Professional Documents
Culture Documents
Recurrence of Bacterial Vaginosis Is Significantly
Uploaded by
tunihaaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Recurrence of Bacterial Vaginosis Is Significantly
Uploaded by
tunihaaCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/233931571
Recurrence of Bacterial Vaginosis Is Significantly Associated With
Posttreatment Sexual Activities and Hormonal Contraceptive Use
Article in Clinical Infectious Diseases · December 2012
DOI: 10.1093/cid/cis1030 · Source: PubMed
CITATIONS READS
57 84
9 authors, including:
Catriona S Bradshaw Lenka A Vodstrcil
Monash University (Australia) University of Melbourne
319 PUBLICATIONS 4,606 CITATIONS 95 PUBLICATIONS 846 CITATIONS
SEE PROFILE SEE PROFILE
Jane Hocking Suzanne M Garland
University of Melbourne Royal Women's Hospital in Victoria
424 PUBLICATIONS 7,130 CITATIONS 854 PUBLICATIONS 22,078 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Vaccination for HPV among MSM View project
VACCINE study View project
All content following this page was uploaded by Catriona S Bradshaw on 26 October 2016.
The user has requested enhancement of the downloaded file.
MAJOR ARTICLE
Recurrence of Bacterial Vaginosis Is
Significantly Associated With Posttreatment
Sexual Activities and Hormonal Contraceptive
Use
Catriona S. Bradshaw,1,5,6,a Lenka A. Vodstrcil,1,a Jane S. Hocking,1,2 Matthew Law,9 Marie Pirotta,3
Suzanne M. Garland,4,7,8,10 Deborah De Guingand,1 Anna N. Morton,5 and Christopher K. Fairley1,5
1
Melbourne School of Population Health, 2Center for Women's Health, Gender and Society, and Departments of 3General Practice and 4Obstetrics and
Gynaecology, University of Melbourne, 5Melbourne Sexual Health Centre, The Alfred Hospital, 6Department of Epidemiology and Preventive Medicine,
Monash University, 7Department of Microbiology and Infectious Diseases, The Royal Women’s Hospital, and 8Department of Microbiology, The Royal
Downloaded from http://cid.oxfordjournals.org/ by guest on October 26, 2016
Children’s Hospital, Melbourne; 9The Kirby Institute, University of New South Wales, Darlinghurst; and 10Murdoch Children’s Research Institute,
Parkville, Australia
(See the Editorial Commentary by Marrazzo on pages 787–9.)
Background. Bacterial vaginosis (BV) recurrence posttreatment is common. Our aim was to determine if be-
haviors were associated with BV recurrence in women in a randomized controlled trial (RCT).
Methods. Symptomatic 18- to 50-year-old females with BV (≥3 Amsel criteria and Nugent score
[NS] = 4–10) were enrolled in a 3-arm randomized double-blind RCT Melbourne Sexual Health Centre, Australia,
in 2009–2010. All 450 participants received oral metronidazole (7 days) and were equally randomized to vaginal
clindamycin, lactobacillus-vaginal probiotic or vaginal placebo. At 1, 2, 3, and 6 months, participants self-collected
vaginal smears and completed questionnaires. Primary endpoint was NS = 7–10. Cox regression was used to esti-
mate hazard ratios (HRs) for risk of BV recurrence associated with baseline and longitudinal characteristics.
Results. Four hundred four (90%) women with postrandomization data contributed to analyses. Cumulative
6-month BV recurrence was 28% (95% confidence interval [CI], 24%–33%) and not associated with treatment.
After stratifying for treatment and adjusting for age and sex frequency, recurrence was associated with having the
same pre-/posttreatment sexual partner (adjusted HR [AHR] = 1.9; 95% CI, 1.2–3.0), inconsistent condom use
(AHR = 1.9; 95% CI, 1.0–3.3), and being non-Australian (AHR = 1.5; 95% CI, 1.0–2.1), and halved with use of
an estrogen-containing contraceptive (AHR = 0.5; 95% CI, .3–.8).
Conclusions. Risk of BV recurrence was increased with the same pre-/posttreatment sexual partner and in-
consistent condom use, and halved with use of estrogen-containing contraceptives. Behavioral and contraceptive
practices may modify the effectiveness of BV treatment.
Clinical Trials Registration. ACTRN12607000350426.
Keywords. bacterial vaginosis; contraceptive use; estrogen; sexual partner; condom use.
Received 31 July 2012; accepted 5 October 2012; electronically published 12
December 2012.
Bacterial vaginosis (BV) is the commonest cause of ab-
a
C. S. B. and L. A. V. contributed equally to this work. normal vaginal discharge in reproductive-age women,
Correspondence: Catriona S. Bradshaw, MD, PhD, Melbourne Sexual Health
Centre, 580 Swanston St, Carlton, VIC 3053, Australia (cbradshaw@mshc.org.au).
affecting 29% of 14- to 49-year-old North American
Clinical Infectious Diseases 2013;56(6):777–86
women in the National Health and Nutrition Survey [1],
© The Author 2012. Published by Oxford University Press on behalf of the Infectious and 12% of 17- to 28-year-old Australian women
Diseases Society of America. All rights reserved. For Permissions, please e-mail:
journals.permissions@oup.com.
attending general and sexual health practices [2]. Al-
DOI: 10.1093/cid/cis1030 though the etiology of BV is unclear, next-generation
Behaviors Associated With BV Recurrence • CID 2013:56 (15 March) • 777
sequencing methods have advanced our understanding of this in 450 women from December 2007 through May 2010 at
complex polymicrobial condition, with high bacterial species Melbourne Sexual Health Centre, Australia [17]. Participants
diversity reported in women with BV compared to normal received 400 mg of oral metronidazole twice daily for 7 days
flora, and increasing numbers of specific noncultivable BV- and were randomized to 1 of 3 vaginal interventions: placebo,
associated bacteria (BVAB) being described [3]. Two of the com- 2% clindamycin cream, or a commercially available estriol-
monest BVAB, Gardnerella vaginalis and Atopobium vaginae, and Lactobacillus-containing probiotic. This study has been
contribute to a vaginal biofilm associated with BV, which described in detail elsewhere [17]. In brief, 18- to 50-year-old
rapidly reaccumulates following antibiotic therapy [4, 5]. women were eligible if they had abnormal vaginal discharge or
Epidemiologic studies consistently report an association odor with ≥3 Amsel criteria and a Nugent score (NS) = 4–10.
between BV and sexual activity. In a study of young women, Women were ineligible if positive for human immunodeficien-
BV was strongly associated with penile-vaginal sex, was rare in cy virus (HIV), pregnant, breastfeeding, or unable to use
women only engaging in noncoital practices, and was absent condoms/abstain from sex during vaginal treatment.
in women reporting no sexual contact with others [6]. BV was At baseline, participants were examined by a clinician,
associated with increased numbers of sexual partners and Nugent and Amsel scores were documented, and paper-based
inconsistent condom use in a meta-analysis [7], and BVAB questionnaires were completed recording demographic, behav-
and BV-associated biofilms have been detected in the male ioral, clinical, and contraceptive data. After treatment, women
coronal sulcus and urine [8–10]. Most researchers concur that completed questionnaires and self-collected vaginal smears and
BV is associated with sexual activity, but whether this is returned specimens by mail at 1, 2, 3, and 6 months or until
Downloaded from http://cid.oxfordjournals.org/ by guest on October 26, 2016
because of transmission of BVAB between partners or because BV recurrence. The primary endpoint was BV recurrence,
sexual activity adversely impacts on colonization with protec- defined as an NS of 7–10 at any interval after treatment, at
tive Lactobacillus species is unknown [11]. which point participants were offered retreatment. Behavioral
One of the challenges facing clinicians is provision of effec- data were recorded for the interval preceding each NS. “Same
tive BV treatment, as long-term efficacy of recommended anti- pre-/posttreatment RSP” was defined as having the same sexual
biotics is poor and relapse is common [12, 13]. Treatment trials partner pretreatment and in the 2 months after treatment.
have yielded mixed results regarding the contribution of post- Smears were scored by 1 of 3 blinded microbiologists experi-
treatment sexual activity to BV recurrence. In a study of 121 enced in the Nugent method [17]. Women providing ≥2 sets of
women following oral metronidazole treatment, 58% recurred microbiological and behavioral data (follow-up data on ≥1 oc-
within 12 months. Recurrence was associated with having a casions) were included in longitudinal analyses. Specimens not
regular sexual partner (RSP) or a female sexual partner (FSP), returned by interval midpoint, or at 6 months if >210 days after
not using hormonal contraception, and history of BV [12]. enrollment, were considered missing, and participants who did
Sanchez et al found that interim unprotected intercourse was not return specimens were deemed lost to follow-up. Data were
associated with BV recurrence [14], and Schwebke et al reported censored when participants experienced BV recurrence, reached
that abstaining from sex/consistent condom use reduced recur- 210 days, or were lost to follow-up.
rence by 50% [15]. In contrast, in women who have sex with
women (WSW), Marrazzo et al found that recurrence was not Statistical Methods and Ethical Approval
associated with posttreatment sexual activity, but with baseline Frequencies and 95% confidence intervals (CIs) of baseline
and posttreatment detection of specific BVAB [16]. demographic, clinical, and behavioral data were analyzed
Current approaches to the management of BV are clearly using Stata software 12.0 (StataCorp LP). The rate per 100
suboptimal, with reliance on antibiotics that cure less person-years of BV recurrence for selected variables was calcu-
than half the treated population. We sought to determine the lated along with Poisson 95% CIs. Cox regression estimated
behavioral and contraceptive factors associated with BV recur- hazard ratios (HRs) for the risk of BV recurrence associated
rence in an analysis of a double-blind, placebo-controlled with baseline and longitudinal characteristics. Characteristics/
treatment trial, in which combination oral and vaginal thera- exposures that changed during the study period were recon-
pies did not improve recurrence rates over metronidazole structed based on questionnaire data from each study interval
alone [17]. Our hypothesis was that BV recurrence is signifi- and examined in a number of ways including “present” or
cantly influenced by sexual and behavioral practices. “absent” and “current/recent” or “not recent” exposure. Multi-
variate cox regression models were used to assess whether
METHODS these characteristics were predictors of BV as time-dependent
covariates. Models were built sequentially starting with the
This was a double-blind, placebo-controlled, parallel-group characteristic most strongly associated with BV by univariate
trial with balanced randomization (3 arms, 1:1:1) conducted analysis and continued until no other variable reached
778 • CID 2013:56 (15 March) • Bradshaw et al
Table 1. Clinical and Laboratory Results of Study Population Table 2. Demographic and Clinical Characteristics of Study
(N = 404) Population (N = 404) at Baseline
Characteristic No. (%) Characteristic No. (%a)
Pretreatment Nugent score Age, y, median (range) 27 (17–49)
4–6a 64 (15.8) Country of birth
7–10 340 (84.2) Australia/New Zealand 251 (62.3)
Duration of symptomsb Otherb 152 (37.7)
≤21 d 211 (52.2) Educational level
>21 d 194 (47.8) Primary/secondary 140 (35.6)
Rating of abnormal vaginal dischargeb Tertiary/postgraduate 253 (64.4)
None 21 (5.3) History of BV
Mild 75 (19.0) No 205 (51.5)
Moderate/heavy 299 (75.7) Yes 193 (48.5)
Rating of abnormal vaginal odorb Current smoker
None 26 (6.6) No 228 (56.7)
Mild 45 (11.5) Yes 174 (43.3)
Moderate/heavy 322 (81.9) No. of cigarettes smoked per day
Effect of vaginal symptoms on quality of lifeb None 232 (57.4)
Downloaded from http://cid.oxfordjournals.org/ by guest on October 26, 2016
No effect 30 (7.6) <10 84 (20.8)
Somewhat concerned 65 (16.5) ≥10 88 (21.8)
Concerned/very distressed 300 (75.9) Currently douchesc
Effect of vaginal symptoms on sexual satisfactionb No 293 (73.6)
No effect 45 (11.4) Yes 105 (26.4)
Mild 56 (14.2) Douching product (n = 102)
Moderate/major 294 (74.4) Water 50 (49.0)
BV recurrence over 6 mo Water based 23 (22.6)
No BV recurrence (NS 0–6) 289 (71.5) Vinegar/hygiene product/other 29 (28.4)
BV recurrence (NS 7–10) 115 (28.5) Douching frequency
Abbreviation: BV, bacterial vaginosis; NS, Nugent score.
None 293 (74.0)
a
All had 3–4 Amsel criteria. Weekly or less often 57 (14.4)
b
Self-reported pretreatment symptoms and their effects. Daily 46 (85.6)
Current contraceptive method
Condoms only 171 (43.5)
Estrogen/progesterone 110 (28.0)
significance. Univariate and multivariate analyses were strati-
Progesterone only 33 (8.4)
fied for treatment group. As condom use and frequency of sex
No contraception/withdrawal/ 79 (20.1)
were moderately correlated, we built 3 multivariate models: 2 PCI/spermicide
containing one of the correlated variables, the third with both. History of chlamydia
Sensitivity analyses were performed adjusting for treatment No 282 (71.0)
group, and with and without age. A level of P < .05 was con- Yes 115 (29.0)
sidered statistically significant. History of HSV
This trial was approved by the Human Research and Ethics No 342 (86.2)
Committees of the Alfred Hospital and Monash University, Yes 55 (13.8)
History of abnormal Pap result
Melbourne, Australia, with written informed consent obtained
No 290 (73.1)
from participants.
Yes 107 (26.9)
Data are presented as No. (%) unless otherwise specified.
RESULTS Abbreviations: BV, bacterial vaginosis; HSV, herpes simplex virus; PCI,
postcoital intervention.
a
Of the 450 volunteers, 46 provided no postrandomization data Up to 3% of participants may have missing data for some variables;
therefore, proportions are calculated using available data.
and were excluded. Postrandomization NS and behavioral data b
China and Southeast Asia (35%), Britain and Ireland (20%), Eastern and
were available for 404 (90%) women, who contributed 152 Western Europe (17%), and North America (16%).
person-years of follow-up (median, 103 days; no difference c
Douching defined as flushing or washing the vagina out with a solution or water.
Behaviors Associated With BV Recurrence • CID 2013:56 (15 March) • 779
Table 3. Sexual Behavioral Characteristics of Study Population NS = 4–6 and ≥3 Amsel criteria (Table 1). Over the course of
(N = 404) at Baseline 6 months, 115 women (28%) experienced BV recurrence;
there was no difference in recurrence of BV or abnormal flora
Characteristic No. (%a) between treatment arms [17].
No. of male partners last 12 mo
0–1 205 (51.0) Demographic, Behavioral, and Clinical Characteristics of the
≥2 197 (49.0) Study Population
No. of female partners last 12 mo The median age of participants was 27 years (range, 17–49
None 314 (78.9)
years; Table 2). Most women had a tertiary education (64%)
≥1 84 (21.1)
and were born in Australia or New Zealand (62%), with the
Any penile-vaginal sex in the last 12 mo
remainder born in China or Southeast Asia (35%), Britain or
No 38 (9.4)
Yes 366 (90.6)
Ireland (20%), Eastern or Western Europe (17%), and North
Any penile-anal sex in the last 12 mo America (16%). A history of BV was reported by 193 (49%)
No 273 (68.4) women, 174 (43%) were current smokers, and 105 (26%)
Yes 126 (31.6) douched. Condoms were the main contraceptive method for
Any receptive oral sex in the last 12 mo 171 (43%) women, and 110 (28%) used an estrogen-contain-
No 40 (9.9) ing method of contraception (ECC). A history of chlamydia
Yes 363 (90.1) (29%), genital warts (18%), herpes (14%), and abnormal cervi-
Downloaded from http://cid.oxfordjournals.org/ by guest on October 26, 2016
Condom use for any vaginal sex in last 3 mo cal cytology (27%) was common, whereas gonorrhoea was
Alwaysb 66 (16.4) rare (2%).
Not always 336 (83.6)
In the prior 12 months, 197 (49%) women reported having
Condom use for any anal sex in last 3 mo (n = 126)
≥2 male sexual partners (MSPs) and 84 (21%) reported
Always 293 (73.8)
having ≥1 FSP; the majority reported penile-vaginal (91%)
Not always 104 (26.2)
Current sex work
and receptive oral (90%) sex (Table 3). Two hundred seventy-
No 341 (84.8) two women (68%) had an RSP at randomization; of these, 252
Yes 61 (15.2) (93%) were MSPs and 20 (7%) were FSPs. Among women
Practices with RSP with an RSP, 225 (83%) had ongoing vaginal and/or receptive
Current RSP at time of randomization oral sex with the same pretreatment RSP in the 2 months after
No 131 (32.5) treatment; 211 (94%) with MSPs and 14 (6%) with FSPs. Few
Yes 272 (67.5) (16%) participants reported consistent condom use for penile-
Sex of RSP at baseline vaginal sex in the 3 months prior to enrollment. Sixty-one
Male 252 (92.7) participants (15%) were sex workers.
Female 20 (7.3)
Practices with FSP
Demographic and Behavioral Factors Associated With BV
Any receptive oral sex from an FSP in last 12 mo
Recurrence
No 335 (83.8)
Yes 65 (16.2)
Univariate analysis of baseline and longitudinal characteristics
Any unwashed shared toy use with an FSP last 3 mo (n = 82) associated with BV recurrence, stratified by treatment group,
No 65 (79.3) are described in Table 4. Baseline characteristics associated
Yes 17 (20.7) with recurrence included being born outside Australia/New
Zealand (HR = 1.48; 95% CI, 1.02–2.15), having a baseline
Abbreviations: FSP, female sexual partner; RSP, regular sexual partner.
a
Up to 2% of participants may have missing data for some variables; RSP (HR = 1.72; 95% CI, 1.12–2.64), and ECC use (HR = 0.57;
therefore, proportions are calculated using available data. 95% CI, .37–.87). Age, education, treatment, and history of
b
Or no vaginal sex in last 3 months. BV were not associated with recurrence. No other baseline be-
haviors were associated with recurrence, including number of
MSPs or FSPs; vaginal, anal, or receptive oral sex in the last 12
months; or inconsistent condom use for vaginal or anal sex in
between treatment groups, P = .90). Fifty-seven participants the last 3 months.
(13%) without BV recurrence did not complete 6 months of Longitudinal univariate posttreatment practices and behav-
follow-up, but contributed person-time to survival analyses as iors associated with BVrecurrence (Table 4) included having
non recurrent cases based on their last NS. At baseline, the penile-vaginal sex (HR = 1.88; 95% CI, 1.15–3.07), inconsistent
majority of women had an NS = 7–10 (84%); 64 (16%) had an condom use for penile-vaginal sex (HR = 1.96; 95% CI, 1.29–
780 • CID 2013:56 (15 March) • Bradshaw et al
Table 4. Baseline Demographics and Baseline and Longitudinal Behavioral Factors Associated With Recurrence, Stratified for Treat-
ment Group
BV Recurrence Rate per
Characteristic (N = 404) 100 py (95% CI) Unadjusted HR (95% CI) P Value
Demographics, treatment allocation, and conditions
Age, y
17–27 76 (59–98) 1
>27 75 (58–98) 0.99 (.39–1.42) .935
Country of birth
Australia/New Zealand 63 (49–81) 1
Other 97 (74–127) 1.48 (1.02–2.15) .038
Educational level
Primary/secondary 94 (71–124) 1
Tertiary 66 (51–84) 0.71 (.49–1.03) .069
Vaginal treatment group
Placebo 74 (54–103) 1
Probiotic 75 (54–103) 0.99 (.63–1.58) .978
Clindamycin 78 (58–106) 1.06 (.68–1.65) .791
Downloaded from http://cid.oxfordjournals.org/ by guest on October 26, 2016
History of BV
No 72 (55–93) 1
Yes 79 (61–103) 1.12 (.78–1.62) .539
Use of ECC at enrollment
No 89 (72–110) 1
Yes 52 (32–76) 0.57 (.37–.87) .010
Baseline sexual behavior
No. of male partners last 12 mo
0–2 82 (64–106) 1
≥3 70 (54–92) 0.84 (.58–1.20) .340
No. of female partners last 12 mo
0 73 (59–90) 1
≥1 84 (58–123) 1.16 (.76–1.77) .482
Any penile-vaginal sex in the last 12 mo
No 62 (32–120) 1
Yes 77 (64–93) 1.24 (.64–2.45) .517
Any penile-anal sex in the last 12 mo
No 75 (60–94) 1
Yes 77 (56–107) 1.02 (.69–1.51) .918
Any receptive oral sex in the last 12 mo
No 90 (52–155) 1
Yes 74 (61–90) 0.82 (.46–1.47) .510
Condom use for any vaginal sex in last 3 mo
Always (or not that 78 (64–95) 1
practice)
Not always 63 (39–103) 0.79 (.48–1.32) .370
Condom use for any anal sex in last 3 mo
Always (or not that 79 (55–112) 1
practice)
Not always 75 (61–93) 0.96 (.64–1.43) .828
RSP at enrollment
No 52 (36–76) 1
Yes 88 (72–109) 1.72 (1.12–2.64) .014
Behaviors Associated With BV Recurrence • CID 2013:56 (15 March) • 781
Table 4 continued.
BV Recurrence Rate per
Characteristic (N = 404) 100 py (95% CI) Unadjusted HR (95% CI) P Value
a
Longitudinal behaviors
Smoker
Never 69 (54–90) 1
Ever during observation 83 (64–108) 1.18 (.82–1.69) .378
No. of cigarettes smoked per day
None 70 (55–89) 1
1–9 86 (58–128) 1.24 (.79–1.95) .340
≥10 84 (56–126) 1.13 (.73–1.76) .587
Currently douching
No 70 (56–87) 1
Yes 94 (66–135) 1.28 (.84–1.96) .246
Current/recent use of ECC
No 87 (70–107) 1
Yes 55 (38–80) 0.62 (.40–.95) .028
Current sex work
Downloaded from http://cid.oxfordjournals.org/ by guest on October 26, 2016
No 74 (60–90) 1
Yes 91 (56–148) 1.17 (.69–1.99) .565
Any penile-vaginal sex
No 46 (29–72) 1
Yes 85 (70–105) 1.88 (1.15–3.07) .012
Any penile-anal sex
No 74 (60–90) 1
Yes 83 (49–140) 1.09 (.63–1.89) .754
Any receptive oral sexb
No 76 (57–100) 1
Yes 72 (56–92) 0.93 (.64–1.36) .707
Condom use for any penile-vaginal sex
Alwaysc 47 (33–68) 1
Not always 93 (75–115) 1.96 (1.29–2.99) .002
Any new male partner
None 73 (59–90) 1
≥1 84 (57–124) 1.16 (.76–1.77) .491
Any female partner
None 74 (61–90) 1
≥1 118 (59–236) 1.59 (.77–3.29) .213
Same pre-/posttreatment RSPd
No 53 (38–73) 1
Yes 95 (76–118) 1.84 (1.25–2.73) .002
Frequency of sex with any sexual partnerse
No sex 41 (24–69) 1
1–4 times per mo 87 (65–116) 2.18 (1.19–4.01) .012
≥5 times per mo 82 (62–107) 1.96 (1.09–3.52) .025
Unadjusted hazard ratios are stratified by treatment group, bolded text indicates significant associations at the level p < 0.05.
Abbreviations: BV, bacterial vaginosis; CI, confidence interval; ECC, estrogen-containing contraceptive; HR, hazard ratio; py, person-years; RSP, regular sexual
partner.
a
Each variable is comprised of behaviors reported longitudinally by participants at each study interval.
b
Receptive oral sex is defined as being given oral sex.
c
Or no penile-vaginal sex.
d
Same pre-/posttreatment RSP, defined as same sexual partner pretreatment and in the 2 months posttreatment.
e
Sex with females is having received oral sex, sex with males is penile-vaginal sex.
782 • CID 2013:56 (15 March) • Bradshaw et al
Table 5. Demographic and Behavioral Factors Associated With Recurrence of Bacterial Vaginosis, Multivariate Model
BV Model 1a Model 2a Model 3a
Recurrence
Rate per
Characteristic 100 py Unadjusted HR P Adjusted HR P Adjusted HR P Adjusted HR P
(N = 404) (95% CI) (95% CI) Value (95% CI) Value (95% CI) Value (95% CI) Value
Age, y
17–27 76 (59–98) 1 1 1 1
>27 75 (58–98) 0.98 (.68–1.41) .902 0.98 (.68–1.43) .931 0.97 (.66–1.41) .863 0.95 (.66–1.39) .812
Country of birth
Australia/New Zealand 63 (49–81) 1 1 1 1
Other 97 (74–127) 1.54 (1.06–2.22) .022 1.49 (1.03–2.17) .034 1.47 (1.01–2.14) .042 1.46 (1.01–2.13) .045
Current/recent use of ECC
No 87 (70–107) 1 1 1 1
Yes 55 (38–80) 0.63 (.41–.96) .031 0.51 (.33–.78) .002 0.56 (.36–.87) .010 0.52 (.34–.81) .004
Same pre-/posttreatment RSPb
No 53 (38–73) 1 1 1 1
Yes 95 (76–118) 1.84 (1.25–2.73) .002 1.77 (1.14–2.73) .010 1.99 (1.25–3.18) .004 1.91 (1.19–3.07) .007
Condom use for any penile-vaginal sex
Downloaded from http://cid.oxfordjournals.org/ by guest on October 26, 2016
Alwaysc 47 (33–68) 1 1 1
Not always 93 (75–115) 1.96 (1.28–3.00) .002 1.74 (1.12–2.70) .014 1.85 (1.04–3.29) .037
Frequency of sex with any sexual partnersd
No sex 41 (24–69) 1 1 1
1–4 times per mo 87 (65–116) 2.17 (1.18–3.99) .013 1.74 (.92–3.29) .090 1.09 (.49–2.40) .826
≥5 times per mo 82 (62–107) 1.97 (1.09–3.56) .025 1.41 (.74–2.69) .300 0.85 (.36–1.97) .700
Bolded text indicates significant associations at the level p < 0.05.
Abbreviations: BV, bacterial vaginosis; CI, confidence interval; ECC, estrogen-containing contraceptive; HR, hazard ratio; py, person-years; RSP, regular sexual
partner.
a
All models are stratified for treatment.
b
Same pre-/posttreatment RSP defined as same sexual partner pretreatment and in the 2 months posttreatment.
c
Or no penile-vaginal sex.
d
Sex with females is defined as having received oral sex, sex with males is defined as penile-vaginal sex.
2.99), and having the same pre-/posttreatment RSP (male or recurrence (HR = 2.18; 95% CI, 1.19–4.01 and HR = 1.96; 95%
female) (HR = 1.84; 95% CI, 1.25–2.73). Current or recent use CI, 1.09–3.52, respectively); however, there was no dose re-
of an ECC (oral contraceptive pill = 108, NuvaRing = 2) was sponse between increased frequency of sexual activity and risk
protective against BV recurrence (HR = 0.62; 95% CI, .40–.95). of recurrence. Frequency of penile-vaginal sex and/or any
Of the 110 women using an ECC at baseline, 80 (72%) had sexual activity with MSPs and FSPs were examined as contin-
continuous ECC use, and 30 (28%) inconsistent ECC use uous variables and at a number of cut points: there was no
during follow-up. Because ovulation can be delayed for several significant association with increased sexual activity and in-
months after ceasing ECC, ECC use was analyzed longitudi- creased risk of recurrence using these methods (data not
nally as “current/recent” or “not recent.” Few women (n = 33) shown). No association was found between BV recurrence and
used progesterone-only methods of contraception, which a new sexual partner, FSPs, smoking, douching, or engaging
limited our power to examine their association with recur- in sex work.
rence; however, use of any hormonal contraception was not Factors associated with BV recurrence by univariate analysis
significantly protective against recurrence (HR = 0.83; 95% CI, were included in multivariate analyses and stratified for treat-
.56–1.24). ment group. This included country of birth, ECC use, same
We explored the association between BV recurrence and pre-/posttreatment RSP, and condom use for penile-vaginal
frequency of sexual activity with partners (male and female) sex (Table 5). Age was included owing to reported associations
and then with frequency of penile-vaginal sex alone. Com- with BV and sexual/contraceptive practices. Frequency of
pared with no sexual activity, sexual contact with partners ≤4 sexual activity was included to determine whether it exerted
times per month or >4 times per month was associated with an independent effect on recurrence after adjusting for RSP.
Behaviors Associated With BV Recurrence • CID 2013:56 (15 March) • 783
As frequency of sex and condom use were moderately correlat- activity does not explain this association. Increased frequency of
ed (r = 0.66, P < .001), 3 multivariate analyses were conducted; sexual activity has been proposed as a mechanism by which
2 contained one of the correlated variables, and one included normal vaginal flora is disrupted. Studies have found an associ-
both variables. Multivariate models were stratified for treat- ation between frequency of penile-vaginal, digital-vaginal, toy-
ment group, but sensitivity analyses were also performed ad- vaginal, or receptive oral sex, and unfavorable vaginal states
justing for treatment group, and with and without age, including unstable vaginal flora [18], BV [19], reduction in
yielding similar results (data not shown). hydrogen peroxide–producing lactobacilli [11, 20, 21], and in-
Model 1 includes the variables most strongly associated creased colonization with G. vaginalis [11]; however, others
with BV recurrence, and demonstrates that having the same report that higher frequency of penile-vaginal sex increases con-
pre-/posttreatment RSP (adjusted HR [AHR] = 1.77; 95% CI, centrations of protective hydrogen peroxide–producing lactoba-
1.14–2.73) and inconsistent condom use for penile-vaginal sex cilli [11].
with any MSP (AHR = 1.74; 95% CI, 1.12–2.70) were associat- Inconsistent condom use for penile-vaginal sex was strongly
ed with BV recurrence, whereas ECC use was protective associated with BV recurrence, and remained so after control-
(AHR = 0.51; 95% CI, .33–.78). Being born outside Australia/ ling for an RSP and other behaviors. This finding is consistent
New Zealand showed a modest association with recurrence with previous studies [14, 15], and a meta-analysis showing a
(AHR = 1.49; 95% CI, 1.03–2.17). The second model included 20% protective effect of consistent condom use against BV [7].
frequency of sex and omitted the correlated “condom use” Other data support the concept that exposure to male genitalia
variable. This analysis showed that frequency of sexual activity contributes to the development of BV in heterosexual women.
Downloaded from http://cid.oxfordjournals.org/ by guest on October 26, 2016
was not associated with recurrence, exposure to the same pre-/ Wives of circumcised males in a Ugandan circumcision trial
posttreatment RSP conferred an increased risk (AHR = 1.99; had a significantly reduced risk of BV (adjusted prevalence
95% CI, 1.25–3.18), and ECC use halved the risk (AHR = 0.56; risk ratio = 0.60; 95% CI, .38–.94) compared to wives of uncir-
95% CI, .36–.87) of recurrence. The final model included all cumcised males [22]. Furthermore, male circumcision has
variables and confirmed that after adjusting for frequency of been associated with a significant reduction in penile anaero-
sexual activity, having the same pre-/posttreatment RSP bic microbial flora, including BV-associated genera Clostri-
(AHR = 1.91; 95% CI, 1.19–3.07), inconsistent condom use for diales and Prevotellaceae [9]. Pyrosequencing of the
penile-vaginal sex (AHR = 1.85; 95% CI, 1.04–3.29) and being microbiota of the coronal sulcus and distal urethra in adoles-
born outside Australia/New Zealand (AHR = 1.46; 95% CI, cents [23] showed these sites to be colonized by BVAB, with
1.01–2.13) were associated with BV recurrence, whereas ECC the composition of the coronal sulcus microbiota influenced
use was protective (AHR = 0.52; 95% CI, .34–.81). by circumcision and sexual activity [23]. Male carriage of
G. vaginalis, an organism considered to be integral in the
DISCUSSION development of BV, is commonly reported [10, 24, 25].
This trial was conducted in a population of sexually
In this trial, posttreatment sexual and contraceptive behaviors active women who predominantly had sex with men.
were strongly associated with BV recurrence. Importantly, ex- Numbers of posttreatment FSPs were too small to examine
posure to the same pre-/posttreatment RSP, and inconsistent the contribution of female partnerships to recurrence. Im-
condom use for penile-vaginal sex, nearly doubled the risk of portantly, there is increasing evidence to support exchange
BV recurrence, whereas the use of an estrogen-containing con- of vaginal flora and BVAB between WSW. WSW have been
traceptive method halved the risk. These data provide compel- shown to have high levels of concordant vaginal flora with
ling evidence that behavioral and contraceptive practices play their FSP [26, 27], and Lactobacillus species are shared
a significant role in modifying the effectiveness of current an- between FSPs [28]. We previously reported that women
tibiotics in the treatment of BV. with a posttreatment FSP had a 3-fold increased risk of BV
The association between exposure to an ongoing RSP and recurrence [12]. Although Marrazzo et al found that BV re-
recurrence is supported by a previous study in which women currence was not associated with posttreatment sexual
who remained with their pretreatment RSP had a 3-fold in- activity in WSW [16], this group recently reported that
creased risk of BV recurrence [12]. The robustness of the asso- vaginal-toy use was associated with higher likelihood of col-
ciation between recurrence and exposure to an RSP across 3 onization with G. vaginalis [11] and digital-vaginal and
multivariate models, and the fact that it remained after adjust- oral-vaginal sex with reduced load of L. crispatus [21]. They
ing for frequency of sexual activity, condom use, and other po- hypothesized that some protective commensal species could
tentially confounding behavioral factors, indicates that ongoing be particularly sensitive to the effects of sexual activity.
exposure to an RSP significantly contributes to BV recurrence Estrogen-containing contraception, predominantly the oral
in this cohort, and importantly, that more frequent sexual contraceptive pill in this cohort, showed a significantly
784 • CID 2013:56 (15 March) • Bradshaw et al
protective effect against BV recurrence after adjusting for con- posttreatment sexual and contraceptive behaviors. Whether
founding factors including condom use and RSP. A number of the association with RSP is due to reinfection/transmission of
cross-sectional studies have reported hormonal contraceptives, BVAB from untreated RSPs, another “RSP factor” that hinders
mainly combined, to be protective against prevalent [29–31], recolonization after treatment with protective Lactobacillus
incident [32, 33], and recurrent [12, 31] BV, with a some species, or unmeasured confounding remains unanswered. Al-
studies also reporting that progesterone-only methods may though 5 of 6 partner treatment trials failed to reduce BV re-
be associated with a reduced risk for incident [33] and currence in women, systematic review has shown that these
recurrent [31] BV. One mechanism by which combined con- trials were significantly flawed [40]. These data raise the tanta-
traceptives may be protective is that estrogen increases the gly- lizing question of whether partner treatment trials in hetero-
cogen-content of epithelial cells, which is a substrate for sexual and WSW populations need revisiting. Importantly for
Lactobacillus species for the generation of lactic acid, a known clinicians, it appears that potentially modifiable practices, such
potent inhibitor of BV [34, 35]. Hormonal contraceptives, par- as use of condoms and/or estrogen-containing contraceptives,
ticularly progesterone-only, may also reduce heme availability may provide a degree of protection against recurrence. As
for anaerobes such as G. vaginalis through reduction in men- current therapeutic approaches have limited impact on long-
struation. Interestingly, BV is most commonly reported at the term BV cure, we need to understand the mechanisms by
beginning of the menstrual cycle when estradiol levels are which these practices modify the risk of BV recurrence, and to
lowest [36, 37], and higher rates of remission occur in preg- more formally assess such interventions to determine the
nancy [38]. Contraceptive use may also affect immunological degree to which they impact on BV recurrence. In the era of
Downloaded from http://cid.oxfordjournals.org/ by guest on October 26, 2016
factors, with Cherpes et al reporting that hormonal contraceptive combination prevention approaches for HIV infection, it
use was associated with altered vaginal immunity in BV [39]. seems quite possible that treatment of BV could be improved
This study has a number of limitations. Sexual practices are through integration of modifiable behavioral factors within
often highly correlated, making it difficult to attribute an asso- more holistic management approaches.
ciation to a specific behavior and to infer causality. Even
though the association between exposure to the same RSP and
Notes
BV recurrence remained in all 3 models after adjusting for po-
tentially confounding factors, we cannot exclude the effect of Acknowledgments. We acknowledge and thank Surbhi Bird, Andrea
Morrow, Sandy Walker, and Eve Urban (Melbourne Sexual Health Centre)
unmeasured confounding. Secondly, we did not have sufficient for their assistance with the daily running of the clinical trial; Glenda
power to examine the effect of less common behaviors on re- Fehler and Leonie Horvath (Melbourne Sexual Health Centre) for assisting
currence, such as female partners and progesterone-only con- with microscopy for the trial; and Philipp Grob and Valda Prasauskas
from Medinova for providing the probiotic and placebo that were evaluat-
traceptives. Although sufficiently common to be assessed,
ed in the original trial.
there was no association between BV recurrence and risk Financial support. This work was supported by the Australian Na-
factors previously associated with BV including history of BV, tional Health and Medical Research Council Project (grant number
smoking, douching, and sex work. Self-sampling was em- APP454644); by the Australian National Health and Medical Research
Council (fellowship numbers APP 456164 and 566576 to C. S. B. and
ployed to optimize participant retention, we were therefore J. S. H., respectively); and by a Primary Health Care Research Evaluation
limited in our outcome measure to the use of the Nugent and Development Mid-career Fellowship, Department of Health and
method, which potentially underestimated BV recurrence by Aging (to M. P.).
Potential conflicts of interest. All authors: No reported conflicts.
classifying women with an NS of 4–6 but ≥3 Amsel criteria as All authors have submitted the ICMJE Form for Disclosure of Potential
cured. The strengths of our trial include that it was a large Conflicts of Interest. Conflicts that the editors consider relevant to the
RCT with high retention rates and detailed epidemiologic data content of the manuscript have been disclosed.
matched to frequent sampling over 6 months. This minimized
participant recall bias and enabled accurate assessment of as- References
sociations between recent behaviors and relevant NSs and
1. Allsworth JE, Peipert JF. Prevalence of bacterial vaginosis: 2001–2004
longer-term BV recurrence. We applied the gold-standard National Health and Nutrition Examination Survey Data. Obstet
Nugent method to ensure generalizability of our findings, and Gynecol 2007; 109:114–20.
have an ongoing quality-assurance program to ensure consis- 2. Walker J, Hocking JS, Fairley CK, et al. The prevalence and incidence
of bacterial vaginosis in a cohort of young Australian women. In:
tency between our experienced microbiologists.
Conference proceedings of the International Society for Sexually
A striking aspect to clinical management of BV is that 1- Transmitted Diseases Research. Quebec, Canada, 2011.
month cure rates of recommended therapies are 70%–80%; 3. Fredricks DN, Fiedler TL, Marrazzo JM. Molecular identification of
however, by 3–12 months, failure rates approach 50% [12, 13]. bacteria associated with bacterial vaginosis. N Engl J Med 2005;
353:1899–911.
Our data indicate that the long-term poor performance of rec- 4. Swidsinski A, Mendling W, Loening-Baucke V, et al. Adherent bio-
ommended therapies may at least partly be attributed to films in bacterial vaginosis. Obstet Gynecol 2005; 106:1013–23.
Behaviors Associated With BV Recurrence • CID 2013:56 (15 March) • 785
5. Swidsinski A, Mendling W, Loening-Baucke V, et al. An adherent 22. Gray RH, Kigozi G, Serwadda D, et al. The effects of male circumci-
Gardnerella vaginalis biofilm persists on the vaginal epithelium after sion on female partner's genital tract symptoms and vaginal infections
standard therapy with oral metronidazole. Am J Obstet Gynecol 2008; in a randomized trial in Rakai, Uganda. Am J Obstet Gynecol 2009;
198:97 e91–96. 200:42.e1–7.
6. Fethers KA, Fairley CK, Morton A, et al. Early sexual experiences and 23. Nelson DE, Dong Q, Van Der Pol B, et al. Bacterial communities of
risk factors for bacterial vaginosis. J Infect Dis 2009; 200:1662–70. the coronal sulcus and distal urethra of adolescent males. PLoS One
7. Fethers KA, Fairley CK, Hocking JS, Gurrin LC, Bradshaw CS. Sexual 2012; 7:e36298.
risk factors and bacterial vaginosis: a systematic review and meta-anal- 24. Bradshaw CS, Tabrizi SN, Read TRH, et al. Etiologies of non-gonococ-
ysis. Clin Infect Dis 2008; 47:1426–35. cal urethritis: bacteria, viruses and the association with oro-genital
8. Nelson DE, Van Der Pol B, Dong Q, et al. Characteristic male urine exposure. J Infect Dis 2006; 193:336–45.
microbiomes associate with asymptomatic sexually transmitted infec- 25. Piot P. Distribution of eight serotypes of Ureaplasma urealyticum in
tion. PLoS One 2012; 5:e14116. cases of non-gonococcal urethritis and of gonorrhoea, and in healthy
9. Price LB, Liu CM, Johnson KE, et al. The effects of circumcision on persons. Br J Vener Dis 1976; 52:266–8.
the penis microbiome. PLoS One 2010; 5:e8422. 26. Marrazzo JM, Koutsky LA, Eschenbach DA, et al. Characterization of
10. Schwebke JR, Rivers C, Lee J. Prevalence of Gardnerella vaginalis in vaginal flora and bacterial vaginosis in women who have sex with
male sexual partners of women with and without bacterial vaginosis. women. J Infect Dis 2002; 185:1307–13.
Sex Transm Dis 2009; 36:92–4. 27. Bailey JV, Farquhar C, Owen C. Bacterial vaginosis in lesbians and
11. Mitchell C, Manhart LE, Thomas KK, Agnew K, Marrazzo JM. Effect bisexual women. Sex Transm Dis 2004; 31:691–4.
of sexual activity on vaginal colonization with hydrogen peroxide- 28. Marrazzo JM, Antonio M, Agnew K, Hillier SL. Distribution of genital
producing lactobacilli and Gardnerella vaginalis. Sex Transm Dis Lactobacillus strains shared by female sex partners. J Infect Dis 2009;
2011; 38:1137–44. 199:680–3.
12. Bradshaw CS, Morton AN, Hocking J, et al. High recurrence rates of 29. Shoubnikova M, Hellberg D, Nilsson S, Mardh PA. Contraceptive
bacterial vaginosis over the course of 12 months after oral metronida- use in women with bacterial vaginosis. Contraception 1997; 55:355–8.
Downloaded from http://cid.oxfordjournals.org/ by guest on October 26, 2016
zole therapy and factors associated with recurrence. J Infect Dis 2006; 30. Calzolari E, Masciangelo R, Milite V, Verteramo R. Bacterial
193:1478–89. vaginosis and contraceptive methods. Int J Gynaecol Obstet 2000;
13. Sobel JD, Schmitt C, Meriwether C. Long-term follow-up of patients 70:341–6.
with bacterial vaginosis treated with oral metronidazole and topical 31. Riggs M, Klebanoff M, Nansel T, et al. Longitudinal association
clindamycin. J Infect Dis 1993; 167:783–4. between hormonal contraceptives and bacterial vaginosis in women of
14. Sanchez S, Garcia PJ, Thomas KK, Catlin M, Holmes KK. Intravaginal reproductive age. Sex Transm Dis 2007; 34:954–9.
metronidazole gel versus metronidazole plus nystatin ovules for bacte- 32. Avonts D, Sercu M, Heyerick P, et al. Incidence of uncomplicated
rial vaginosis: a randomized controlled trial. Am J Obstet Gynecol genital infections in women using oral contraception or an intrauter-
2004; 191:1898–906. ine device: a prospective study. Sex Transm Dis 1990; 17:23–9.
15. Schwebke JR, Desmond RA. A randomized trial of the duration of 33. Baeten JM, Nyange PM, Richardson BA, et al. Hormonal contracep-
therapy with metronidazole plus or minus azithromycin for treat- tion and risk of sexually transmitted disease acquisition: results from a
ment of symptomatic bacterial vaginosis. Clin Infect Dis 2007; prospective study. Am J Obstet Gynecol 2001; 185:380–5.
44:213–9. 34. O’Hanlon DE, Lanier BR, Moench TR, Cone RA. Cervicovaginal fluid
16. Marrazzo JM, Thomas KK, Fiedler TL, Ringwood K, Fredricks DN. and semen block the microbicidal activity of hydrogen peroxide pro-
Relationship of specific vaginal bacteria and bacterial vaginosis treat- duced by vaginal lactobacilli. BMC Infect Dis 2010; 10:120.
ment failure in women who have sex with women. Ann Intern Med 35. O’Hanlon DE, Moench TR, Cone RA. In vaginal fluid, bacteria associ-
2008; 149:20–8. ated with bacterial vaginosis can be suppressed with lactic acid but
17. Bradshaw CS, Pirotta M, De Guingand D, et al. Efficacy of oral metro- not hydrogen peroxide. BMC Infect Dis 2011; 11:200.
nidazole with vaginal clindamycin or vaginal probiotic for bacterial 36. Bradshaw CS, Morton AN, Garland SM, et al. Higher-risk behavioral
vaginosis: randomised placebo-controlled double-blind trial. PLoS practices associated with bacterial vaginosis compared with vaginal
One 2012; 7:e34540. candidiasis. Obstet Gynecol 2005; 106:105–14.
18. Schwebke JR, Richey CM, Weiss HL. Correlation of behaviors with mic- 37. Schwebke JR, Morgan SC, Weiss HL. The use of sequential self-
robiological changes in vaginal flora. J Infect Dis 1999; 180:1632–6. obtained vaginal smears for detecting changes in the vaginal flora. Sex
19. Marrazzo JM, Thomas KK, Fiedler TL, Ringwood K, Fredricks DN. Transm Dis 1997; 24:236–9.
Risks for acquisition of bacterial vaginosis among women who report 38. Hay PE, Morgan DJ, Ison CA, et al. A longitudinal study of
sex with women: a cohort study. PLoS One 2010; 5:e11139. bacterial vaginosis during pregnancy. Br J Obstet Gynaecol 1994;
20. Vallor AC, Antonio MA, Hawes SE, Hillier SL. Factors associated with 101:1048–53.
acquisition of, or persistent colonization by, vaginal lactobacilli: role of 39. Cherpes TL, Marrazzo JM, Cosentino LA, et al. Hormonal contracep-
hydrogen peroxide production. J Infect Dis 2001; 184:1431–6. tive use modulates the local inflammatory response to bacterial vagi-
21. Mitchell C, Manhart LE, Thomas K, et al. Behavioral predictors of nosis. Sex Transm Infect 2008; 84:57–61.
colonization with Lactobacillus crispatus or Lactobacillus jensenii after 40. Mehta SD. Systematic review of randomized trials of treatment of
treatment for bacterial vaginosis: a cohort study. Infect Dis Obstet male sexual partners for improved bacterial vaginosis outcomes in
Gynecol 2012; 2012:706540. women. Sex Transm Dis 2012; 39:822–30.
786 • CID 2013:56 (15 March) • Bradshaw et al
View publication stats
You might also like
- Bipolar 2 FixDocument10 pagesBipolar 2 FixtunihaaNo ratings yet
- W9 WJ 20 InsDocument19 pagesW9 WJ 20 InsDaffaliska Azaria NugrahaNo ratings yet
- W9 WJ 20 InsDocument19 pagesW9 WJ 20 InsDaffaliska Azaria NugrahaNo ratings yet
- PDF Forensik PDFDocument6 pagesPDF Forensik PDFWira AdityaNo ratings yet
- 8140 Ce (Ra) F (T) PF1 (Agak) Pfa (Ak) PF2 (Pag) PF2 (PN) PDFDocument4 pages8140 Ce (Ra) F (T) PF1 (Agak) Pfa (Ak) PF2 (Pag) PF2 (PN) PDFKoas PatoNo ratings yet
- PDF Forensik PDFDocument6 pagesPDF Forensik PDFWira AdityaNo ratings yet
- Herpes Zoster and Postherpetic Neuralgia - Prevention and ManagementDocument8 pagesHerpes Zoster and Postherpetic Neuralgia - Prevention and ManagementNadia Desanti RachmatikaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- BLEEDING DISORDERS GUIDEDocument26 pagesBLEEDING DISORDERS GUIDEsaskiakonitaNo ratings yet
- Statement of Account For TuberculosisDocument1 pageStatement of Account For TuberculosisMHIEMHOINo ratings yet
- Actress Selma Blair, Factitious Disorder, October 2019.Document22 pagesActress Selma Blair, Factitious Disorder, October 2019.4456280% (10)
- Immunology and Serology Lecture HistoryDocument3 pagesImmunology and Serology Lecture HistoryLyka ReyesNo ratings yet
- High Risk New BornDocument36 pagesHigh Risk New BornIze C VijiNo ratings yet
- CHANGES After Death (Part Two) 2011 GC - 2Document18 pagesCHANGES After Death (Part Two) 2011 GC - 2HassanNo ratings yet
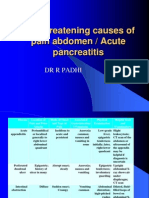
- Life Threatening Causes of Pain Abdomen / Acute PancreatitisDocument27 pagesLife Threatening Causes of Pain Abdomen / Acute PancreatitisDr. Rajesh Padhi100% (1)
- The Effect of Exercise On Cardiovascular Activity in HumansDocument11 pagesThe Effect of Exercise On Cardiovascular Activity in HumansnbwassamNo ratings yet
- Gastrointestinal Stromal Tumor Early Detection, Diagnosis, and StagingDocument22 pagesGastrointestinal Stromal Tumor Early Detection, Diagnosis, and StagingDekdesNo ratings yet
- Ectopia LentisDocument38 pagesEctopia LentisSaransh Sharma100% (1)
- Mls Study Guidelines AscpDocument5 pagesMls Study Guidelines AscpCielamae Orbeta100% (1)
- NP1Document43 pagesNP1Edward Nicko GarciaNo ratings yet
- Nursing Care of a Child with Acute Myeloid LeukemiaDocument18 pagesNursing Care of a Child with Acute Myeloid LeukemiaStephanie Joy EscalaNo ratings yet
- Tri Immunophasic Periodontal TherapyDocument9 pagesTri Immunophasic Periodontal TherapySireesha SadasivanNo ratings yet
- Oral Ulcers: Acute and ChronicDocument39 pagesOral Ulcers: Acute and Chronicnour almarshadiNo ratings yet
- Homeopathic Relief for DepersonalizationDocument4 pagesHomeopathic Relief for DepersonalizationAnonymous dpxYTENo ratings yet
- Makalah Basic Life SupportDocument22 pagesMakalah Basic Life SupportKustian PramuditaNo ratings yet
- Internship Manual 20-21 PDFDocument19 pagesInternship Manual 20-21 PDFMsalik1No ratings yet
- IHW 2024 - Sponsorship LetterDocument2 pagesIHW 2024 - Sponsorship LettercharliekonsorNo ratings yet
- Wound HealingDocument23 pagesWound Healingkhadija HabibNo ratings yet
- Allergies Yes: No: Royal Government of Bhutan Jigme Dorji Wangchuk National Referral Hospital Patient Discharge FormDocument2 pagesAllergies Yes: No: Royal Government of Bhutan Jigme Dorji Wangchuk National Referral Hospital Patient Discharge FormSuman Pradhan 2803No ratings yet
- 10.1007-S00210-008-027serotonin Pharmacology in The Gastrointestinal Tract: A ReviewDocument23 pages10.1007-S00210-008-027serotonin Pharmacology in The Gastrointestinal Tract: A ReviewanataeusNo ratings yet
- COPD A Multifactorial Systemic DiseaseDocument9 pagesCOPD A Multifactorial Systemic DiseaseNjala SankhulaniNo ratings yet
- Pediatric DentistryDocument8 pagesPediatric DentistryPavleta RashkovaNo ratings yet
- Tips For The NDECCDocument2 pagesTips For The NDECCMagda Jakubowska-EwiczNo ratings yet
- PD2Document15 pagesPD2DrShobhit RajNo ratings yet
- Nursing Responsibilities Adverse Effect Indication / Contraindication Mechanism of Action Drug Name IndicationDocument1 pageNursing Responsibilities Adverse Effect Indication / Contraindication Mechanism of Action Drug Name IndicationOmar IzzoNo ratings yet
- Nursing Care For Patient With Wilms TumorDocument2 pagesNursing Care For Patient With Wilms TumorAnusha Verghese100% (2)
- Lyphochek Immunology Plus Control Levels 1 and 2: 430 430X Bilevel Minipak 12 X 1 ML 2 X 1 ML Level 1 27551 Level 2 27552Document6 pagesLyphochek Immunology Plus Control Levels 1 and 2: 430 430X Bilevel Minipak 12 X 1 ML 2 X 1 ML Level 1 27551 Level 2 27552Ade FeriyatnaNo ratings yet
- Pemeriksaan Klinis Pada Bayi Dan Anak (Edisi 3) Bab 1-4Document72 pagesPemeriksaan Klinis Pada Bayi Dan Anak (Edisi 3) Bab 1-4Nadia Hani Nabilah Irawan100% (1)