Professional Documents
Culture Documents
Hemorrhage NCP
Uploaded by
Elisha0 ratings0% found this document useful (0 votes)
1K views4 pagesNursing care plan for hemorrhage
Original Title
hemorrhage Ncp
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentNursing care plan for hemorrhage
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
1K views4 pagesHemorrhage NCP
Uploaded by
ElishaNursing care plan for hemorrhage
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
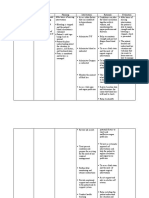
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
Subjective: Fluid Volume At the end of Independent Client’s pulse
easy fatigability, Deficit secondary nursing Assess uterine That is to note rate is between
anxiety to Postpartum intervention, client contraction and how much 80 to 100 beats
Hemorrhage will maintain fluid lochia flow blood loss the per min and
Objective: volume at a every 2 hours. client is blood pressure
Drop in the functional level as experiencing is 110/60
haemoglobin evidenced by and to prompt mmHg, lochia
and hematocrit individually for immediate slows to
laboratory adequate Assess vital intervention moderate
results haemoglobin, signs and note Changes in BP amount of flow
Blood loss more hematocrit for peripheral and pulse may with no large
than 500 ml laboratory results, pulses. be used for clots,
Heavy lochia stable vital signs, rough estimate hemoglobin
flow adequate urine of blood loss. level is above
Decreased output, good skin 11g/L.
urine output turgor and capillary Collaborative Client
Pallor refill after one Monitor Helps in verbalizes
week. laboratory monitoring the understanding
studies effectiveness of of the causative
(haemoglobin the intervention; factors and
and hematocrit, malfunction in purpose of
creatinine/ BUN) the kidneys may interventions
indicate major and medication;
bleeding participates in
episodes procedures
Advise client to Activity may without
maintain bed predispose to hesitations;
rest and further bleeding. attentive and
schedule monitors own
activities to vital signs upon
provide assessment;
undisturbed rest and follows
periods. restrictions
Keep fluids To encourage applied.
within reach of fluid intake
client.
Teach client To prevent
perineal self- development of
care. perineal
infections
Administer This drug helps
oxytocin as in the
prescribed by contraction of
physician the uterus.
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
Subjective: Risk for ineffective After 8 hours of Independent: After 8 hours of
Patient is still tissue perfusion nursing Monitor amount To measure the nursing
bleeding after a related to interventions , of bleeding by amount of blood interventions, the
week of giving birth hemorrhage. the patient will weighing all loss. patient was able to
Restlessness demonstrate pads. Early demonstrate
Confusion adequate Frequently recognition of adequate perfusion
Irritability perfusion and monitor vital possible and stable vital
stable vital signs. signs. adverse effects signs.
Objective: allows for
V/S taken as prompt
follows: Massage the intervention.
T: 36.7 uterus. To help expel
P: 107 clots of blood
R: 23 and it is also
Bp: 100/70 used to check
the tone of the
uterus and
ensure that it is
clamping down
Place the to prevent
mother in excessive
Trendelenberg bleeding.
position. Encourages
venous return to
facilitate
circulation, and
Provide comfort prevent further
measure like bleeding.
back rubs, deep Promotes
breathing. relaxation and
Instruct in may enhance
relaxation or patient’s coping
visualization abilities by
exercises. refocusing
attention.
Collaborative:
Administer oxygen
as indicated.
To supply
adequate
oxygen to the
fetus and
Administer mother and
medication as prevents further
indicated complication.
(oxytocin) To promote
contraction and
prevents further
bleeding.
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
Subjective: Anxiety related to After 8 hours of Independent: After 8 hours of
Confusion, knowledge deficit nursing Encourage Verbalization of nursing
Restlessness regarding intervention, the the client and anxiety provides an intervention, the
Patient procedures, client can or the family opportunity client is able to
displays management verbalize anxiety to identify to clarify information, verbalize anxiety
increased and disease and appear feelings of correct misconception and appears
apprehension condition as relaxed with anxiety. s relaxed with
and evidenced by stable vital and gain perspective, stable vital signs.
uncertainty patient asks signs. facilitating the
Objective: many question problem-solving
Pallor about the process.
VS taken as follows: disease Stay with the To help in maintaining
T: 36.5 client by emotional control in
P: 110 providing a response to the
R: 22 calm, empathic changing physiological
BP: 120/90 and supportive status. Helps in
attitude. lessening
interpersonal
transmission of
feelings.
Provide Giving accurate
information information can lessen
about the the anxiety and to
treatment identify what is reality
regimen and based.
effectiveness of
the
interventions.
Evaluate Changes in the vital
physiological signs may be due to
response to physiologic responses,
postpartum but they can be
hemorrhage aggravated by
psychological factors
You might also like
- Final NCP For PostpartumDocument8 pagesFinal NCP For PostpartumJam Ali100% (1)
- Hernandez NCP Drug StudyDocument7 pagesHernandez NCP Drug StudyEliza Joyce HernandezNo ratings yet
- NCP Post PartumDocument2 pagesNCP Post PartumsteffiNo ratings yet
- NCP Placenta PreviaDocument2 pagesNCP Placenta PreviaCathy CnlsNo ratings yet
- Pre EclampsiaDocument3 pagesPre EclampsiaJon Sayson100% (1)
- After 8 Hours of Nursing Interventions Patient Will Be Able To: Demonstrate Adequate Perfusion. Demonstrate Stable Vital SignsDocument3 pagesAfter 8 Hours of Nursing Interventions Patient Will Be Able To: Demonstrate Adequate Perfusion. Demonstrate Stable Vital Signsroma_elonaNo ratings yet
- NCP-Risk For InfectionDocument2 pagesNCP-Risk For InfectionJea Joel Mendoza100% (1)
- Fluid Volume Deficit Secondary To Post Partum HemorrhageDocument3 pagesFluid Volume Deficit Secondary To Post Partum HemorrhagePatricia Franco100% (1)
- Uterine Atony - NCPDocument17 pagesUterine Atony - NCPMonica BorjaNo ratings yet
- Precipitous Labor/Delivery or Unplanned/Out-of-Hospital DeliveryDocument7 pagesPrecipitous Labor/Delivery or Unplanned/Out-of-Hospital DeliveryLei Ortega100% (1)
- Nursing Care Plan For Postpartum HemorrhageDocument2 pagesNursing Care Plan For Postpartum HemorrhageDianne Mae100% (1)
- NCP: Labor Stage 1 Transition Phase (Deceleration)Document7 pagesNCP: Labor Stage 1 Transition Phase (Deceleration)JavieNo ratings yet
- Predisposing Factors:: Placenta Previa Lower Uterine SegmentDocument11 pagesPredisposing Factors:: Placenta Previa Lower Uterine Segmentjhachers100% (1)
- Ectopic and Abortion NCPDocument6 pagesEctopic and Abortion NCPElizabeth Quiñones100% (1)
- Preventing Infection Through EducationDocument3 pagesPreventing Infection Through EducationGian Arlo Hilario Castro100% (6)
- NCP For EclampsiaDocument6 pagesNCP For EclampsiaXtine Soliman Zamora100% (3)
- NCP Gestational HypertensionDocument2 pagesNCP Gestational Hypertensionshila_glangNo ratings yet
- Abruptio Placenta NCPDocument2 pagesAbruptio Placenta NCPNichole Audrey Saavedra100% (1)
- Nursing Care Plan for Postoperative ComfortDocument1 pageNursing Care Plan for Postoperative ComfortAngela DancelNo ratings yet
- NCP Pre EclampsiaDocument2 pagesNCP Pre EclampsiaFarrah Grace Birowa0% (1)
- Care Plan PostpartumDocument2 pagesCare Plan Postpartumteokie082483% (6)
- NCP Case 3Document3 pagesNCP Case 3boomer SeargeNo ratings yet
- NCP ObDocument2 pagesNCP ObtimmyNo ratings yet
- Nursing Care Plan Abrubtio PlacentaDocument2 pagesNursing Care Plan Abrubtio PlacentaLei Ortega0% (1)
- NCP PPHDocument2 pagesNCP PPHmikee-berredo-9975No ratings yet
- NCP On Postpartum MotherDocument13 pagesNCP On Postpartum MotherLenjun89% (57)
- NCP For Ectopic PregnancyDocument4 pagesNCP For Ectopic PregnancyClarissa_Dante_735850% (4)
- Abruptio Placenta NCP 2 FinalDocument19 pagesAbruptio Placenta NCP 2 FinalTin100% (1)
- Nursing Diagnosis: May Be Related To: Fluid Volume Deficit (Isotonic)Document26 pagesNursing Diagnosis: May Be Related To: Fluid Volume Deficit (Isotonic)Ric Nacional75% (4)
- Pain - Post Partum MotherDocument2 pagesPain - Post Partum Motherulrikov91% (11)
- Nursing Care Plan Abruptio PlacentaeDocument2 pagesNursing Care Plan Abruptio PlacentaeWann WannNo ratings yet
- Nursing Care Plan AbortionDocument4 pagesNursing Care Plan AbortionJane Casiquin100% (1)
- Nursing Care Plan For Pregnancy Induced HypertensionDocument9 pagesNursing Care Plan For Pregnancy Induced HypertensionMurugham DineshNo ratings yet
- Nursing Care Plan 1Document12 pagesNursing Care Plan 1Disyme Duron AzuresNo ratings yet
- Postpartum CareDocument9 pagesPostpartum CareFreida Marie PiczonNo ratings yet
- College of Nursing: Rupture of Membrames On Full Term PrimigravidaDocument7 pagesCollege of Nursing: Rupture of Membrames On Full Term PrimigravidaJulia BanagodosNo ratings yet
- NCP For Delivery RoomDocument4 pagesNCP For Delivery RoomGiselle EstoquiaNo ratings yet
- NCP Abruptio PlacentaDocument2 pagesNCP Abruptio PlacentaCarson Birth100% (1)
- NCP Ineffective Tissue Perfusion (Eclampsia)Document1 pageNCP Ineffective Tissue Perfusion (Eclampsia)Jenny AjocNo ratings yet
- De Guzman, Cameron Josh B. APRIL 26, 2021 2BSN-B RLENCM109Document4 pagesDe Guzman, Cameron Josh B. APRIL 26, 2021 2BSN-B RLENCM109Cameron De GuzmanNo ratings yet
- NCP GDMDocument2 pagesNCP GDMboomNo ratings yet
- NCP Alterations in Normal LaborDocument9 pagesNCP Alterations in Normal LaborCameron De GuzmanNo ratings yet
- Incompetent NCPDocument1 pageIncompetent NCPJohn Francis Velasco100% (6)
- Ectopic PregnancyDocument2 pagesEctopic PregnancyRex Dave Guinoden100% (1)
- NCP: Gestational HTN - Preeclampsiaeclampsia - Hellp SyndromeDocument23 pagesNCP: Gestational HTN - Preeclampsiaeclampsia - Hellp SyndromeKath100% (2)
- Retained Placental FragmentsDocument9 pagesRetained Placental FragmentsHannah Laput100% (2)
- Nursing Care Plan For Knowledge DeficitDocument3 pagesNursing Care Plan For Knowledge DeficitRegine BautistaNo ratings yet
- Nursing Care Plans (NCP) of Abruptio PlacentaDocument13 pagesNursing Care Plans (NCP) of Abruptio PlacentaKath76% (21)
- Neonatal Jaundice and Ineffective Breundiceeding Nursing Care PlanDocument3 pagesNeonatal Jaundice and Ineffective Breundiceeding Nursing Care Planpapadaad100% (1)
- Nursing Care Plan for Acute Pain ManagementDocument3 pagesNursing Care Plan for Acute Pain ManagementSheene Lysethea Sioteco AguilosNo ratings yet
- CA - Amniotic Fluid EmbolismDocument13 pagesCA - Amniotic Fluid EmbolismRodelen Maraño100% (2)
- Infection NCPDocument1 pageInfection NCPMsOrangeNo ratings yet
- NCP For Postpartum DiscomfortsDocument3 pagesNCP For Postpartum DiscomfortsCamille Maluenda - Tan0% (1)
- Post Partum Hemorrhage Nursing Care Plan PDFDocument2 pagesPost Partum Hemorrhage Nursing Care Plan PDFA sison100% (1)
- BOX 17.4 NCP Postpartum HemorrhageDocument4 pagesBOX 17.4 NCP Postpartum HemorrhageJam AliNo ratings yet
- Nursing Care Plan for Acute Renal FailureDocument3 pagesNursing Care Plan for Acute Renal FailureKian Herrera100% (1)
- Nursing Care Plan for Fluid Volume DeficitDocument9 pagesNursing Care Plan for Fluid Volume DeficitYesha Mae MartinNo ratings yet
- NCP CKDDocument5 pagesNCP CKDDbktNo ratings yet
- Nursing Care PlanDocument11 pagesNursing Care PlanKirstin del CarmenNo ratings yet
- NCP DrugstudyDocument2 pagesNCP DrugstudyAbegail MierNo ratings yet
- October 23, 2021: by Dr. Leah SabayleDocument3 pagesOctober 23, 2021: by Dr. Leah SabayleElishaNo ratings yet
- Understanding pathophysiology of cardiovascular conditionsDocument12 pagesUnderstanding pathophysiology of cardiovascular conditionsElishaNo ratings yet
- Blank DiagramDocument1 pageBlank DiagramElishaNo ratings yet
- Media and Information Literacy Prelims Reviewer PDFDocument7 pagesMedia and Information Literacy Prelims Reviewer PDFElishaNo ratings yet
- Media and Information Literacy Prelims Reviewer PDFDocument7 pagesMedia and Information Literacy Prelims Reviewer PDFElishaNo ratings yet
- Blank DiagramDocument1 pageBlank DiagramElishaNo ratings yet
- Shock and Multi OrganDocument90 pagesShock and Multi OrganElishaNo ratings yet
- ANAPHY First Quarter ReviewerDocument27 pagesANAPHY First Quarter ReviewerReinzoCardenas100% (3)
- The Neurophysiological Cause of AutismDocument2 pagesThe Neurophysiological Cause of AutismElishaNo ratings yet
- Bioethics in Critical CareDocument80 pagesBioethics in Critical CareElishaNo ratings yet
- Maternal Perceptions On Childhood Obesity On Selected Communities in Metro ManilaDocument91 pagesMaternal Perceptions On Childhood Obesity On Selected Communities in Metro ManilaElishaNo ratings yet
- Media and Information Literacy Prelims Reviewer PDFDocument7 pagesMedia and Information Literacy Prelims Reviewer PDFElishaNo ratings yet
- Hand Hygiene Why How and When BrochureDocument7 pagesHand Hygiene Why How and When BrochureLeis FatwaNo ratings yet
- Physical Science Reviewer EssentialsDocument16 pagesPhysical Science Reviewer EssentialsElishaNo ratings yet
- Media and Information Literacy Prelims Reviewer PDFDocument7 pagesMedia and Information Literacy Prelims Reviewer PDFElishaNo ratings yet
- Reaction Paper Rizal in DapitanDocument4 pagesReaction Paper Rizal in DapitanTatlonghariChristine79% (28)
- Physical Science Reviewer EssentialsDocument16 pagesPhysical Science Reviewer EssentialsElishaNo ratings yet
- Chapter 1: The Human OrganismDocument26 pagesChapter 1: The Human OrganismElishaNo ratings yet
- Ethics in ResearchDocument4 pagesEthics in ResearchElishaNo ratings yet
- Hand Hygiene Why How and When BrochureDocument7 pagesHand Hygiene Why How and When BrochureLeis FatwaNo ratings yet
- Work ImmDocument2 pagesWork ImmElishaNo ratings yet
- Fundamentals of FaithDocument16 pagesFundamentals of FaithAlessandraNo ratings yet
- Work ImmDocument2 pagesWork ImmElishaNo ratings yet
- Higher Education: Jose Rizal in Ateneo Municipal and Universidad de Santo TomasDocument41 pagesHigher Education: Jose Rizal in Ateneo Municipal and Universidad de Santo TomasElishaNo ratings yet
- Safety ProtocolsDocument6 pagesSafety ProtocolsElishaNo ratings yet
- Case Study ArticleDocument4 pagesCase Study ArticleElishaNo ratings yet
- Practical Research 2 Theoretical and Conceptual Framework Jerry V. Manlapaz, RN, PHD, Edd, LPT Theoretical and Conceptual FrameworkDocument5 pagesPractical Research 2 Theoretical and Conceptual Framework Jerry V. Manlapaz, RN, PHD, Edd, LPT Theoretical and Conceptual FrameworkElishaNo ratings yet
- Edited Risk For MaternalDocument2 pagesEdited Risk For MaternalElisha100% (1)
- The Indolence of Filipinos: Causes and SolutionsDocument2 pagesThe Indolence of Filipinos: Causes and SolutionsElishaNo ratings yet
- Kaleidoscope-Patti Heale Feb 21 Placenta Previa PDFDocument66 pagesKaleidoscope-Patti Heale Feb 21 Placenta Previa PDFElishaNo ratings yet
- Health-Related Quality of Life ScaleDocument4 pagesHealth-Related Quality of Life ScaleMihaela Cosmina NiculescuNo ratings yet
- Mercury Poisoning: An Experience in HUSMDocument45 pagesMercury Poisoning: An Experience in HUSMfadhylNo ratings yet
- Malaria PresentationDocument11 pagesMalaria PresentationGalina TiscencoNo ratings yet
- Thrombosis Prevention by SlidesgoDocument67 pagesThrombosis Prevention by SlidesgoRohanNo ratings yet
- A Sonographic Sign of Moderate ToDocument5 pagesA Sonographic Sign of Moderate ToDivisi FER MalangNo ratings yet
- LES y Enf CardiovascularDocument15 pagesLES y Enf CardiovascularSMIBA MedicinaNo ratings yet
- Guaphan Syrup Patient Information LeafletDocument1 pageGuaphan Syrup Patient Information Leafletpharmacia1.comNo ratings yet
- Bicillin C-R Penicillin G: Drug StudyDocument1 pageBicillin C-R Penicillin G: Drug StudyChristine Pialan Salimbagat100% (1)
- CHCECE002 - Ensure The Health and Safety of ChildrenDocument8 pagesCHCECE002 - Ensure The Health and Safety of ChildrenGisele SilvestreNo ratings yet
- Dental Management of Medically Compromised Patients 2Document85 pagesDental Management of Medically Compromised Patients 2Mohamed KhaledNo ratings yet
- Ncbi Ascorbic AcidDocument7 pagesNcbi Ascorbic AcidOsunlola GabrielNo ratings yet
- Blood ChecklistDocument2 pagesBlood Checklistfrosthyuuga10No ratings yet
- Fhu PDFDocument3 pagesFhu PDFdanielep1No ratings yet
- TESDA COVID-19 Test (Answer Keys)Document12 pagesTESDA COVID-19 Test (Answer Keys)ash mizushiNo ratings yet
- Mental HealthDocument9 pagesMental HealthPatrick JoshuaNo ratings yet
- Evaluation of Antidermatophytic Activity of Piper Betle, Allamanda Cathertica and Their Combination: An in Vitro and in Vivo StudyDocument8 pagesEvaluation of Antidermatophytic Activity of Piper Betle, Allamanda Cathertica and Their Combination: An in Vitro and in Vivo Studyfrez_kingdomNo ratings yet
- MNJ ToastDocument4 pagesMNJ ToastRichard SuherlimNo ratings yet
- GonorreheaDocument5 pagesGonorreheaSunny OZNo ratings yet
- Large For Gestational Age (LGA)Document4 pagesLarge For Gestational Age (LGA)Aira AlaroNo ratings yet
- Ha 1 15Document15 pagesHa 1 15cianixNo ratings yet
- Metanalisis Feline Gingivo EstomatitisDocument10 pagesMetanalisis Feline Gingivo EstomatitisPatriciaNo ratings yet
- Tubulointerstitial nephritis: an overview of kidney diseases involving the tubules and interstitiumDocument34 pagesTubulointerstitial nephritis: an overview of kidney diseases involving the tubules and interstitiumIaros OlgaNo ratings yet
- BOTOX LectureDocument74 pagesBOTOX LectureAnonymous 8hVpaQdCtr100% (6)
- 07 Mycology00.NewDocument61 pages07 Mycology00.NewvriliadiarNo ratings yet
- Introduction To ECG: Presenter: Emiacu Kenneth Facilitator: Dr. Ssebuliba MosesDocument36 pagesIntroduction To ECG: Presenter: Emiacu Kenneth Facilitator: Dr. Ssebuliba MosesNinaNo ratings yet
- Lary SprayDocument7 pagesLary SprayMedley SinkhaiNo ratings yet
- Indriyaaneekam of Charaka Indriya Sthana - An Explorative StudyDocument13 pagesIndriyaaneekam of Charaka Indriya Sthana - An Explorative StudyPrasad MamidiNo ratings yet
- 01MakeTheGrade1 ExtraListenPrac1Document1 page01MakeTheGrade1 ExtraListenPrac1sergio ruizherguedas0% (1)
- 12 Home Remedies For Toothaches That Actually Work - Klement Family DentalDocument1 page12 Home Remedies For Toothaches That Actually Work - Klement Family DentalStephanie AtienzaNo ratings yet
- RESIT 2014 PAPER: CERVIX, BREAST, THYROID, HEART DISEASE MCQSDocument3 pagesRESIT 2014 PAPER: CERVIX, BREAST, THYROID, HEART DISEASE MCQSDr-Irfan Habib100% (1)