Professional Documents
Culture Documents
Geurts 2005 CGP2
Uploaded by
maggie305Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Geurts 2005 CGP2
Uploaded by
maggie305Copyright:
Available Formats
Acta Physiol Scand 2005, 183, 117124
Local cold acclimation of the hand impairs thermal responses of the nger without improving hand neuromuscular function
C. L. M. Geurts,1 G. G. Sleivert2 and S. S. Cheung3
1 2 3 Human Performance Laboratory, Faculty of Kinesiology, University of New Brunswick, Fredericton, NB, Canada PacicSport Canadian Sport Centre Victoria, Victoria, BC, Canada Environmental Ergonomics Laboratory, School of Health and Human Performance, Dalhousie University, Halifax, NS, Canada
Received 25 February 2004, accepted 2 September 2004 Correspondence: G. G. Sleivert PhD, Director of Sport Science and Medicine, PacicSport Canadian Sport Centre Victoria, 100-4636 Elk Lake Dr Victoria, BC V8Z 5M1, Canada.
Abstract Aim: To investigate the effects of cold acclimation on the thermal response and neuromuscular function of the hand. Methods: Ten healthy subjects [three female, seven male, age (mean SD): 27.9 7.9 years] immersed their right hand in 8 C water for 30 min, 5 days a week for 3 weeks. On the rst and the last day, neuromuscular function of the rst dorsal interosseus (FDI) muscle was tested. Results: There was no signicant change in maximal voluntary contraction strength or evoked contractile characteristics of the FDI after cold acclimation. Minimum nger temperature decreased signicantly from 10.6 1.2 to 9.3 0.8 C after 3 weeks (P < 0.01), with most of the decrease occurring after a single exposure. Mean nger temperature dropped signicantly from 14.2 1.9 to 11.7 1.4 C following cold acclimation (P < 0.05), with 90% of this adaptation occurring after 5 days. Onset time of cold-induced vasodilatation increased from 446 171 to 736 384 s (P < 0.05) and the amplitude decreased from 5.3 3.2 to 2.5 2.1 C (P < 0.05). This was signicantly different from the control group, who immersed their right hand on the rst and last days only. Conclusion: These data suggest that cold acclimation does not enhance hand temperature or function but may put the hands at a greater risk of cold injury when exposed to the cold. Keywords cold acclimation, cold-induced vasodilatation, contractile properties, evoked force, hand, skin temperature.
There are occupations in which manual work has to be performed in a cold environment. Examples include sherman (LeBlanc et al. 1960, 1964), power-line workers that must work outside in winter, and frozen-food processing industry workers (Chiang et al. 1990). While performing these manual tasks, it is not always possible to protect the hands sufciently against the cold because bulky gloves impair manual dexterity (Geng et al. 1997). When exposed to acute cold stress, the body responds with a vasoconstriction of the extremities to maintain the temperature in the core. After a prolonged period of vasoconstriction, a paradoxical vasodilatation usually
2005 Scandinavian Physiological Society
occurs. This cold-induced vasodilatation (CIVD) was rst reported by Lewis (1930) and has long been considered a protective mechanism for cold injury of the ngers (Wilson & Goldman 1970). During a CIVD, there is an increase in blood ow to the hand that warms up the ngers. Ducharme et al. (1991) also showed increased blood circulation in the large vessels of the forearm during CIVD, which increased the temperature of the forearm muscles. It is well known that neuromuscular function is dependent on the temperature of the muscle (Ranatunga et al. 1987), therefore if CIVD increases muscle temperature of the 117
Cold acclimation in the hand
C L M Geurts et al.
Acta Physiol Scand 2005, 183, 117124
hand muscles due to an increased blood ow to the extremities, this may have a benecial effect on the neuromuscular function in this region and could conceivably improve manual dexterity (Heus et al. 1995). Repeated exposure to cold stress results in a cold acclimation, described by some as cold adaptation. The literature on cold acclimation is ambiguous regarding the effect of chronic or repeated cold stress on the human body. Studies on people living and working in the cold have shown an increased skin temperature and enhanced blood ow to the extremities while in cold conditions (Miller & Irving 1962, Eagan 1963, LeBlanc et al. 1964, Savourey et al. 1996). Other researchers have shown an enhanced vasoconstriction after cold adaptation, resulting in a decreased skin temperature upon cold exposure (Livingstone 1976, Leftheriotis et al. 1990, Bridgman 1991). There are numerous reasons for this diversity of cold adaptation. The type of cold adaptation is probably dependent upon the various experimental conditions used to develop and test cold adaptation, such as continuous vs. discontinuous exposures, moderate vs. severe cold stress, variations in total exposure time during both adaptation and testing, whole body vs. extremity-only exposure, and air vs. water immersion. The purpose of this study was to investigate the effects of repeated cold-water immersion of the hand on thermoregulation of the hand and on the neuromuscular function of the rst dorsal interosseus (FDI) muscle. In this study, the hand was tested and acclimated in cold water for 30 min to get a complete view on the CIVD response that typically occurs after 10 min of cold stress. Although contact cooling through handling material or tools may impose a greater risk in daily life due to its more intense and rapid cooling effect (Jay & Havenith 2004), acclimation will most likely result from whole hand cooling over a longer period of time. Cold water is the safest and fastest way to cool the periphery without putting the subjects at risk of cold injury. The whole hand was cooled instead of only the nger because in daily life people typically expose their whole hand when working in a cold environment. Because the whole hand was immersed, the cold stress would be larger than with nger-only immersion; therefore, a water temperature of 8 C was chosen to minimize the extreme discomfort and nausea often experienced by subjects. It was hypothesized that repeated cold-water immersion of the hand would enhance the CIVD response and that this would improve neuromuscular function of the FDI muscle.
University of New Brunswick approved the study protocol in advance. Each subject completed and answered no to all questions on the Physical Activity Readiness Questionnaire (PAR-Q) (CSEP 1998) and provided written informed consent before participating. Seventeen subjects (10 male, seven female, 26.9 6.6 years) were used for the analysis. One female subject withdrew because of intolerance of the cold water. The data of two male subjects were discarded because they did not show a CIVD response during the initial test, dened as an increase in nger temperature of 0.5 C.
Experimental design
All subjects underwent in total four neuromuscular function tests. The rst two were conducted in thermoneutral condition and after 30 min hand cooling and this was repeated 3 weeks later. The subjects were assigned to two groups a priori to avoid time gaps between the initial test and the acclimation trials. The experimental group (EXP; three female, seven male; age 27.9 7.9 years; height 1.76 0.07 m; weight 74.3 10.4 kg) came into the laboratory ve times a week for 3 weeks to immerse their right hand up to the styloid process into 8 C water for 30 min. On the rst and the last day of this cold acclimation period, they underwent a neuromuscular function test. A control group (CON; four female, three male; age of 25.6 4.1 years; height 1.74 0.08 m; weight 70.2 11.4 kg) arrived at the laboratory on the rst and last day only to undergo the neuromuscular function test. The testing took place in September and October 2002 in eastern Canada (average ambient outdoor temperature: 11.8 5.7 C).
Neuromuscular function test
Upon arrival on the rst and the last day of the cold acclimation period, a plastic mould was made for the index nger and forearm. Two insulated ceramic chip thermistors (MA-100; Thermometrics, New York, NY, USA) were placed next to the nail bed of the right index nger (Tif) and on the skin over the FDI muscle (Tfdi). Skin temperature of the index nger was measured and logged every 8 s on a data logger (Smartreader 8 Plus; ACR, Vancouver, BC, Canada) interfaced with a computer to prevent cold injury. Two stimulating electrodes were placed on the ulnar nerve, 4 and 7 cm proximal to the pisiform bone, respectively. The subject was seated with the shoulder abducted and the forearm resting on a stable base. Forearm and hand were immobilized using a plastic mould and straps. The subject was accustomed to the electric current and familiarized to the feeling of tetanic stimulation. The
2005 Scandinavian Physiological Society
Materials and methods Subjects
Twenty volunteers (12 male and eight female) participated in this study. The Ethics Committee of the 118
Acta Physiol Scand 2005, 183, 117124
C L M Geurts et al.
Cold acclimation in the hand
current was delivered through supramaximal square wave pulses of 200 ls duration by a constant current stimulator (Digitimer; DS7A, Hertfordshire, UK). The protocol used was similar to that of Geurts et al. (2004) and was conducted as follows: rst, the subject performed an isometric maximal voluntary contraction (MVC) with the index nger. The resulting abduction force was amplied (100) and collected at 1 kHz for 1 later processing (WinDaq Pro+; Dataq, Akron, OH, USA). Thereafter, one evoked twitch, evoked tetanic contractions at 10 and 20 Hz stimulating frequencies, and two voluntary force control trials at 25 and 50% of the MVC, 40 s in duration, were performed. Two minutes of rest separated each neuromuscular test. The plastic mould and stimulating electrodes were removed and the subject was then transferred to the hand cooling station. The right hand was immersed up to the styloid processes for 30 min in circulating 8 C water maintained with a chiller (Polyscience, Niles, IL, USA). After 30 min, the hand was removed from the water, dried off, and the subject was transferred back to the myograph and the neuromuscular testing, with exception of the MVC, was repeated. This process took about 35 min; in this time, the index nger warmed up on average 6.2 2.6 C and the skin above the FDI by 6.1 2.4 C.
For the temperature data, a two-sample t-test was used to compare the difference between pre- and posttest values across the experimental and control group. The subjects were assigned to the experimental and control group a priori, which resulted in a difference in the pre-test temperature. Therefore, the different scores of the pre- and post-tests were used for analysis. Additional analysis was performed on the acclimation data. A one-way analysis of variance (anova) with repeated measurements (time, four levels) was performed on day 1, 6, 11 and 15. When a main effect was detected, Bonferroni post-hoc tests were applied to determine signicant differences between the days. For the neuromuscular data, a two-way anova (group time) with repeated measures on one factor (time, consisting of four levels: pre-cold, pre-warm, post-cold and post-warm) was used to test for differences in responses between groups and across time. For all statistics, type 1 error was protected at the 5% level. All data are reported as mean SD.
Results Thermoregulatory data
For the EXP group, minimum nger temperature decreased from 10.6 1.2 to 9.3 0.8 C after 3 weeks of cold acclimation. The difference between the pre- and post-test was signicantly different (P < 0.01) from that of the control group (9.2 0.5 C before, 9.3 0.8 C after). The time-course of the minimum temperature response is shown in Figure 1. Time-course analysis showed that the modelled minimum nger temperature was completely adapted after a single exposure. Analysis of variance conrmed a signicant time effect and post-hoc comparisons revealed that the cold acclimation response occurred between days 1 and 6 (P 0.02).
Data analysis
The onset time of the CIVD was dened as the time from hand entry until the skin temperature of the index nger rst started to rise for more than 0.5 C and the amplitude of the CIVD was dened as the apex of the CIVD minus the nadir of the CIVD. The minimum skin temperature of the index nger (Tif min) and the average temperature of the index nger (Tif mean) during the 30 min water immersion were averaged over the 10 experimental subjects and plotted vs. acclimation day and then tted with a simple exponential function [y a + b exp()x/c)] (Gill & Sleivert 2001). The following characteristics were calculated from the evoked force measurements. Peak twitch force (PTF) was dened as the peak amplitude of the force signal. Time to peak force (TTP) was dened as the delay between the stimulus and the peak amplitude. The half relaxation time (1/2RT) was dened as the time between the PTF and the point at which the peak force was reduced to half its size. To determine the degree of fusion in the tetanic forces at 10 and 20 Hz, an epoch of 200 ms was taken at peak force and the coefcient of variation (CV) was calculated by dividing the standard deviation by the mean force of this epoch. The CV of the submaximal voluntary forces were calculated in a similar manner by using an epoch of 1 s after 20 s. High CV represent poorer force control.
2005 Scandinavian Physiological Society
Figure 1 Minimum index nger temperature [mean (SD)] during cold water immersion of the EXP group (open circles) over the course of 15 days, and pre and post values of the CON group (lled circles). *Signicantly different from day 1: P < 0.05 (repeated measures on day 1, 6, 11 and 15).
119
Cold acclimation in the hand
C L M Geurts et al.
Acta Physiol Scand 2005, 183, 117124
The mean nger temperature over the 30-min immersion signicantly dropped from 14.2 1.9 C before to 11.7 1.4 C after cold acclimation (P < 0.05), compared with that of the control group (12.1 1.5 C before, 11.5 1.3 C after). The time-course analysis shown in Figure 2 reveals that after a single exposure, 67% of the acclimation in mean nger temperature had occurred, and 99% of cold acclimation was reached by day 5. Analysis of variance conrmed a signicant time effect and post-hoc comparisons revealed that the cold acclimation response occurred between days 1 and 6 (P < 0.01). The onset time for CIVD increased from 446 172 s before to 736 385 s after acclimation in the EXP group and the difference between pre- and post-test was signicantly different (P < 0.05) from that of the CON group (534 263 s before, 573 247 s after). Timecourse analysis shown in Figure 3 reveals that 92% of the acclimation had occurred by day 5. The amplitude of CIVD decreased from 5.3 3.2 C before to 2.5 2.1 C after acclimation, which was signicantly different (P < 0.05) from the control group
(3.0 3.0 C before, 3.0 2.9 C after). The timecourse of the amplitude change is displayed in Figure 4. In addition, the skin temperature of the index nger after 10 min of cold water immersion was signicantly decreased from 12.3 2.2 C before to 10.6 2.0 C after acclimation in the EXP group (P < 0.04) compared with the control group (10.5 1.3 before, 11.6 2.2 C after). An overview of all the temperature data is shown in Table 1. Comparison of the temperature data of EXP and CON group combined for the pre-acclimation test revealed no signicant difference between the male subjects and females subjects for the index nger temperature. Only the onset time of the CIVD was signicantly later in the group of male subjects (P < 0.04). After 30 min of cold water immersion, the hand was quickly placed in the hand myograph and strapped in. As soon as the hand was out of the water, the hand warmed up. Although nger and FDI temperature increased on average 6.2 2.6 and 6.0 2.4 C, respectively, both Tif and Tfdi were signicantly colder during the cold condition compared with the warm condition (P < 0.01). During the neuromuscular testing, the Tfdi in the warm condition was 32.6 2.8 C before and 30.7 2.4 C after cold acclimation. In the cold condition, the Tfdi was 18.8 2.8 C before and 17.6 3.4 C after cold acclimation. The Tif was 30.4 3.9 C before and 27.0 3.7 C after cold acclimation in the warm condition and 19.2 3.2 and 15.7 2.7 C after cold acclimation in the cold condition. These differences were not signicantly different between groups.
Figure 2 Average index nger temperature over 30 min cold water immersion [mean (SD)] of the EXP group (open circles) over the course of 15 days and pre and post values of the CON group (lled circles). *Signicantly different from day 1: P < 0.05 (repeated measures on day 1, 6, 11 and 15).
Neuromuscular data
Maximal voluntary contraction was not signicantly different between groups after acclimation and averaged 54.5 21.8 n before and 59.5 22.0 n after cold for
Figure 3 Onset time for the CIVD [mean (SD)] of the EXP group (open circles) over the course of 15 days of cold acclimation and the pre and post values of the CON group (lled circles). *Signicantly different from day 1: P < 0.05.
Figure 4 Amplitude of the CIVD [mean (SD)] of the EXP group (lled circles) over the course of 15 days, and the pre and post values of the CON group (lled circles). *Signicantly different from day 1: P < 0.05. 2005 Scandinavian Physiological Society
120
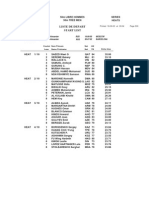
Acta Physiol Scand 2005, 183, 117124 Table 1 Temperature responses before and after cold acclimation and the difference score for the experimental and control group
C L M Geurts et al.
Cold acclimation in the hand
Post Difference (pre ) post) 3.4 3.0 0.8 0.8 1.4 1.3 3.2 2.4 384.9 247 2.1 2.9 2.0 2.2 4.5 0.9 1.3 )0.1 2.5 0.6 4.0 0.6 )290 )40 2.8 0.0 1.7 )1.1 4.0 4.5 1.0 0.6* 1.8 1.7* 5.0 2.2* 325 129* 3.6 1.2* 1.9 2.6*
Group Tif at entry (C) Tif Tif Tif
min
Pre 31.9 28.3 10.6 9.2 14.2 12.1 16.5 13.4 446.4 533.7 5.3 3.0 12.3 10.5 3.0 3.2 1.2 0.5 1.9 1.5 3.9 2.9 171.7 263.2 3.2 3.0 2.2 1.2
(C) (C) (C)
mean
max
Onset time (s) Amplitude (C) Tif (after 10 min) (C)
Exp Con Exp Con Exp Con Exp Con Exp Con Exp Con Exp Con
27.4 27.3 9.3 9.3 11.7 11.5 12.5 12.8 736 573.7 2.5 3.0 10.6 11.6
Tif, skin temperature of index nger; Entry, nger temperature before water immersion; Min, minimum temperature during 30-min immersion; Mean, average temperature during 30-min immersion; Max, maximum temperature after the minimum temperature; Onset time, onset time of CIVD. Amplitude is Tif max ) Tif min. *Signicant difference between experimental and control group on difference score (P < 0.05).
the groups combined. An overview of the neuromuscular data is shown in Table 2. There was a signicant difference between the muscle characteristics in the warm and cold conditions, but there were no signicant changes in neuromuscular function of the FDI as a result of cold acclimation. The degree of fusion was higher (as observed by the smaller CV) in the voluntary force control trials than in the evoked tetanic contractions, but there was no effect of either thermal condition or cold acclimation. There was no signicant effect of cold acclimation on any neuromuscular parameters measured in this study.
Discussion
The unique aspect of this study was the time-course data of local acclimation of the hand, coupled with the prolonged immersion time and the neuromuscular tests performed before and after local cold acclimation. We found that immersing one hand repeatedly in cold water resulted in an enhanced vasoconstriction and a blunted CIVD response, with the majority of the acclimation occurring within the rst week of cold water immersion. Most researchers who have reported a decrease in skin temperature after cold acclimatization tested their subjects during whole body cooling in air (Young et al. 1986, Savourey et al. 1996, OBrien et al. 2000) or their subjects underwent a whole body cold exposure during the acclimatization period (Paik et al. 1972, Livingstone 1976, Bridgman 1991, Savourey et al. 1992). However, a lower core body temperature can
2005 Scandinavian Physiological Society
directly impair the CIVD response (Daanen et al. 1997). In this study, the subjects were only subjected to local hand cooling while sitting in a thermoneutral room (ambient temperature 23.0 1.6 C). This is similar to the exposures used in other studies using imposed repeated local cooling of the periphery, but other studies using this exposure regime on their subjects found higher skin temperatures of the hand in the adapted group (Adams & Smith 1962, Eagan 1963). The results in this study were therefore unexpected. An enhanced vasoconstriction resulting in colder hands may be expected to impair neuromuscular function, as temperature is an important modulator of the contractile function of skeletal muscle (Davies & Young 1983, De Ruiter et al. 1999). In the present study, a signicant impairment in contractile characteristics between the warm and cold condition was observed and no benecial adaptations in neuromuscular function were found after cold acclimation. Previous research by Geurts et al. (2004) reported that a decrease in Tfdi of 10.2 C resulted in an increase in TTP and 1/2RT of 58 and 63 ms, respectively. A larger change in temperature response in the hand and nger may be needed to see signicant changes in neuromuscular function after acclimation. During cold water immersion, the nger temperature was signicantly lower after cold acclimation. The skin temperature above the FDI was, however, less affected and this decrease was not signicantly different between groups. The skin temperature directly above the FDI is closely related to the muscle temperature of the FDI 121
Cold acclimation in the hand
C L M Geurts et al.
Cold Post 20.5 23.5 1.3 1.2 19 12 18 13 5.3 4.8 1.0 1.3 9.4 14.9 0.9 0.5 1.0 0.9 1.2 2.0 61.2 58.3 2.5 1.8 145 138 72 63 11.7 8.6 2.5 4.6 30.8 27.1 1.2 1.1 1.8 3.5 4.2 3.5 16.4 27.7 0.8 0.8 14 17 20 15 10.0 7.4 1.0 3.5 10.8 13.7 0.6 0.6 1.3 2.4 7.7 3.2 Pre 2.0 1.6 231 223 173 179 20.5 15.9 1.4 2.0 33.7 27.7 1.1 1.0 1.8 2.6 2.7 2.8 1.2 1.5 27 31 46 56 7.6 11.5 0.6 1.0 10.1 16.0 0.7 0.7 1.8 2.5 1.7 1.6 Post 1.2 0.8 268 269 174 162 15.5 11.1 1.6 2.3 24.8 21.1 1.0 1.2 1.5 2.2 2.2 2.2 1.2 0.3 48 103 55 5.2 8.6 4.6 0.7 0.9 7.2 6.2 0.6 0.7 0.5 1.5 1.1 1.2
Acta Physiol Scand 2005, 183, 117124 Table 2 An overview of the neuromuscular data (mean SD) from the warm (31.6 2.7 C) and cold test (18.2 3.1 C) for the experimental and control group
Warm Group MVC (n) PTF (n) TTP (ms) 1/2RT (ms) Fmax 10 Hz (n) CV 10 Hz (%) Fmax 20 Hz (n) CV 20 Hz (%) CV25%MVC (10)2 %) CV50%MVC (10)2 %) Exp Con Exp Con Exp Con Exp Con Exp Con Exp Con Exp Con Exp Con Exp Con Exp Con Pre 55.1 54.3 2.8 2.3 142 136 78 69 10.9 9.6 2.6 1.9 32.3 30.0 1.6 1.0 1.7 2.2 1.8 2.7
MVC, maximal voluntary contraction; PFT, peak twitch force; TTP, time to peak force; 1/2RT, half relaxation time; Fmax 10 Hz, maximum force at 10 Hz stimulating frequency; CV 10 Hz, SD/mean of 200 ms epoch of force response at 10 Hz; Fmax 20 Hz, maximum force at 20 Hz stimulating frequency; CV 20 Hz, SD/mean of 200 ms epoch of force response at 20 Hz.
(Ranatunga et al. 1987). To our knowledge it is not known if this relationship would change with repeated cold water immersion of the hand. It is possible that cold acclimation results in a more severe cutaneous vasoconstriction (Paik et al. 1972), causing the skin to act more as an insulating layer over the FDI muscle. As the skin above the FDI muscle is thin, we think this effect, if present, will be negligible, and that the skin temperature can be used as an indication of the muscle temperature. Cold acclimation did not affect FDI temperature and therefore it is not surprising that cold acclimation did not affect neuromuscular function. This also suggests that focusing on changes in nger thermal responses may not be appropriate when investigating manual dexterity or neuromuscular function of the hand as a whole during cold exposure. The longer cold exposure duration in the present study than in typical studies on hand immersion, in combination with whole-hand vs. single nger immersion, may have had an effect on the study outcome. The majority of studies on peripheral cold adaptation immersed hands for a relatively brief period of 515 min (LeBlanc et al. 1960, Adams & Smith 1962, Nelms & Soper 1962, Eagan 1963, Savourey et al. 1996), in contrast to the 30 min exposure utilized in the present study. Upon closer examination of the values of 122
Tif min after 10 min and Tif min, it was found that there was a signicant decrease in skin temperature in the nal 20 min of exposure. It is possible that the extended duration of cold exposure in the present protocol precipitated the insulative adaptation that was observed, and in the other studies the duration of exposure was insufcient to fully maximize the vasoconstrictive response. Contact cooling can be expected to play a role in the cooling of the hand when working in a cold environment. Depending on the materials handled and contact force, contact cooling is a more rapid and local cooling than whole hand cooling (Jay & Havenith 2004). It may be expected that in contact cooling only the local skin will be cooled (Chen et al. 1996) and that the muscles, mostly located on the dorsum of the hand will be less affected. The local skin temperature in this case will determine the contact time, and thus cooling, in such situations. Another interesting nding of the present study was that the time-course analysis showed that the modelled minimal nger temperature during the 30 min immersion decreased after only one single exposure. Cold acclimation outside the laboratory was not expected as the testing was conducted in September and October with outside temperatures of 1018 C. Vasoconstriction can be inuenced by mental stress (Halperin et al.
2005 Scandinavian Physiological Society
Acta Physiol Scand 2005, 183, 117124
C L M Geurts et al.
Cold acclimation in the hand
1983) as well as physical stress (Adams & Smith 1962). Noradrenaline release is increased during psychological stress and enhances vasoconstriction. It is possible that the cold stress experienced in the rst day caused an additional mental stress on the second day resulting in an enhanced vasoconstriction. Anticipation of the cold water may have caused the small change in temperature response observed in the control group, resulting in a small decrease in mean Tif and amplitude as well as a slight delay in onset of the CIVD. These changes were substantially smaller than those observed in the experimental group, and we would not expect the mental stress of cold exposure to endure with the repeated cold immersions experienced in the experimental group. There was an uneven distribution of males and females in the experimental and control group and this may have caused differences between the two groups in the pre-acclimation tests. Bartelink et al. (1993) found lower index nger temperatures for females compared with males and an enhanced vascular reactivity in women, resulting in enhanced vasoconstriction and thus lower temperatures. Female core temperature uctuates within the menstrual cycle with the highest core temperatures during the luteal phase, with a difference up to 0.59 C (Hessemer & Bruck 1985) when tested at 03:00 h at the middle of the luteal phase. Jay & 2 Havenith (2004) found that hand/nger size had a greater predictive power than sex. However, we did not nd a signicant difference in index nger temperatures in the initial test between the male and female subjects in this study. Only the onset time of the CIVD was signicantly later in males compared with the females. It has been previously reported that thermal sensation is rapidly habituated with cold exposure (Leppaluoto et al. 2001). In addition, pain sensation is less in coldadapted individuals (Budd et al. 1993). This was also reported in the older literature on Inuits (Brown & Page 1952), shers (LeBlanc et al. 1960) and sh lleters (Nelms & Soper 1962). Unfortunately, thermal sensation was not measured in this study; however, subjective complaints indicated that the subjects did experience less pain and cold at the end of the acclimation period. Sawada et al. (2000) concluded that subjective judgements may not be reliable indicators for monitoring the risk of progressive tissue cooling and frostbite formation. If the ngers are getting colder after cold acclimation but the subjects experience less pain or feel less cold, cold acclimation could potentially put someone at greater risk of cold injury. In summary, unlike the majority of prior research, repeated and prolonged cold water immersion of the hand with the present protocol resulted in an attenuated CIVD response of the ngers but no adaptive responses in FDI temperature or neuromuscular function. The rapid reduction in CIVD, after only a single cold
2005 Scandinavian Physiological Society
exposure of the hands, could potentiate the risk of cold injury during subsequent cold exposure.
We would like to thank the subjects for their enthusiastic participation. The study was supported by a Discovery Grant (Cheung and Sleivert) from the Natural Sciences and Engineering Research Council of Canada (NSERC). C. Geurts was supported by a NSERC PGS-B Scholarship.
References
Adams, T. & Smith, R.E. 1962. Effect of chronic local cold exposure on nger temperature responses. J Appl Physiol 17, 317322. Bartelink, M.L., De Wit, A., Wollersheim, H., Theeuwes, A. & Thein, T. 1993. Skin vascular reactivity in healthy subjects: inuence of hormonal status. J Appl Physiol 72, 727732. Bridgman, S.A. 1991. Peripheral cold acclimatization in Antarctic scuba divers. Aviat Space Environ Med 62, 733738. Brown, G.M. & Page, J. 1952. The effect of chronic exposure to cold on temperature and blood ow of the hand. J Appl Physiol 5, 221227. Budd, G.M., Brotherhood, J.R., Beasley, F.A. et al. 1993. Effects of acclimatization to cold baths on mens responses to whole-body cooling in air. Eur J Appl Physiol Occup Physiol 67, 438449. Chen, F., Liu, Z.Y. & Holmer, I. 1996. Hand and nger skin temperatures in convective and contact cold exposure. Eur J Appl Physiol Occup Physiol 72, 372379. Chiang, H.C., Chen, S.S., Yu, H.S. & Ko, Y.C. 1990. The occurrence of carpal tunnel syndrome in frozen food factory employees. Kaohsiung J Med Sci 6, 7380. CSEP 1998. Canadian Physical Activity Fitness and Lifestyle Appraisal. Canadian Society for Exercise Physiology, 3 Ottawa, Canada. Daanen, H.A., Van de Linde, F.J., Romet, T.T. & Ducharme, M.B. 1997. The effect of body temperature on the hunting response of the middle nger skin temperature. Eur J Appl Physiol Occup Physiol 76, 538543. Davies, C.T. & Young, K. 1983. Effect of temperature on the contractile properties and muscle power of triceps surae in humans. J Appl Physiol 55, 191195. De Ruiter, C.J., Jones, D.A., Sargeant, A.J. & De Haan, A. 1999. Temperature effect on the rates of isometric force development and relaxation in the fresh and fatigued human adductor pollicis muscle. Exp Physiol 84, 11371150. Ducharme, M.B., VanHelder, W.P. & Radomski, M.W. 1991. Cyclic intramuscular temperature uctuations in the human forearm during cold-water immersion. Eur J Appl Physiol Occup Physiol 63, 188193. Eagan, C.J. 1963. Local vascular adaptations to cold in man. Fed Proc 22, 947952. Geng, Q., Chen, F. & Holmer, I. 1997. The Effect of Protective Gloves on Manual Dexterity in the Cold Environments. Int J Occup Safety Ergon 3, 1529. Geurts, C., Sleivert, G.G. & Cheung, S.S. 2004. Temperature effects on the contractile characteristics and sub-maximal voluntary isometric force production of the rst dorsal interosseus muscle. Eur J Appl Physiol 91, 4145.
123
Cold acclimation in the hand
C L M Geurts et al.
Acta Physiol Scand 2005, 183, 117124 Miller, L.K. & Irving, L. 1962. Local reactions to air cooling in an Eskimo population. J Appl Physiol 17, 449455. Nelms, J.D. & Soper, D.J.G. 1962. Cold vasodilatation and cold acclimatization in the hands of British sh lleters. J Appl Physiol 17, 444448. OBrien, C., Young, A.J., Lee, D.T., Shitzer, A., Sawka, M.N. & Pandolf, K.B. 2000. Role of core temperature as a stimulus for cold acclimation during repeated immersion in 20 degrees C water. J Appl Physiol 89, 242250. Paik, K.S., Kang, B.S., Han, D.S., Rennie, D.W. & Hong, S.K. 1972. Vascular responses of Korean Ama to hand immersion in cold water. J Appl Physiol 32, 446450. Ranatunga, K.W., Sharpe, B. & Turnbull, B. 1987. Contractions of a human skeletal muscle at different temperatures. J Physiol 390, 383395. Savourey, G., Vallerand, A.L. & Bittel, J.H. 1992. General and local cold adaptation after a ski journey in a severe arctic environment. Eur J Appl Physiol Occup Physiol 64, 99105. Savourey, G., Barnavol, B., Caravel, J.P., Feuerstein, C. & Bittel, J.H. 1996. Hypothermic general cold adaptation induced by local cold acclimation. Eur J Appl Physiol Occup Physiol 73, 237244. Sawada, S., Araki, S. & Yokoyama, K. 2000. Changes in coldinduced vasodilatation, pain and cold sensation in ngers caused by repeated nger cooling in a cool environment. Ind Health 38, 7986. Wilson, O. & Goldman, R.F. 1970. Role of air temperature and wind in the time necessary for a nger to freeze. J Appl Physiol 29, 658664. Young, A.J., Muza, S.R., Sawka, M.N., Gonzalez, R.R. & Pandolf, K.B. 1986. Human thermoregulatory responses to cold air are altered by repeated cold water immersion. J Appl Physiol 60, 15421548.
Gill, N. & Sleivert, G. 2001. Effect of daily versus intermittent exposure on heat acclimation. Aviat Space Environ Med 72, 385390. Halperin, J.L., Cohen, R.A. & Coffman, J.D. 1983. Digital vasodilatation during mental stress in patients with Raynauds disease. Cardiovasc Res 17, 671677. Hessemer, V. & Bruck, K. 1985. Inuence of menstrual cycle on shivering, skin blood ow, and sweating responses measured at night. J Appl Physiol, 59, 19021910. Heus, R., Daanen, H.A. & Havenith, G. 1995. Physiological criteria for functioning of hands in the cold. Appl Ergon 26, 513. Jay, O. & Havenith, G. 2004. Finger skin cooling on contact with cold materials: a comparison between male and female responses during short-term exposures. Eur J Appl Physiol 91, 373381. LeBlanc, J., Hildes, J.A. & Heroux, O. 1960. Tolerance of Gaspe shermen to cold water. J Appl Physiol 15, 1031 1034. LeBlanc, J., Pouliot, M. & Rheaume, S. 1964. Thermal balance and biogenic amine excretion in Gaspe shermen exposed to cold. J Appl Physiol 19, 912. Leftheriotis, G., Savourey, G., Saumet, J.L. & Bittel, J. 1990. Finger and forearm vasodilatatory changes after local cold acclimation. Eur J Appl Physiol Occup Physiol 60, 4953. Leppaluoto, J., Korhonen, I. & Hassi, J. 2001. Habituation of thermal sensations, skin temperatures, and norepinephrine in men exposed to cold air. J Appl Physiol 90, 12111218. Lewis, T. 1930. Observations upon the reactions of the vessels of the human skin to cold. Heart 15, 177208. Livingstone, S.D. 1976. Changes in cold-induced vasodilation during Arctic exercises. J Appl Physiol 40, 455457.
124
2005 Scandinavian Physiological Society
You might also like
- Japplphysiol 00859 2004Document7 pagesJapplphysiol 00859 2004muntasir antuNo ratings yet
- Immune Effects of Cold ExposureDocument12 pagesImmune Effects of Cold ExposurePAPA HURCONo ratings yet
- Exercise&HeatDocument27 pagesExercise&HeatAlexander ElkoninNo ratings yet
- Coombs Et Al 2021 Distinct Contributions of Skin and Core Temperatures To Flow Mediated Dilation of The Brachial ArteryDocument11 pagesCoombs Et Al 2021 Distinct Contributions of Skin and Core Temperatures To Flow Mediated Dilation of The Brachial Arteryhassenesalam18No ratings yet
- E Vect of Body Temperature On Cold Induced VasodilationDocument9 pagesE Vect of Body Temperature On Cold Induced Vasodilationmuntasir antuNo ratings yet
- Watkins 2018Document8 pagesWatkins 2018rulas workNo ratings yet
- 2001 Ice Therapy How Good Is The EvidenceDocument6 pages2001 Ice Therapy How Good Is The EvidenceFrancisco Antonó Castro WeithNo ratings yet
- Resistance Index of Frostbite As A Predictor of Cold Injury in Arctic OperationsDocument4 pagesResistance Index of Frostbite As A Predictor of Cold Injury in Arctic OperationsFenni OktoberryNo ratings yet
- 1 s2.0 S0169814119306043 MainDocument8 pages1 s2.0 S0169814119306043 Main30 secondsNo ratings yet
- Cleveland Clinic Quarterly-1985-Ciolek-193-201 PDFDocument9 pagesCleveland Clinic Quarterly-1985-Ciolek-193-201 PDFCésar Morales GarcíaNo ratings yet
- Physical Agent Modalities in PTDocument16 pagesPhysical Agent Modalities in PTlauris881106No ratings yet
- Rapid warming of cold probe upon oral contact measuredDocument5 pagesRapid warming of cold probe upon oral contact measuredAldo Hip NaranjoNo ratings yet
- Effects of A Circulating-Water Garment and Forced-Air Warming On Body Heat Content and Core TemperatureDocument7 pagesEffects of A Circulating-Water Garment and Forced-Air Warming On Body Heat Content and Core Temperaturemuntasir antuNo ratings yet
- AnthDocument8 pagesAnthapi-302701702No ratings yet
- Trashed-0000318Document5 pagesTrashed-0000318Manish GhimireNo ratings yet
- Bicycle Ergometer Warms Hands for Nerve TestsDocument3 pagesBicycle Ergometer Warms Hands for Nerve Testseka nurjanahNo ratings yet
- Ice Therapy: How Good Is The Evidence?: Orthopedics and Clinical ScienceDocument6 pagesIce Therapy: How Good Is The Evidence?: Orthopedics and Clinical ScienceEva FisioNo ratings yet
- Motor and Sensory Nerve ConductionDocument12 pagesMotor and Sensory Nerve ConductionSantiago Mondragon RiosNo ratings yet
- Cold Water Immersion: A Review of The Literature For Winter SwimmingDocument8 pagesCold Water Immersion: A Review of The Literature For Winter SwimmingUrs MüllerNo ratings yet
- Influence of and Humidity The Obstruction By: Airway Induced Exercise AsthmaDocument8 pagesInfluence of and Humidity The Obstruction By: Airway Induced Exercise AsthmaiulyyNo ratings yet
- Hydro CardiovasDocument39 pagesHydro CardiovasFransiskus Xaverius CungkringNo ratings yet
- Effects of Cryotherapy On Lower Leg Deep TissueDocument10 pagesEffects of Cryotherapy On Lower Leg Deep TissueQuiroprácticaParaTodosNo ratings yet
- Scientific Justification of Cryonics Practice: Rejuvenation Research May 2008Document19 pagesScientific Justification of Cryonics Practice: Rejuvenation Research May 2008Ike Jayson ROLLONNo ratings yet
- Blood Pressure Response To Cold Water Immersion TestDocument9 pagesBlood Pressure Response To Cold Water Immersion TestholdonpainendsNo ratings yet
- Thermal Behavior Differs Between Males and Females.18Document12 pagesThermal Behavior Differs Between Males and Females.18GerasimarasNo ratings yet
- Physiological Tolerance To Uncompensable Heat Stress: Effects of Exercise Intensity, Protective Clothing, and ClimateDocument7 pagesPhysiological Tolerance To Uncompensable Heat Stress: Effects of Exercise Intensity, Protective Clothing, and ClimateAnonymous lPY9viIB5No ratings yet
- Magnetic RefrigerationDocument7 pagesMagnetic RefrigerationhasanNo ratings yet
- Sweat 780Document11 pagesSweat 780ecofriend341445No ratings yet
- The Effect of Direct and Indirect Hand Heating On Finger Blood Flow and Dexterity During Cold ExposureDocument6 pagesThe Effect of Direct and Indirect Hand Heating On Finger Blood Flow and Dexterity During Cold ExposureDaenaCharlesNo ratings yet
- Does The Hair Influence Heat Extraction From The Head During Head Cooling Under Heat Stress?Document9 pagesDoes The Hair Influence Heat Extraction From The Head During Head Cooling Under Heat Stress?ytithiNo ratings yet
- 2Document82 pages2qaisersiddiNo ratings yet
- Kim 2020Document4 pagesKim 2020Ester DuwitNo ratings yet
- Hypothermia's central and peripheral effects on elbow flexor performanceDocument11 pagesHypothermia's central and peripheral effects on elbow flexor performanceCristopher Castro RdNo ratings yet
- Cold Pressure Test PDFDocument4 pagesCold Pressure Test PDFAdel LiaNo ratings yet
- The Effect of Temperature On Manual Dexterity, Reaction Time, and Optimum Grip-SpanDocument5 pagesThe Effect of Temperature On Manual Dexterity, Reaction Time, and Optimum Grip-SpanMladen PuljićNo ratings yet
- Sex Difference in Cold Perception and Shivering Onset Upon Gradual Cold ExposureDocument9 pagesSex Difference in Cold Perception and Shivering Onset Upon Gradual Cold ExposureAzizi AlfyanNo ratings yet
- Ice TowelDocument4 pagesIce TowelAyu sulistiani dianingtyasNo ratings yet
- CryotherapyIce PacksDocument12 pagesCryotherapyIce PacksMurad KurdiNo ratings yet
- A Thermoregulation Model To Detect Diabetic Peripheral NeuropathyDocument4 pagesA Thermoregulation Model To Detect Diabetic Peripheral NeuropathyDilip KenNo ratings yet
- The Effects of Indoor Versus Outdoor Thermal Biofeedback Training in Cold Weather SportsDocument7 pagesThe Effects of Indoor Versus Outdoor Thermal Biofeedback Training in Cold Weather Sportswan nazrolNo ratings yet
- The Temperature-Dependent Viscoelasticity of Porcine Lumbar Spine LigamentsDocument7 pagesThe Temperature-Dependent Viscoelasticity of Porcine Lumbar Spine LigamentshjakamjNo ratings yet
- Hot and Cold Modalities EffectsDocument2 pagesHot and Cold Modalities EffectsYumi KaitoNo ratings yet
- 2007021394Document17 pages2007021394ramy86No ratings yet
- Efficacy of Keishibukuryogan A Traditional JapanesDocument6 pagesEfficacy of Keishibukuryogan A Traditional JapanesKhánh NguyễnNo ratings yet
- The Application of Thermal Image Analysis To Diabetic Foot DiagnosisDocument7 pagesThe Application of Thermal Image Analysis To Diabetic Foot DiagnosisDilip KenNo ratings yet
- Jurnal Terapi Rendam Kaki PDFDocument7 pagesJurnal Terapi Rendam Kaki PDFFIRMAN SYAH PERMADINo ratings yet
- Physiological Responses and Performance During Cold Storage WorkDocument8 pagesPhysiological Responses and Performance During Cold Storage WorkAmeer HamzaNo ratings yet
- Hot Skin and Hypohydration Limit Aerobic PerformanceDocument6 pagesHot Skin and Hypohydration Limit Aerobic PerformanceSaifuddin HaswareNo ratings yet
- Hunting Reaction - WikipediaDocument6 pagesHunting Reaction - WikipediaMashal GulNo ratings yet
- Physiological Consequences of Intermittent Exercise During Compensable and Uncompensable Heat StressDocument8 pagesPhysiological Consequences of Intermittent Exercise During Compensable and Uncompensable Heat Stresscraig1014No ratings yet
- HPA Axis Activation by A Socially Evaluated Cold-Pressor TestDocument6 pagesHPA Axis Activation by A Socially Evaluated Cold-Pressor TestKlaudijus VitkauskasNo ratings yet
- Cabana C 1992Document2 pagesCabana C 1992Armando Jose Yáñez SolerNo ratings yet
- Thermoregulation During Exercise inDocument15 pagesThermoregulation During Exercise inRicardo LeaoNo ratings yet
- Perioperative Thermoregulation and Heat BalanceDocument10 pagesPerioperative Thermoregulation and Heat BalanceGio VandaNo ratings yet
- Warm UpDocument12 pagesWarm Upmeor1906No ratings yet
- Ice Freezes Pain A Review of The Clinical Effectiveness of Analgesic Cold PDFDocument4 pagesIce Freezes Pain A Review of The Clinical Effectiveness of Analgesic Cold PDFMatin Abdillah GogaNo ratings yet
- Ford (2006) Prolonged Unintended Brain Cooling May Inhibit Recovery From Brain Injuries: Case Study and Literature ReviewDocument7 pagesFord (2006) Prolonged Unintended Brain Cooling May Inhibit Recovery From Brain Injuries: Case Study and Literature ReviewMarthasWisdomNo ratings yet
- CryotherapyDocument54 pagesCryotherapyAhmed Baghdadi100% (1)
- Selected Topics in Environmental Biology: Based on the Sessions on Environmental Biology Held at the XXVI International Congress of Physiological Sciences, New Delhi, October 20-26, 1974From EverandSelected Topics in Environmental Biology: Based on the Sessions on Environmental Biology Held at the XXVI International Congress of Physiological Sciences, New Delhi, October 20-26, 1974Balraj BhatiaNo ratings yet
- The Ice Bath Path To Enhanced Sperm Health And Fertility - Based On The Teachings Of Dr. Andrew Huberman: Ice Baths And Male Reproductive HealthFrom EverandThe Ice Bath Path To Enhanced Sperm Health And Fertility - Based On The Teachings Of Dr. Andrew Huberman: Ice Baths And Male Reproductive HealthNo ratings yet
- Exhibit 1-2 InsertDocument2 pagesExhibit 1-2 Insertmaggie305No ratings yet
- 2000 Sydney Swogsys2000Document238 pages2000 Sydney Swogsys2000maggie305No ratings yet
- Blue TipsDocument4 pagesBlue Tipsmaggie305No ratings yet
- Geurts 2005 CGP2Document8 pagesGeurts 2005 CGP2maggie305No ratings yet