Professional Documents
Culture Documents
Mguide NeonatResv4
Uploaded by
Ashok SubramaniumOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mguide NeonatResv4
Uploaded by
Ashok SubramaniumCopyright:
Available Formats
Neonatal resuscitation
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
Document title: Neonatal resuscitation
Publication date: November 2009
Document number: NN0911.5-V1-R11
Replaces document: New document
Author: Statewide Maternity and Neonatal Clinical Guidelines Program
Medical, midwifery and nursing staff in Queensland public and private
Audience:
maternity services
Exclusions: Nil
Review date: November 2011
Statewide Maternity and Neonatal Clinical Network
Endorsed by:
Patient Safety and Quality Executive Committee
Statewide Maternity and Neonatal Clinical Guidelines Program
Contact: Email: MN-Guidelines@health.qld.gov.au
URL: http://www.health.qld.gov.au/cpic/resources/mat_guidelines.asp
Disclaimer
These guidelines have been prepared to promote and facilitate standardisation and
consistency of practice, using a multidisciplinary approach.
Information in this guideline is current at time of publication.
Queensland Health does not accept liability to any person for loss or damage incurred as a
result of reliance upon the material contained in this guideline.
Clinical material offered in this guideline does not replace or remove clinical judgement or the
professional care and duty necessary for each specific patient case.
Clinical care carried out in accordance with this guideline should be provided within the
context of locally available resources and expertise.
This Guideline does not address all elements of standard practice and assumes that
individual clinicians are responsible to:
• Discuss care with consumers in an environment that is culturally appropriate and
which enables respectful confidential discussion. This includes the use of interpreter
services where necessary
• Advise consumers of their choice and ensure informed consent is obtained.
• Provide care within scope of practice, meet all legislative requirements and maintain
standards of professional conduct
• Apply standard precautions and additional precautions as necessary, when delivering
care
• Document all care in accordance with mandatory and local requirements
Refer to online version, destroy printed copies after use Page 2 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
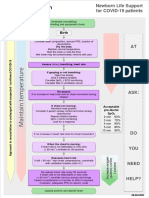
Flow Chart: Neonatal resuscitation
tion
Birth
Approximate
time
Routine Care:
Term gestation? Dry baby & provide
Yes
Amniotic fluid clear? warmth
Assessment Breathing or crying? Clear airway only if
needed
No
¾ Dry & stimulate (unless preparing to A Airway
intubate for meconium) • Positioning
30 sec A ¾ Position head & neck to open airway; • Suction trachea ‐ if
¾ Clear airway (as necessary)* meconium stained fluid and
¾ Provide warmth baby is not vigorous
Breathing,
HR >100 Observational care: • Endotracheal intubation or
Evaluation and Pink Routine care nasal or oral airway if
Assess: breathing, HR, and color appropriate for persistent obstruction
gestation & risk factors
Breathing, HR >100 Encourage parental
but cyanotic interaction
Pink
Apneic or B Breathing
¾ Continue • PPV at 40‐60 breaths/minute
30 sec HR <100
assessment • Observe chest rise
Persistent cyanosis
Effective ventilation,
B ¾ Provide positive‐pressure ventilation* HR >100 and Pink
C Circulation
Post resuscitation care:
Evaluation HR <60 HR >60 • 90 compression coordinated
Ongoing evaluation/
with 30 breaths/minute
¾ Provide positive‐pressure ventilation* monitoring in neonatal
C • (3 compressions to 1 breath
30 sec ¾ Administer chest compressions unit (arrange transfer
every 2 seconds)
if necessary)
• Compress 1/3 of AP chest
Encourage parental
Evaluation HR <60 diameter
interaction
• Increase inspired oxygen to
100%
D ¾ Administer
adrenaline and/or
volume*
D Drugs
• See attached table
Recheck effectiveness of:
Ventilation
Chest Compressions
Endotracheal intubation
Adrenaline delivery
Consider possibility of
hypovolemia
Persistent bradycardia or
cyanosis or failure to ventilate
Consider: * Endotracheal intubation
Airway malformations Absent HR for may be considered at several
Lung problems such as >10 minutes steps
o Pneumothorax HR indicates heart rate
o Diaphragmatic hernia (shown in beats per minute)
Congenital heart disease
Consider discontinuing resuscitation
th
Adapted from: Australian Resuscitation Council. Neonatal Flowchart. February 2006 and Katwinkel J. Textbook of Neonatal Resucitation. 5 ed.
The American Academy of Paediatrics. 2006.
Refer to online version, destroy printed copies after use Page 3 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
Abbreviations
bpm Beats per minute
cm Centimetres
CO2 Carbon dioxide
CTG Cardiotocograph
ETT Endotracheal tube
F French gauge
g Gram
HIE Hypoxic ischaemic encephalopathy
HR Heart rate
IV Intravenous
Kg Kilograms
mg Milligram
mL Millilitre
mm Millimetres
PIP Peak inspiratory pressure
PPV Positive pressure ventilation
Rh Rhesus
sec Seconds
UVC Umbilical venous catheter
-ve Negative
Refer to online version, destroy printed copies after use Page 4 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
Table of Contents
1 Introduction.....................................................................................................................................6
2 Clinicians attending the birth ..........................................................................................................6
3 Preparation .....................................................................................................................................7
3.1 Anticipating the need for resuscitation...................................................................................7
3.2 Communication ......................................................................................................................8
3.2.1 Maternal and neonatal clinicians .......................................................................................8
3.2.2 Parents...............................................................................................................................8
3.3 Equipment..............................................................................................................................9
4 Assessment of the newborn infant at birth ...................................................................................10
4.1 Immediate management of the newborn infant at birth .......................................................10
4.2 Endotracheal suctioning in the presence of meconium stained liquor ................................11
4.3 Free flow supplemental oxygen ...........................................................................................11
4.4 Positive pressure ventilation ................................................................................................12
4.5 Endotracheal intubation .......................................................................................................13
4.5.1 Indications for endotracheal intubation............................................................................13
4.5.2 Checking endotracheal tube position ..............................................................................13
4.6 Combined chest compression and positive pressure ventilation.........................................14
5 Drugs and volume expanders in resuscitation .............................................................................15
5.1 Vascular access...................................................................................................................15
5.2 Adrenaline 1:10,000.............................................................................................................15
5.3 Volume Expansion...............................................................................................................16
5.4 Other drugs ..........................................................................................................................16
6 Documentation .............................................................................................................................16
7 Care of the newborn after resuscitation .......................................................................................16
8 Inter-hospital transfer....................................................................................................................17
9 Care of clinicians ..........................................................................................................................17
10 Ethical issues in resuscitation of the newborn .............................................................................17
10.1 Initiating resuscitation ..........................................................................................................17
10.2 Discontinuing resuscitation ..................................................................................................17
References ..........................................................................................................................................18
Appendix A: Flowchart for endotracheal suctioning in the presence of meconium stained liquor ......19
Appendix B: Neonatal resuscitation drug guide ..................................................................................20
Appendix C: Endotracheal tube size and insertion distance ...............................................................21
Appendix D: Further notes on the use of a narcotic antagonist ..........................................................22
Appendix E: Acknowledgments ...........................................................................................................23
List of Tables
Table 1: Adrenaline via IV route .......................................................................................................... 15
Table 2: Adrenaline via ETT route....................................................................................................... 15
Table 3: Volume expanders................................................................................................................. 16
Refer to online version, destroy printed copies after use Page 5 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
1 Introduction
Definitions of newborn, neonate and infant:
• the term “newborn” refers to the infant in the first few minutes to hours following birth.1
In contrast, the neonatal period is defined as the first 28 days of life.1 Infancy includes the
neonatal period and extends through the first 12 months of life1
This guideline is intended to apply specifically to newborn infants, although many of the principles are
applicable throughout the neonatal period.
Most newborn infants are vigorous at birth:
• 5% will require some form of resuscitation at birth to begin breathing1
• 1% will require assisted ventilation to survive2
The need for neonatal resuscitation cannot always be anticipated.1,2 Maternity facilities providing
planned birthing services require:
• a suitable place to resuscitate a newborn infant
• appropriate neonatal resuscitation equipment
• clinicians trained in neonatal resuscitation1
2 Clinicians attending the birth
Neonatal resuscitation is a team effort that requires a coordinated approach.2 There should be at
least one clinician dedicated to the care of each newborn infant.1,2 Two clinicians are recommended if
it is anticipated that the newborn infant will require advanced resuscitation.1
All clinicians attending the birth to care for the newborn infant must:
• be familiar with the available neonatal resuscitation equipment1
• be appropriately trained in basic neonatal resuscitation techniques1
• have demonstrated and been assessed as competent in basic neonatal resuscitation
• maintain competence through continued practice and review
A clinician trained in advanced neonatal resuscitation skills including:
• basic neonatal resuscitation
• intubation
• intravenous (IV) cannulation
• the use of drugs and fluids
should be accessible for normal low risk births, and be in attendance at all births with significant
maternal and/or fetal risk factors that predispose to the need for neonatal resuscitation.1
All clinicians must implement standard precautions according to hospital Infection Control
Guidelines.1,2
Refer to online version, destroy printed copies after use Page 6 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
3 Preparation
3.1 Anticipating the need for resuscitation
A variety of maternal, fetal and intrapartum circumstances can increase the risk of needing
resuscitation at birth.
Maternal risk factors include1:
• prolonged rupture of membranes (greater than 24 hours)
• bleeding in second or third trimester
• severe pregnancy induced hypertension
• chronic hypertension
• substance abuse
• drug therapy including:
o lithium
o magnesium
o adrenergic blocking agents
o narcotics
• diabetes mellitus
• chronic illness including:
o anaemia
o cyanotic congenital heart disease
• maternal infection
• chorioamnionitis
• heavy sedation
• previous fetal or neonatal death
• no prenatal care
Fetal risk factors include1:
• twins or higher order multiples
• preterm gestation (especially less than 35 weeks)
• post term gestation (greater than 41 weeks)
• large for dates
• fetal growth restriction
• Rh or other blood group isoimmunisation especially if there is fetal anaemia
• polyhydramnios and oligohydramnios
• reduced fetal movement before onset of labour
• congenital abnormalities which may effect breathing
• intrauterine infection
Intrapartum risk factors include1:
• abnormalities of fetal heart rate detected by auscultation, sonography or cardiotocograph
(CTG)
• abnormal presentation
• prolapsed cord
• prolonged labour or prolonged second stage of labour
• precipitate labour
• antepartum haemorrhage including:
o abruption
o placenta praevia
o vasa praevia
• thick meconium in the amniotic fluid
• narcotic administered to the mother within 4 hours of birth
• forceps birth
• vacuum-assisted birth
• caesarean section under general anaesthetic
Refer to online version, destroy printed copies after use Page 7 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
3.2 Communication
3.2.1 Maternal and neonatal clinicians
Effective communication between maternal and neonatal clinicians is vital to ensure optimal outcome
for the newborn infant and parents.
As a minimum requirement, the following information should be provided by maternal clinicians to
neonatal clinicians1:
• gestation
• expected number of newborn infants, if multiple birth
• reason this is a high risk birth
• presence of meconium in the amniotic fluid
• assessments of fetal heart rate variability
• any known congenital abnormalities
• results of screening, including screening for perinatally transmitted viruses or bacteria
(e.g. Group B Streptococcus)
• maternal medications and medical conditions
3.2.2 Parents
It is important that whenever possible, the neonatal team introduce themselves to the parents before
the birth,1 and take every opportunity to1,2:
• prepare parents for the possibility of resuscitation when it is anticipated
• keep parents informed during and after the resuscitation
• give information appropriately
• facilitate early contact between parents and their newborn infant
Where possible, a senior clinician should provide information to the parents.1
In cases of potentially lethal fetal malformations or extreme prematurity, parents must be included in
decisions about the extent of the resuscitation whenever possible.1
Refer to online version, destroy printed copies after use Page 8 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
3.3 Equipment
The following resuscitation equipment and drugs should be readily available in the areas of hospitals
where infants are born or receive neonatal care.1,2
Check equipment regularly according to hospital policy:
• to ensure it is complete and operational1
• before any resuscitation1
A clear record documenting the checking procedure should be maintained for each set of
resuscitation equipment and drugs.
Resuscitation equipment:
• Firm padded resuscitation surface
• Overhead warmer
• Light for the area
• Warm towel or other covering
• Clock with timer in seconds
• Stethoscope (neonatal preferred)
• Polyethylene bag or wrap for infants less than1500 g1,2,3
• Suction source, tubing and size 6 F, 8 F, and either 10 F or 12 F suction catheters
• Meconium aspirators
• Medical gases:
o oxygen source with flow meter and tubing
o air source with flow meter and tubing
o air/oxygen blender (if available)
• Positive pressure ventilation device, either of:
o flow-inflating bag with manometer OR
o T-Piece resuscitation device or Neopuff1 AND
o self-inflating neonatal resuscitation bag (240 mL) with an oxygen reservoir and
pressure pop-off valve
• Face masks (range of sizes suitable for premature and term infants)
• Oropharyngeal airways (sizes 00 and 0)
• Laryngeal mask airway (not recommended for use in infant less than 1500 g)1,2,4 (optional)
• Intubation equipment:
o endotracheal tube (ETT) (uncuffed sizes 2.5, 3.0, 3.5, 4.0)
o ETT introducer/stylet
o laryngoscope with straight blades (sizes 00, 0, 1 ), spare globes and batteries. If
there is strong local preference, curved blades (sizes 0, 1) can be included in addition
(not instead of straight blades)
o Magill forceps (neonatal size)
o sterile scissors
o tape and/or device to secure ETT
o end-tidal carbon dioxide (CO2) detector
• IV access equipment:
o umbilical venous catheter (UVC) kit (including UVC size 5F)
o peripheral IV cannulation kit
o suitable skin preparation solution
o tapes/devices to secure UVC/IV cannula
o syringes and needles
• Feeding tubes (sizes 6F, 8F)
• Pulse oximeter (optional)
Resuscitation Drugs:
• Adrenaline 1:10 000 - concentration (0.1 mg/mL)
• Volume expander:
o 0.9% sodium chloride
Refer to online version, destroy printed copies after use Page 9 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
4 Assessment of the newborn infant at birth
Assessing the need for resuscitation should begin immediately after birth and proceed throughout the
resuscitation.1 Evaluation and intervention are simultaneous processes, especially when more than
one resuscitator is present.1
For clarity this process is described as a sequence of distinct steps as shown in the Neonatal
Resuscitation Flowchart, adapted from the Australian Resuscitation Council and American Academy
of Paediatrics Neonatal Resuscitation Program Flowcharts.1,2
4.1 Immediate management of the newborn infant at birth
At birth:
• assess the newborn infant to determine the need for resuscitation by reviewing1:
o response to stimulation
o breathing
o heart rate
o tone
If the newborn infant is:
• term gestation, breathing effectively, heart rate is greater than 100 beats per minute
(bpm) and is beginning to look pink:
o place the newborn infant:
skin to skin on the mothers chest or abdomen and cover with warm blankets
or wrap the newborn infant in warm blankets and give to the mother1
o provide routine care2:
ongoing observation of breathing, activity and colour, to determine the need
for additional intervention
• breathing effectively, heart rate is greater than 100 bpm, but appears centrally
cyanosed:
o place the newborn infant under an overhead warmer
o continue assessment, including commencing oxygen saturation monitoring if
possible. If the infant still appears centrally cyanosed or has oxygen saturation less
than 85% at 5 minutes, commence supplemental oxygen2 [refer to section 4.3]
• infant has absent or ineffective breathing, has low tone, or is bradycardic:
o place the newborn infant under a radiant warmer
o position the newborn infant to open the airway, clear the airway as necessary1,2
[refer to section 4.2 if meconium stained liquor present]
o stimulate the newborn infant by drying with warm towels1,2
o assess:
heart rate1,2 by listening with a stethoscope (apply pulse oximeter if
available)1
breathing1,2
colour
o commence positive pressure ventilation (PPV) if1,2:
the infant remains apnoeic
does not breathe effectively and/or
the heart rate is less than 100 bpm
If the newborn infant is:
• preterm:
o place the newborn infant under a radiant warmer:
if less than 28 weeks gestation or less than 1500 g cover newborn infant’s
body with a polyethylene wrap or carefully place the infant in a polyethylene
bag (with hole cut for the head), ensuring the newborn infant’s head is clear
of the bag1,2,3
o assess and manage as above2
Refer to online version, destroy printed copies after use Page 10 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
4.2 Endotracheal suctioning in the presence of meconium stained liquor
The need for endotracheal suctioning in the presence of meconium is based on the newborn infant’s
level of activity at birth.1.2
If the newborn infant has meconium stained liquor and is vigorous at birth, endotracheal suctioning is
not required.1
If the amniotic fluid contains thick meconium and the newborn infant has more than one of1,2:
• absent or depressed respirations
• decreased muscle tone
• a heart rate less than 100 bpm
suction meconium from the mouth and pharynx if needed and intubate and suction meconium from
the trachea, prior to stimulating or drying the newborn infant.1
If no meconium is recovered, do not repeat the procedure,2 continue with resuscitation.
If meconium is recovered, and the infant is not yet vigorous, airway suction may be repeated once.
This must be quickly accomplished as it may be a much higher priority to commence resuscitation.1
If there is no-one skilled at intubation present at birth, proceed immediately with other resuscitation
steps as needed. [refer to Appendix A: Flowchart for endotracheal suctioning in the presence of
meconium stained liquor].
4.3 Free flow supplemental oxygen
Commence free flow supplemental oxygen if the newborn infant2:
• is breathing effectively, heart rate is greater than 100 bpm but remains centrally cyanosed
at 5 minutes of age2
• is breathing effectively, heart rate is greater than 100 bpm and becomes cyanosed in the
newborn period2
• when discontinuing PPV:
o gradually withdraw free flow supplemental oxygen until the newborn infant remains
pink while breathing room air2
Whenever supplemental oxygen is used, especially in premature infants, oximetry should be
commenced as soon as possible. Oximetry should be used to guide oxygen therapy so as to avoid
oxygen saturation readings greater than 95% while supplemental oxygen is being administered. The
oxygen saturation probe should be placed on the infant’s right hand or wrist.
Refer to online version, destroy printed copies after use Page 11 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
4.4 Positive pressure ventilation
Effective ventilation is the most important aspect of neonatal resuscitation.1,2
PPV may be delivered via a face mask or ETT. Consider endotracheal intubation if ventilation via a
face mask is ineffective.1
Call for assistance if planning to commence PPV.
Commence PPV if the newborn infant1,2:
• remains apnoeic
• does not breathe effectively and/or
• the heart rate is less than 100 bpm
Commence PPV with air1,2,5 (if not available use oxygen1) at a rate at of 40 - 60 breaths per minute.1,2
After 30 seconds of PPV reassess the newborn infant’s1:
• breathing
• heart rate
• colour:
o if cyanosis is not resolving:
inspired oxygen concentration can be increased
oxygen saturation monitoring is recommended
If the infant’s:
• heart rate is greater than 100 bpm and the newborn infant is breathing effectively:
o discontinue PPV1,2
o commence free flow supplemental oxygen if necessary [refer to section 4.3].
o provide observational care1,2:
cardio-respiratory and vital signs monitoring during immediate newborn
period as appropriate for gestation and risk factors
encourage newborn infant/parent interaction
• heart rate is greater than 100 bpm but the newborn infant is not breathing
effectively:
o continue to provide PPV
o consider endotracheal intubation
• heart rate is less than 100 bpm or the chest wall does not rise with each inflation:
check2:
o airway patency
o seal between mask and face
o ventilation device is functional
o air/oxygen delivery (not needed for self-inflating bag)
o consider increasing positive inspiratory pressure (PIP)
o consider endotracheal intubation
then
o continue PPV with supplementary oxygen if necessary
Refer to online version, destroy printed copies after use Page 12 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
4.5 Endotracheal intubation
Neonatal endotracheal intubation should only be attempted by clinicians with appropriate training and
experience in the procedure. If there is no-one skilled at intubation present continue positive pressure
ventilation via a face mask.
4.5.1 Indications for endotracheal intubation
Consider endotracheal intubation at any stage during neonatal resuscitation for:
• tracheal suctioning for meconium1,2
• no detectable heart rate at birth1
• congenital abnormalities (e.g. diaphragmatic hernia)2
• inadequate breathing effort1,2
• persistent apnoea1
• inadequate response to bag and mask ventilation1,2
• coordination of chest compressions and ventilation when resuscitation is prolonged2
• administration of endotracheal medications, such as adrenaline or artificial surfactant
(premature infants)
4.5.2 Checking endotracheal tube position
ETT placement should always be checked clinically.1,2
Correct ETT placement is confirmed by1:
• visual inspection of the ETT passing through the larynx
• misting in the ETT during expiration (usually visible for only the first few exhaled breaths)
• using a stethoscope to listen for similar sounds of PPV in both axillas
• colour change visible with an end-tidal CO2 detector
Incorrect ETT placement may be indicated by1:
• the absence of misting in the ETT
• no chest wall movement with PPV
• no improvement in the newborn infant’s colour and/or heart rate
• no detection of expired CO2
• the absence of sounds of PPV in the axillas
Once the infant is stabilised, obtain a chest X-ray to confirm ETT position.1,2
ETT size and insertion length are based on the infant’s weight1,2 [refer to Appendix C].
Refer to online version, destroy printed copies after use Page 13 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
4.6 Combined chest compression and positive pressure ventilation
Commence chest compressions if the heart rate remains less than 60 bpm after 30 seconds of
effective PPV.1,2
Administer 100% oxygen if chest compressions are required.
Synchronise chest compressions and PPV at a 3:1 ratio of 90 compressions and 30 breaths to
achieve 120 events per minute1,2 by either the:
• 2 thumb technique1,2 (recommended technique when two clinicians available)1
• 2 finger technique1,2
After 30 seconds of synchronised chest compressions and PPV reassess the newborn infant’s1:
• heart rate
• breathing
• colour
If the newborn infant’s:
• heart rate is greater than 100 bpm and the newborn infant is breathing effectively:
o discontinue chest compressions
o discontinue PPV (this may be best done after admission to a neonatal unit and
measurement of blood gases)
o commence free flow supplemental oxygen as indicated [refer to section 4.3]
o when stabilised, transfer to an appropriate level nursery
• heart rate increases to greater than 60 bpm but the newborn infant is not breathing
effectively:
o discontinue chest compressions1,2
o continue PPV at 40 - 60 breaths per minute1,2
o consider endotracheal intubation
o when stabilised, transfer to an appropriate level nursery
• heart rate remains less than 60 bpm:
o check effectiveness of:
PPV
chest compressions
endotracheal intubation
o administer IV adrenaline after 30 seconds of effective combined chest compressions
and PPV1,2:
adrenaline may be given vie ETT while IV access is obtained1,2
o consider administering volume expander1
Every 30 seconds reassess the newborn infant’s2:
• breathing
• heart rate
• colour
If the newborn infant’s:
• heart rate remains less than 60 bpm despite effective PPV and cardiac compressions:
o continue synchronised chest compressions and PPV
o repeat adrenaline every 3 - 5 minutes1
o consider administering volume expander1
o recheck effectiveness of:
PPV2
chest compressions2
endotracheal intubation2
adrenaline delivery2
o insert an orogastic tube, leaving it open to free drainage to decompress the stomach2
o consider potential causes of persistent bradycardia or cyanosis or failure to ventilate:
mechanical blockage of airway (meconium, mucus, malformation)2
impaired lung function (pneumothorax, diaphragmatic hernia, prematurity)2
Consider ceasing resuscitation after 10 minutes of maximal resuscitation, if the newborn infant has
not responded with any measurable heart rate1,2 [refer to section 10].
Refer to online version, destroy printed copies after use Page 14 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
5 Drugs and volume expanders in resuscitation
5.1 Vascular access
Preferred vascular access is via the umbilical vein,1,2 alternative access is via:
• peripheral veins
• femoral veins
If venous access is unachievable consider intraosseous access.1,2
5.2 Adrenaline 1:10,000
Adrenaline is indicated if the heart rate remains less than 60 bpm despite 30 seconds of effective
PPV and cardiac compressions.1,2
When possible, adrenaline should be administered intravenously.1 If the first dose has been given via
an endotracheal tube and the heart rate remains less than 60 bpm, give further dose(s) via the
umbilical vein if possible.
Table 1: Adrenaline via IV route
Adrenaline 1:10,000
Route Intravenous
Method of Rapid bolus followed by 0.9% sodium chloride flush
administration
Dose 0.01 - 0.03 mg/kg equates to 0.1 - 0.3 mL/kg
Frequency Repeat every 3 - 5 minutes, if the heart rate remains less than 60 bpm
despite effective PPV and cardiac compressions
Dilution Not required
Table 2: Adrenaline via ETT route
Adrenaline 1:10,000
Route ETT
Method of Inject into ETT, immediately provide PPV
administration
Dose 0.03 - 0.1 mg/kg equates to 0.3 - 1.0 mL/kg
Frequency Repeat every 3 - 5 minutes, if the heart rate remains less than 60 bpm
despite effective PPV and cardiac compressions
Dilution Not required
Refer to online version, destroy printed copies after use Page 15 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
5.3 Volume Expansion
Volume replacement is not routine in neonatal resuscitation.
Consider intravascular fluids if there is suspected blood loss and/or the newborn infant appears
shocked and has not responded adequately to other resuscitative interventions.1,2
Table 3: Volume expanders
Volume Expanders
• 0.9% Sodium chloride1,2 or (if suspicion or evidence of recent blood loss) O Rh negative
blood
Route Intravenous
Method of Infusion over 5 - 10 minutes1,2
administration
Dose 10 mL/kg
Frequency May be repeated if only minimal improvement
Dilution Not required
5.4 Other drugs
Artificial surfactant can have a role in improving lung function during the resuscitation of some
premature infants.
There is insufficient data to recommend routine use of sodium bicarbonate during neonatal
resuscitation.1,2
Naloxone should not be used as part of the initial resuscitation of newborns with respiratory
depression in the delivery room.1,2 [for further explanation refer to Appendix D].
6 Documentation
Comprehensive contemporaneous documentation of neonatal resuscitation is required for
medicolegal and clinical reasons.1 When possible, it is recommended that one clinician is appointed
to document the time, intervention and newborn infant’s response during the resuscitation.
Ensure documentation is complete.
7 Care of the newborn after resuscitation
Cord blood gases should be measured in every resuscitated newborn infant as the most objective
way to assess the condition just before birth.1 Collect umbilical cord arterial blood in a heparinised
syringe and analyse within 30 minutes of birth.1
The newborn infant who has required resuscitation remains at risk and should be cared for in an
environment where appropriate evaluation and care can be provided including monitoring of1:
• oxygen saturation
• temperature
• heart rate
• respiratory rate and pattern
• blood glucose measurement
• blood gas analysis
• blood pressure
Term asphyxiated newborn infants with hypoxic ischaemic encephalopathy (HIE) may meet the
criteria for cooling,6 this should be discussed with a Neonatologist after initial stabilisation.
Refer to online version, destroy printed copies after use Page 16 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
8 Inter-hospital transfer
If the birth facility is unable to provide an appropriate level of post resuscitation monitoring and
support, transfer the newborn infant to an appropriate higher level facility.
Once the decision has been made to transfer the infant to a higher level facility, this will be
coordinated by Retrieval Services Queensland (RSQ) and a Neonatal medical coordinator, by calling
1300 799 127.
9 Care of clinicians
Support clinicians after resuscitation by:
• providing formal and informal opportunities to debrief
• providing information regarding local hospital support services
• providing feedback to the referring hospital, if the infant is transferred
10 Ethical issues in resuscitation of the newborn
10.1 Initiating resuscitation
Where unexpected anomalies are present offer full resuscitation, ongoing care can be discussed with
parent(s) after assessment of the newborn infant's condition.1,2 Examples of exceptions include
infants with1:
• anencephaly
• extremely immature infants for whom there is very little possibility of intact survival
10.2 Discontinuing resuscitation
Consider discontinuing resuscitation after 10 minutes of maximal resuscitation if an infant has not
responded with any measurable heart rate.1,2
Failure to obtain a heart rate by 10 minutes is associated with death or severe neurological
sequelae.1,2,7
Before ceasing resuscitation1:
• obtain a second opinion if immediately available
• wherever possible seek agreement with parent(s)
Refer to online version, destroy printed copies after use Page 17 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
References
1. Australian Resuscitation Council Neonatal Guidelines revised February 2006. Available
from:URLwww.resus.org.au/
2. Kattwinkel J, editor. Textbook of Neonatal Resuscitation, 5th ed. Chicago:American Academy of
Paediatrics and American Heart Association; 2006.
3. McCall EM, Alderdice FA, Halliday HL, Jenkins JG, Vohra S. Interventions to prevent
hypothermia at birth in preterm and/or low birthweight infants. Cochrane Database Syst Rev
2008;(1):CD004210.
4. Grein AJ, Weiner GM. Laryngeal mask airway versus bag-mask ventilation or endotracheal
intubation for neonatal resuscitation. Cochrane Database Syst Rev 2005 Apr 18;(2):CD003314.
5. Tan A, Schulze A, O’Donnell CPF, Davis PG. Air versus oxygen for resuscitation of infants at
birth. Cochrane Database of Systematic Reviews 2005;(2):CD002273.
6. Schulzke SM, Rao S, Patole SK. A systematic review of cooling for neuroprotection in neonates
with hypoxic ischemic encephalopathy-are we there yet? BMC Paediatr [serial online] 2007 [cited
2009 Apr 6]; 7(30):[10 screens]. Available from:URL:http://www.biomedcentral.com/content/pdf/1471-
2431-7-30.pdf
7. Haddad B, Mercer BM, Livingston JC, Talatti A, Sibai BM. Outcome after successful
resuscitation of babies born with Apgar scores of 0 at both 1 and 5 minutes. Am J Obstet Gynecol
2000; 182:1210-1214.
Refer to online version, destroy printed copies after use Page 18 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
Appendix A: Flowchart for endotracheal suctioning in the presence
of meconium stained liquor
Refer to online version, destroy printed copies after use Page 19 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
Appendix B: Neonatal resuscitation drug guide
These drugs require an order from a Medical Officer/Neonatal Nurse Practitioner prior to
administration.
WEIGHT (kg)
DRUGS
0.5 kg 0.75 kg 1.0 kg 1.5 kg 2.0 kg 2.5 kg 3.0 kg 3.5 kg 4.0 kg
Adrenaline 1:10,000
Route - IV
Dose - 0.01 - 0.03 mg/kg 0.05 mL 0.07 mL 0.1 mL 0.15 mL 0.2 mL 0.25 mL 0.3 mL 0.35 mL 0.4 mL
(0.1 - 0.3 mL/kg) to to to to to to to to to
0.15 mL 0.22 mL 0.3 mL 0.45 mL 0.6 mL 0.75 mL 0.9 mL 1.05 mL 1.2 mL
Admin - rapid bolus
followed by 0.9% sodium
chloride flush
Frequency - repeat every
3 - 5 minutes, if the heart
rate remains less than 60
bpm despite effective PPV
and cardiac compressions
Dilution - not required
Adrenaline 1:10,000
Route - ETT
Dose - 0.03 - 0.1 mg/kg 0.15 mL 0.22 mL 0.3 mL 0.45 mL 0.6 mL 0.75 mL 0.9 mL 1.05 mL 1.2 mL
(0.3 - 1.0 mL/kg) to to to to to to to to to
0.5 mL 0.75 mL 1 mL 1.5 mL 2 mL 2.5 mL 3 mL 3.5mL 4 mL
Admin - inject into ETT,
immediately followed by
PPV
Frequency - repeat every
3 - 5 minutes, if the heart
rate remains less than 60
bpm despite effective PPV
and cardiac compressions
Dilution - not required
Volume Expansion
0.9% Sodium chloride,
(or O Rh – ve blood
only if acute blood loss)
Route - IV
Dose - 10 ml/kg 5 mL 7.5 mL 10 mL 15 mL 20 mL 25 mL 30 mL 35 mL 40 mL
Admin - infusion over
5 -10 minutes
Frequency - may be
repeated if only minimal
improvement
Estimating weight and rounding to the nearest kilogram is appropriate in emergency circumstances.
All drugs administered during the resuscitation must be clearly documented in the newborn infant’s
medical record as per hospital medication administration guidelines.
Refer to online version, destroy printed copies after use Page 20 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
Appendix C: Endotracheal tube size and insertion distance
ETT size (mm Depth of Suction
Weight (g)1 Gestation in inside insertion from catheter size (F)
weeks1 diameter)1 middle of upper for ETT suction
lip in
centimetres
(cm)1
Less than 1000 Less than 28 2.5 6.5 - 7 5 or 6
1000 - 2000 28 – 34 3.0 7-8 6 or 8
2000 – 3000 34 – 38 3.0 - 3.5 8-9 8
Greater than Greater than 38 3.5 - 4.0 Greater than 9 8 or 10
3000
ETT insertion distance, measured from the middle of the upper lip = [weight in kg +6] cm
Refer to online version, destroy printed copies after use Page 21 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
Appendix D: Further notes on the use of a narcotic antagonist
The following is quoted from the Neonatal Resuscitation Textbook 5th Edition 2006, American Heart
Association/American Academy of Paediatrics, Lesson 7, page 10.
“Narcotics given to the labouring mother to relieve pain also may inhibit respiratory drive and activity
in the newborn. In such cases, administration of naloxone (a narcotic antagonist) to the newborn will
reverse the effects of narcotics on the baby.
Giving a narcotic antagonist is not the correct first therapy for a baby who is not breathing. The first
corrective action is positive-pressure ventilation.
The indications for giving naloxone to the baby require both of the following to be present:
• continued respiratory depression after positive pressure ventilation has restored a normal
heart rate and colour and
• a history of maternal narcotic administration within the past 4 hours
After naloxone administration, continue to administer positive pressure ventilation until the baby is
breathing normally. The duration of action of the narcotic often exceeds that of naloxone,
necessitating repeated doses of naloxone. Therefore, observe the baby closely for recurrent
respiratory depression, necessitating repeated doses of naloxone.
Caution: Do not give naloxone to the newborn of a mother who is suspected of being addicted to
narcotics or is on methadone maintenance. This may result in the newborn having seizures.
Other drugs given to the mother, such as magnesium sulphate or non-narcotic analgesics or general
anaesthetics also can depress respirations in the newborn and will not respond to naloxone. If
maternal narcotics were not given to the mother, or if naloxone does not result in restoring
spontaneous respirations, transport the baby to the nursery for further evaluation and management
while continuing to administer positive-pressure ventilation.”
WEIGHT (kg)
DRUG
2.0 kg 2.5 kg 3.0 kg 3.5 kg 4.0 kg
Naloxone hydrochloride 0.4 mg/mL
Route - IV (preferred)
IM acceptable, but delayed onset
of action
Dose - 0.1 mg/kg = 0.25 mL/kg 0.5 mL 0.625 mL 0.75 mL 0.875 mL 1.0 mL
Admin – IV bolus followed by 0.9%
sodium chloride flush
IM - no flush required
Refer to online version, destroy printed copies after use Page 22 of 23
Statewide Maternity and Neonatal Clinical Guideline: Neonatal resuscitation
Appendix E: Acknowledgments
Working Party Clinical Lead
Dr Helen Liley, Neonatologist, Mater Health Services, Brisbane
Working Party Members
Mr Glen Alexander, Nurse Unit Manager, Logan Hospital
Ms Tanya. Beaumont, Midwife, Royal Brisbane and Women’s Hospital
Ms Rosemary Brown, Midwife, Redcliffe Hospital
Dr David Cartwright, Neonatologist, Royal Brisbane and Women’s Hospital
Ms Liz Chappell, Neonatal Clinical Educator, Gold Coast Hospital
Dr Mark Davies, Neonatologist, Royal Brisbane and Women’s Hospital
Dr Luke Jardine, Neonatologist, Royal Brisbane and Women’s Hospital
Dr Guan Koh, Clinical Director Women’s and Children’s Institute, The Townsville Hospital
Ms Sam Lannan, Midwife, Nambour General Hospital
Ms Naida Lumsden, Statewide Maternity and Neonatal Clinical Network Coordinator
Ms Joclyn Neal, Midwifery Educator, Northside Health Service District (Redcliffe/Caboolture)
Ms Maryanne Payne, Neonatal Nurse, The Townsville Hospital
Ms Joy Pitman, Midwife, Biloela Hospital, Biloela
Dr Peter Schmidt, Neonatologist, Gold Coast Hospital
Ms Mary Tredinnick, Pharmacist, Royal Brisbane and Women’s Hospital
Professor David Tudehope, Neonatologist, Mater Health Services, Brisbane
Ms Narelle Walton, Midwife, Logan Hospital
Program Team
Associate Professor Rebecca Kimble, Program Chair, Statewide Maternity and Neonatal Clinical
Guidelines Program
Ms Joan Kennedy, Principal Project Officer, Statewide Maternity and Neonatal Clinical Guidelines
Program
Ms Jacinta Lee, Project Officer, Statewide Maternity and Neonatal Clinical Guidelines Program
Ms Catherine van den Berg, Project Officer, Statewide Maternity and Neonatal Clinical Guidelines
Program
Steering Committee 08_09_10, Statewide Maternity and Neonatal Clinical Guidelines Program
Refer to online version, destroy printed copies after use Page 23 of 23
You might also like
- Neonatal Resuscitation Current IssuesDocument12 pagesNeonatal Resuscitation Current IssuesHuyen LamNo ratings yet
- Advanced Neonatal ResuscitationDocument14 pagesAdvanced Neonatal ResuscitationKrini TandelNo ratings yet
- Advanced Neonatal Resuscitation ProceduresDocument14 pagesAdvanced Neonatal Resuscitation ProceduresSanthosh.S.U100% (1)
- Algoritm: Neonatal Resuscitation: BirthDocument3 pagesAlgoritm: Neonatal Resuscitation: BirthimoyNo ratings yet
- Neonatal Resuscitation Current IssuesDocument11 pagesNeonatal Resuscitation Current Issuesjimmy tNo ratings yet
- Extension of Review Date: Translating Evidence Into Best Clinical PracticeDocument39 pagesExtension of Review Date: Translating Evidence Into Best Clinical PracticeEvan SaapNo ratings yet
- 34 AsfiksiaDocument40 pages34 AsfiksiaDaeng Anggit AdirahmanNo ratings yet
- NRP Reference Chart GuideDocument1 pageNRP Reference Chart GuideWilma Yandan Bau75% (4)
- Clinical PathwayDocument1 pageClinical PathwayMarby MiralNo ratings yet
- NRPDocument8 pagesNRPaeyousefNo ratings yet
- Advanced Neonatal Resuscitation ProceduresDocument14 pagesAdvanced Neonatal Resuscitation ProceduresVijith.V.kumar100% (8)
- Advanced Neonatal ProceduresDocument43 pagesAdvanced Neonatal ProceduresKrupa Jyothirmai100% (1)
- Newborn life support (Antenatal counsellingDocument1 pageNewborn life support (Antenatal counsellingOsman Absher100% (1)
- ITISMITA Biswal MSC, Nursing 2 YearDocument48 pagesITISMITA Biswal MSC, Nursing 2 YearGandimareiNo ratings yet
- 2 Resuscitation of Newborn - Feb 2015Document26 pages2 Resuscitation of Newborn - Feb 2015fnhjfjnfNo ratings yet
- Conen NewborncareDocument35 pagesConen NewborncareRevathi DadamNo ratings yet
- Nursing Care Plan For Ineffective Airway ClearanceDocument3 pagesNursing Care Plan For Ineffective Airway ClearanceRodel Yacas67% (3)
- Pocket Book of Hospital Care For Children - Guidleines For The Management of Common Illnesses With Limited Resources. (2012, World Health Organization)Document442 pagesPocket Book of Hospital Care For Children - Guidleines For The Management of Common Illnesses With Limited Resources. (2012, World Health Organization)Sadia YousafNo ratings yet
- Name: Mr. M AGE: 62 Years Old SEX: Male CC: Persistent Cough Admitting/Working Diagnosis: PnuemoniaDocument3 pagesName: Mr. M AGE: 62 Years Old SEX: Male CC: Persistent Cough Admitting/Working Diagnosis: PnuemoniaMae Therese B. MAGNONo ratings yet
- NeonatalDocument4 pagesNeonatalezzyy whaleNo ratings yet
- Sabal, Pearl Angeli - Ineffective Breathing Pattern (NCP)Document3 pagesSabal, Pearl Angeli - Ineffective Breathing Pattern (NCP)Sam EugenioNo ratings yet
- Newborn Resuscitation GuideDocument40 pagesNewborn Resuscitation GuideAnggun Permata Sari SuknaNo ratings yet
- Helping Baby To BreathDocument49 pagesHelping Baby To BreathmohdmaghyrehNo ratings yet
- Nursing Care Plan for Ineffective Breathing PatternDocument10 pagesNursing Care Plan for Ineffective Breathing PatternAlri LestariNo ratings yet
- Neonatal Resuscitation Seminar1Document120 pagesNeonatal Resuscitation Seminar1G VenkateshNo ratings yet
- Neonatal Resuscitation PDFDocument1 pageNeonatal Resuscitation PDFOdessa EnriquezNo ratings yet
- Neonatal Resuscitation EssentialsDocument22 pagesNeonatal Resuscitation Essentialsshraddha verma100% (1)
- Nursing Care PlanDocument6 pagesNursing Care PlanAnthea ValinoNo ratings yet
- Neonatal Resuscitation (Practical)Document24 pagesNeonatal Resuscitation (Practical)Viraj PawarNo ratings yet
- Clustered Data Nursing Diagnosis (Diagnostic Label) PriorityDocument4 pagesClustered Data Nursing Diagnosis (Diagnostic Label) PriorityRoger ViloNo ratings yet
- NCP PTBDocument4 pagesNCP PTBbryan matiasNo ratings yet
- Neonatal Resuscitation JincyDocument78 pagesNeonatal Resuscitation JincyVivek PrabhakarNo ratings yet
- NlsalgoDocument1 pageNlsalgozacklim_2000No ratings yet
- NRP PPDocument44 pagesNRP PPJl ANo ratings yet
- Newborn Resuscitation StepsDocument9 pagesNewborn Resuscitation StepsAswathy RCNo ratings yet
- DR D R Aryal May, 2014Document109 pagesDR D R Aryal May, 2014kamalshrishNo ratings yet
- Lesson Plan On ResuscitationDocument17 pagesLesson Plan On ResuscitationFarheen khanNo ratings yet
- ResuscitationDocument23 pagesResuscitationMay EvelynNo ratings yet
- NCPDocument3 pagesNCPAmal MUTIANo ratings yet
- For Healthcare Providers Quick Reference: Ard - PushDocument2 pagesFor Healthcare Providers Quick Reference: Ard - Pushزياد داودNo ratings yet
- NCPDocument3 pagesNCPAlexis CoronadoNo ratings yet
- Assessment Nursing Diagnosis Plan of Care Expected Outcome Evaluation Subjective: Independent: Short Term Goal: Goals MetDocument2 pagesAssessment Nursing Diagnosis Plan of Care Expected Outcome Evaluation Subjective: Independent: Short Term Goal: Goals Metapi-3828211No ratings yet
- NLS InfographicsDocument6 pagesNLS InfographicsMihai Ion GhioaldaNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument9 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationthegoodreaderNo ratings yet
- Newborn Life Support for COVID-19 Patients (39Document1 pageNewborn Life Support for COVID-19 Patients (39Hubert AnusNo ratings yet
- NRP - Lesson 7 MedicationsDocument31 pagesNRP - Lesson 7 MedicationsShariti DeviNo ratings yet
- Newborn ResuscitationDocument24 pagesNewborn Resuscitationsagi mu100% (2)
- Lec05 Neonatal Assess ResuscitationDocument16 pagesLec05 Neonatal Assess Resuscitationapi-3709645No ratings yet
- 016-NCP (Pneumonia Rapid Breathing)Document2 pages016-NCP (Pneumonia Rapid Breathing)Venise Angela GarciaNo ratings yet
- 3 PPV PDFDocument28 pages3 PPV PDFBeatrice Joy TombocNo ratings yet
- Nursing Care Plan Newborn Group 2 PlacentaDocument5 pagesNursing Care Plan Newborn Group 2 PlacentaFRANCES DALE ROSALESNo ratings yet
- NCP - MedicinewardDocument3 pagesNCP - MedicinewardErika Mae Deleña MarcoNo ratings yet
- Nursing Care Plan for Activity IntoleranceDocument1 pageNursing Care Plan for Activity IntolerancesonylynneNo ratings yet
- NeonatalresuscitationDocument67 pagesNeonatalresuscitationfidaNo ratings yet
- Neonatal ResuscitationDocument38 pagesNeonatal Resuscitationramanand chaudharyNo ratings yet
- NCM 107 Skills Lab NCPDocument1 pageNCM 107 Skills Lab NCPMoises Clerick BalloguingNo ratings yet
- Pediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesFrom EverandPediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesRating: 5 out of 5 stars5/5 (2)
- Basic Life Support (BLS) Provider HandbookFrom EverandBasic Life Support (BLS) Provider HandbookRating: 5 out of 5 stars5/5 (2)