Professional Documents
Culture Documents
Nursing Care Plan For Hypertension
Uploaded by
Althea ValerianoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan For Hypertension
Uploaded by
Althea ValerianoCopyright:
Available Formats
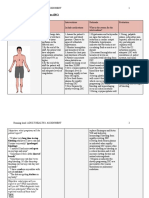
ASSESSMENT Subjective: madalas ako mahilo, as verbalized by the patient.
Objective: >lethargic >decreased cardiac output >decreased stroke volume >increased peripheral vascular resistance >VS taken as follows: T: 37.2 PR: 83 RR: 18 BP: 180/100
DIAGNOSIS Decreased Cardiac Output r/t malignant hypertension as manifested by decreased stroke volume.
PLANNING STG: After 6 hrs of nursing interventions, the client will have no elevation in blood pressure above normal limits and will maintain blood pressure within acceptable limits. LTG: After 5 days of nursing interventions, the client will maintain adequate cardiac output and cardiac index.
INTERVENTION 1.monitor BP every 1-2 hours, or every 5 minutes during actve titration of vasoactive drugs. 2. monitor ECG for dysrrhythmias, conduction defects and for heart rate.
RATIONALE
EVALUATION STG: After 6 hrs of nursing interventions, the client had no elevation in blood pressure above normal limits and will maintain blood pressure within acceptable limits. Goal was met. LTG: After 5 days of nursing interventions, the client maintained an adequate cardiac output and cardiac index. Goal was met.
1. changes in BP may indicates changes in patient status requiring prompt attention. 2. decrease in cardiac output may result in changes in cardiac perfusion causing dysrhythmias. 3. suggest frequent 3. it may decreases position changes. peripheral venous pooling that may be potentiated by vasodilators and prolonged sitting or standing. 4.encourage patient 4. caffeine is a to decrease intake of cardiac stimulant caffeine, cola and and may adversely chocolates. affect cardiac function. 5. observe skin 5. peripheral color, temperature, vasoconstriction capillary refill time may result in pale, and diaphoresis. cool, clammy skin, with prolonged capillary refill time
6.auscultate heart tones.
7. administer medicines as prescribed by the physician. 8. instruct client & family on fluid and diet requirements and restrictions of sodium.
due to cardiac dysfunction and decreased cardiac output. 6. hypertensive patients often have S4 gallops caused by atrial hypertrophy. 7. to promote wellness.
8. restrictions can assist with decrease in fluid retention and hypertension, thereby improving cardiac output. 9. instruct client and 9. promotes family on knowledge and medications, side compliance with effects, drug regimen. contraindications and signs to report.
ASSESSMENT Subjective: Laging sumasakit ang aking ulo at parang nanlalabo ang aking paningin, as verbalized by the patient. Objective: Tachycardia Shortness of breath >rales Restlessness Cool, clammy skin Optic disc papilledema Increased blood pressure.
DIAGNOSIS Ineffective Tissue Perfusion: Cardiopulmonary, Gastrointestinal and Peripheral r/t hypertension and decreased cardiac output as manifested by blurred vision and increased blood pressure..
PLANNING STG: After 8 hrs of nursing interventions, blood pressure will be within set parameters for the client. LTG: After 6 days of nursing interventions, the client will have an adequate tissue perfusion to his body systems.
INTERVENTION 1. monitor VS at least q 1-2 hrs and prn.. 2. encourage patient to decrease intake of caffeine, cola and chocolates. .3. administer vasoactive drugs and titrate as ordered to maintain pressures at set parameters for patient. 4. observe for complaints of blurred vision, tinnitus or confusion. 5. monitor I&O status.
RATIONALE 1.to monitor baseline data. 2. caffeine is a cardiac stimulant and may adversely affect cardiac function. 3. these frugs have rapid action and may decrease the blood pressure too rapidly, resulting in complications. 4. may indicate cyanide toxicity from increasing intracranial pressure. 5. I&O will give an indication of fluic balance or imbalance, thus allowing for changes in treatment regimen when required.
EVALUATION STG: After 8 hrs of nursing interventions, blood pressure maintained within set parameters for the client. Goal was met. LTG: After 6 days of nursing interventions, the client had an adequate tissue perfusion to his body systems. Goal was met.
6. monitor for sudden onset of chest pain. 7. monitor ECG for changes in rate, rhythm, dysrhythmias and conduction defects. 8. observe extremities for swelling, erythema, tenderness and pain. Observe for decreased peripheral pulses, pallor, coldness and cyanosis.
6. may indicate dissecting aortic aneurysm. 7. decreased perfusion may result in dysrhythmias caused by decrease in oxygen. 8.Bedrest promotes venous statis which can increase the risk of thromboembolus formation. If treatment is too rapid and aggressive in decreasing the blood pressire, tissue perfusion will be impaired and ischemia can result. 9. promotes knowledge and compliance with treatment. Promotes prompt detection and facilitates prompt intervention.
9. instruct client in signs/symptoms to report to physician such as headache upon rising, increased blood pressure, chest pain, shortness of breath, increased heart rate,
visual changes, edema, muscle cramps and nausea and vomiting.
You might also like
- Patient Centered Pharmacology Tindall William N Sedrak Mona M Boltri John M SRG PDFDocument575 pagesPatient Centered Pharmacology Tindall William N Sedrak Mona M Boltri John M SRG PDFTedpwer100% (3)
- Psych Nursing Complete Edited Royal PentagonDocument32 pagesPsych Nursing Complete Edited Royal PentagonRichard Ines Valino100% (68)
- Stroke RehabilitationDocument43 pagesStroke RehabilitationHashini Vjkmr100% (4)
- Nanda NCP BasedDocument14 pagesNanda NCP Baseddeliejoyce100% (1)
- Hypertension NCPDocument4 pagesHypertension NCPChristian Karl B. Llanes0% (2)
- Decreased Cardiac Output Related To Decreased Myocardial Contractility Secondary To CardiomyopathyDocument2 pagesDecreased Cardiac Output Related To Decreased Myocardial Contractility Secondary To Cardiomyopathywen_pil75% (8)
- Nuirsing Care Plan For HypertensionDocument8 pagesNuirsing Care Plan For HypertensionJowzef92% (24)
- Nursing Care Plan For HemodialysisDocument2 pagesNursing Care Plan For Hemodialysisderic80% (20)
- Nursing Care Plan For Myocardial InfarctionDocument7 pagesNursing Care Plan For Myocardial Infarctionmariejo95% (125)
- Nursing Care Plan For HypertensionDocument3 pagesNursing Care Plan For HypertensionFranco Razon100% (2)
- NCP HypertensionDocument2 pagesNCP Hypertensionsinister1781% (27)
- Managing Hypertension and Decreased Cardiac OutputDocument5 pagesManaging Hypertension and Decreased Cardiac Outputanon_9189425950% (2)
- Train Yourself QuestionsDocument74 pagesTrain Yourself QuestionsHosam Gomaa100% (5)
- BHW Report 2014Document34 pagesBHW Report 2014Jeff JanNo ratings yet
- Case Study of HypertensionDocument37 pagesCase Study of HypertensionAngelo Bellon Bautista75% (4)
- Assessment Nursing Diagnosis Analysis Goals and Objectives Nursing Interventions Rationale Evaluation EffectivenessDocument3 pagesAssessment Nursing Diagnosis Analysis Goals and Objectives Nursing Interventions Rationale Evaluation EffectivenessYnah Sayoc75% (4)
- NCP For HypertensionDocument6 pagesNCP For HypertensionJaic Ealston D. Tampus0% (2)
- Nursing Care Plan For HypertensionDocument4 pagesNursing Care Plan For HypertensionKathleen Dimacali100% (2)
- NCP For HypertensionDocument4 pagesNCP For HypertensionCiariz Charisse83% (6)
- Subjective:: Decreased Cardiac Output R/T HypertensionDocument3 pagesSubjective:: Decreased Cardiac Output R/T Hypertensionnurse_yramenaj67% (3)
- Nursing Care Plan HypertensionDocument2 pagesNursing Care Plan Hypertensionderic98% (124)
- Nursing Care Plan. HypertensionDocument2 pagesNursing Care Plan. HypertensionKiara Shanelle Posadas AbrioNo ratings yet
- Decreased Cardiac OutputDocument2 pagesDecreased Cardiac OutputDheza Rodis Santos0% (1)
- Nursing Care pLAN (Hypertension)Document7 pagesNursing Care pLAN (Hypertension)Rosalie Valdez Espiritu100% (3)
- Nursing care plan for hypertension, renal calculi, diabetesDocument3 pagesNursing care plan for hypertension, renal calculi, diabetesGimcy Dela Fuente100% (6)
- Research On Curriculum DevelopmentDocument16 pagesResearch On Curriculum Developmentmariejo100% (8)
- Research On Curriculum DevelopmentDocument16 pagesResearch On Curriculum Developmentmariejo100% (8)
- Nursing Care PlanDocument4 pagesNursing Care Planmanu_gutierrez0891% (11)
- Drugs and Tinnitus - Neil Bauman PHD - April '09Document2 pagesDrugs and Tinnitus - Neil Bauman PHD - April '09DownTheTheRabbitHole108No ratings yet
- Nursing Care Plan For HypertensionDocument2 pagesNursing Care Plan For HypertensionFranco Razon100% (1)
- Biochemical Biomarkers in Alzheimer's DiseaseDocument150 pagesBiochemical Biomarkers in Alzheimer's DiseaseInternational Medical PublisherNo ratings yet
- Nursing Care Plan For Upper Resrpiratory Tract InfectionDocument2 pagesNursing Care Plan For Upper Resrpiratory Tract Infectionmariejo90% (30)
- NCP For HypertensionDocument1 pageNCP For Hypertensionrhizalyn1367% (6)
- NCP #1 Ineffective Cerebral Tissue PerfusionDocument4 pagesNCP #1 Ineffective Cerebral Tissue PerfusionsteffiNo ratings yet
- Front Page of Our ThesisDocument13 pagesFront Page of Our Thesismariejo100% (4)
- Introduction to the History and Development of Medical TechnologyDocument23 pagesIntroduction to the History and Development of Medical TechnologyAnne TGNo ratings yet
- High Blood Pressure (HBP) or Hypertension N C P BY BHERU LALDocument2 pagesHigh Blood Pressure (HBP) or Hypertension N C P BY BHERU LALBheru LalNo ratings yet
- Diabetic Patient with Pre-eclampsiaDocument2 pagesDiabetic Patient with Pre-eclampsiaJen Faye Orpilla100% (9)
- 001 Hilton Dr. Directory 2Document20 pages001 Hilton Dr. Directory 2Muhammad Siraj KhanNo ratings yet
- ANDAYA, Kristine Alexis L. BSN218 Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesANDAYA, Kristine Alexis L. BSN218 Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAlexis TineNo ratings yet
- Hypertension Nursing Care PlanDocument2 pagesHypertension Nursing Care PlanCyrus De Asis92% (13)
- Hypertension NCPDocument1 pageHypertension NCPj4royce100% (1)
- NCP Acute Pain (HTN Crisis)Document3 pagesNCP Acute Pain (HTN Crisis)Jenny AjocNo ratings yet
- Nursing Care Plan For HypertensionDocument5 pagesNursing Care Plan For HypertensionJessy MalloNo ratings yet
- Nursing Care Plan For HypocalcemiaDocument1 pageNursing Care Plan For Hypocalcemiamariejo78% (18)
- Stroke NCPDocument5 pagesStroke NCPChantal Caragan100% (1)
- NCP Hypertension 2Document3 pagesNCP Hypertension 2Roseben Somido50% (2)
- Hypertension Nursing Care PlanDocument3 pagesHypertension Nursing Care Plangeng gengNo ratings yet
- Teaching Plan for Chronic Kidney Disease PatientDocument5 pagesTeaching Plan for Chronic Kidney Disease PatientYhan-yhan Rodriguez Khou100% (1)
- Hypertension Nursing Care PlanDocument1 pageHypertension Nursing Care PlanSheila Mae Cabahug100% (1)
- Nursing Care Plan for Hypertension and Knee PainDocument3 pagesNursing Care Plan for Hypertension and Knee PainEzron Kendrick Duran50% (2)
- Rationale EvaluationDocument1 pageRationale EvaluationAshraf DalumaNo ratings yet
- Assessment Explanation Planning Interventions Rationale Evaluation (AEPPIREDocument11 pagesAssessment Explanation Planning Interventions Rationale Evaluation (AEPPIREGrape JuiceNo ratings yet
- HypertensionDocument2 pagesHypertensionRodel Yacas0% (1)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermDocument5 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermJA BerzabalNo ratings yet
- NCP HypertensionDocument2 pagesNCP HypertensionRea LynNo ratings yet
- Nursing Care Plan for HypertensionDocument2 pagesNursing Care Plan for HypertensionKiara Shanelle Posadas AbrioNo ratings yet
- Nursing Care Plan: SubjectiveDocument6 pagesNursing Care Plan: SubjectiveAlimansor M. DarpingNo ratings yet
- Tams NCP and DrugDocument5 pagesTams NCP and DrugNicholas Xavier VenturaNo ratings yet
- Nursing Care Plan For HypertensionDocument6 pagesNursing Care Plan For HypertensionArian May MarcosNo ratings yet
- NCP PlanningDecreased in Cardiac Output Related To Low Hemoglobin and Hematocrit CountDocument6 pagesNCP PlanningDecreased in Cardiac Output Related To Low Hemoglobin and Hematocrit CountMabelle SorianoNo ratings yet
- Nursing Care Plan for HypotensionDocument2 pagesNursing Care Plan for HypotensionMae Denn LabordoNo ratings yet
- NCPDocument2 pagesNCPJonathan LiscanoNo ratings yet
- Nursing Care Plan for HypotensionDocument2 pagesNursing Care Plan for HypotensiondubsNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanNo ratings yet
- DIC Case StudyDocument3 pagesDIC Case StudyJuliaNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention EvaluationDocument3 pagesAssessment Nursing Diagnosis Planning Intervention EvaluationStefhanie DaloraNo ratings yet
- Jake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersDocument8 pagesJake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersJake Yvan DizonNo ratings yet
- Risk NCP Decreased Cardiac OutputDocument2 pagesRisk NCP Decreased Cardiac OutputMICHELLE FACTONo ratings yet
- NCP ApalisokDocument3 pagesNCP ApalisokApalisok GerardNo ratings yet
- Nursing Care Plan: Assessment Cues Nursing DiagnosisDocument4 pagesNursing Care Plan: Assessment Cues Nursing DiagnosisKristil ChavezNo ratings yet
- September 12, 2020: Gulanick, Meg. "Nursing Care Plans: Nursing Diagnosis and Intervention." Apple BooksDocument9 pagesSeptember 12, 2020: Gulanick, Meg. "Nursing Care Plans: Nursing Diagnosis and Intervention." Apple BooksJane Arian BerzabalNo ratings yet
- Nursing Care Plan No. 1 Assessment Diagnosis Planning Intervention Rationale Evaluation Short Term: Short TermDocument11 pagesNursing Care Plan No. 1 Assessment Diagnosis Planning Intervention Rationale Evaluation Short Term: Short TermYumeko JabamiNo ratings yet
- Assessment Diagnosis Scientific Background Planning Intervention Rationale Evaluation Subjective: Short-Term Goals: Independent: Short-Term GoalsDocument2 pagesAssessment Diagnosis Scientific Background Planning Intervention Rationale Evaluation Subjective: Short-Term Goals: Independent: Short-Term GoalsMelvin D. RamosNo ratings yet
- Nursing Care Plan: Thyroid HormonesDocument3 pagesNursing Care Plan: Thyroid HormonesShenaNo ratings yet
- Republic Act 7305Document28 pagesRepublic Act 7305mariejoNo ratings yet
- ParaphiliasDocument4 pagesParaphiliasmariejoNo ratings yet
- Calcium ImbalanceDocument12 pagesCalcium ImbalancemariejoNo ratings yet
- Histoplasmosis: A Case StudyDocument9 pagesHistoplasmosis: A Case StudyDean ivan ParalesNo ratings yet
- Patient Counseling ServicesDocument15 pagesPatient Counseling ServicesAishiteru Mawarna B LaNo ratings yet
- Ds OresolDocument2 pagesDs OresolShannie PadillaNo ratings yet
- EMS Management of Acute Stroke-Prehospital Triage (Resource Document To NAEMSP Position Statement)Document6 pagesEMS Management of Acute Stroke-Prehospital Triage (Resource Document To NAEMSP Position Statement)Allencia NauweNo ratings yet
- Best Dentists in Delhi. ToDocument9 pagesBest Dentists in Delhi. Torohit22221No ratings yet
- Child Health NSGDocument5 pagesChild Health NSGSaleem ParwazNo ratings yet
- SPINE Minimally Invasive TLIF Vs Open TLIF For Lumbar DDDDocument7 pagesSPINE Minimally Invasive TLIF Vs Open TLIF For Lumbar DDDGarry Kin CamarilloNo ratings yet
- Population Dynamics and Control of ContraceptionDocument16 pagesPopulation Dynamics and Control of Contraceptionjaish8904No ratings yet
- Safety Regulations in CSSDocument4 pagesSafety Regulations in CSSMM Ayehsa Allian SchückNo ratings yet
- Immunology and Hypersensitivity: Central Tolerance, Peripheral Tolerance, Types of Hypersensitivity and Autoimmune DiseasesDocument7 pagesImmunology and Hypersensitivity: Central Tolerance, Peripheral Tolerance, Types of Hypersensitivity and Autoimmune DiseasesLianneRaoNo ratings yet
- 1 PE 067 InfographicDocument1 page1 PE 067 InfographicTomáš KrajíčekNo ratings yet
- Day Surgery Policies&ProceduresDocument32 pagesDay Surgery Policies&Proceduresegyank100% (1)
- Case Management TemplateDocument5 pagesCase Management TemplateEncik AhmadNo ratings yet
- The Significant Association Between Maternity Waiting Homes Utilization and Perinatal Mortality in Africa: Systematic Review and Meta-AnalysisDocument6 pagesThe Significant Association Between Maternity Waiting Homes Utilization and Perinatal Mortality in Africa: Systematic Review and Meta-AnalysisTegenne LegesseNo ratings yet
- Civil Aviation Medical Examination Report: Protected "B" When CompletedDocument3 pagesCivil Aviation Medical Examination Report: Protected "B" When CompletedsupriyaNo ratings yet
- Teori 7 Pilar Dasar IKMDocument41 pagesTeori 7 Pilar Dasar IKMIntan Putri Wirahana ShantyNo ratings yet
- Rabie CateiDocument3 pagesRabie CateiC LNo ratings yet
- Administering Intramuscular Injections To Children - What Does The Evidence Say?Document8 pagesAdministering Intramuscular Injections To Children - What Does The Evidence Say?ZACHARIAH MANKIRNo ratings yet
- 1.structure of The TeethDocument5 pages1.structure of The TeethCălin PavelNo ratings yet
- Acute Headache Guide for Emergency PhysiciansDocument6 pagesAcute Headache Guide for Emergency PhysiciansRoselyn DawongNo ratings yet
- TB Treatment in Liver Disease PatientsDocument2 pagesTB Treatment in Liver Disease Patientsmoipone makakoleNo ratings yet
- Physical Education H.O.P.E 1 Module 6Document17 pagesPhysical Education H.O.P.E 1 Module 6Reynaldo Jr LundagNo ratings yet