: Insights from research to enhance your clinical workFrom EverandPsychiatry Practice Boosters, Second Edition: Insights from research to enhance your clinical workNo ratings yet
- Revelations 2020 - 2133: Bertha Dudde Book 30Document28 pagesRevelations 2020 - 2133: Bertha Dudde Book 30Pavel VelcotăNo ratings yet
- Critical Thinking Nurse 1Document4 pagesCritical Thinking Nurse 1indah Purnama sariNo ratings yet
- Chapter 01 What Is Social PsychologyDocument29 pagesChapter 01 What Is Social PsychologyLarryNo ratings yet
- 000 2021 FIBAA Selfdocumentation - 09.06Document47 pages000 2021 FIBAA Selfdocumentation - 09.06Chandler M. Bing100% (1)
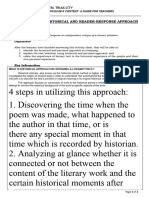
- Info Sheet g10 QRTR 3 Lesson 7 Histo Reader Response 1Document2 pagesInfo Sheet g10 QRTR 3 Lesson 7 Histo Reader Response 1preciouspurple.marquezNo ratings yet
- Bsed-Filipinno Educ110 PortfolioDocument64 pagesBsed-Filipinno Educ110 PortfolioRichelle MendozaNo ratings yet
- - Analysis of the Extract to Sir, With Love (Аракин, 3 Курс)Document3 pages- Analysis of the Extract to Sir, With Love (Аракин, 3 Курс)Mohammed Israr ShaikhNo ratings yet
- Navajo Philosophy of LearningDocument4 pagesNavajo Philosophy of Learningraindeer667No ratings yet
- Teaching Creativity Skills in Primaryuagc2013Document6 pagesTeaching Creativity Skills in Primaryuagc2013Iancu CezarNo ratings yet
- Migration Process Impacts on Migrants and RefugeesDocument25 pagesMigration Process Impacts on Migrants and RefugeesCherif ChokeirNo ratings yet
- Law of PhilosophyDocument21 pagesLaw of PhilosophyKareen Baucan100% (1)
- Example of An Informative Thesis StatementDocument7 pagesExample of An Informative Thesis Statementfjbnd9fq100% (2)
- Use Your IntuitionDocument24 pagesUse Your IntuitionDajana Posavcic100% (1)
- International Business 16th Edition Daniels Test Bank DownloadDocument28 pagesInternational Business 16th Edition Daniels Test Bank DownloadChristina Walker100% (27)
- The Third House: Cyclical MeaningDocument3 pagesThe Third House: Cyclical MeaningHamida Eugenia GabrielliNo ratings yet
- MC 4 Logic and Critical ThinkingDocument6 pagesMC 4 Logic and Critical Thinkingkenchavez08No ratings yet
- Formulating Extended Identity Theory' For Twenty - First Century Social Sciences Research: Modeling Extended Identity in Relation To Real - World Observations and DataDocument37 pagesFormulating Extended Identity Theory' For Twenty - First Century Social Sciences Research: Modeling Extended Identity in Relation To Real - World Observations and DataInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Michael F. - Junguian Psychotherapy PDFDocument20 pagesMichael F. - Junguian Psychotherapy PDFSergio Nahat100% (1)
- Being Myself - Rupert SpiraDocument57 pagesBeing Myself - Rupert SpiraguzmaNo ratings yet
- William James' Theory of the SelfDocument5 pagesWilliam James' Theory of the SelfRAYMUND QUIGTARNo ratings yet
- Pearson Effective Questioning in TGFUDocument10 pagesPearson Effective Questioning in TGFUGwee ShiannHerngNo ratings yet
- 4-Logic Chpter 4 Basic Concepts of Critical ThinkingDocument25 pages4-Logic Chpter 4 Basic Concepts of Critical ThinkingYasinNo ratings yet
- Interpersonal vs Intrapersonal Communication SkillsDocument20 pagesInterpersonal vs Intrapersonal Communication Skillsabh ljknNo ratings yet
- BernsteinDocument19 pagesBernsteinJoseline VegaNo ratings yet
- BordenAmy ETD 2010【翻译狗www.fanyigou.com】Document325 pagesBordenAmy ETD 2010【翻译狗www.fanyigou.com】Webber TangNo ratings yet
- Pca-Educación Básica Superior Intensiva-InglésDocument5 pagesPca-Educación Básica Superior Intensiva-InglésCLEVER FAREZNo ratings yet
- 10 Stage Counsellee ExperienceDocument11 pages10 Stage Counsellee ExperienceUmar MasoodNo ratings yet
- Watch the movie "7 SundaysDocument4 pagesWatch the movie "7 SundaysQueenie Carale100% (2)
- ICT MOOC Unit 4 Packet - Winter 2023Document31 pagesICT MOOC Unit 4 Packet - Winter 2023Bùi TuấnNo ratings yet
- Sla 22Document7 pagesSla 22api-604277894No ratings yet