Professional Documents
Culture Documents
Presion AI EE 2010 Jase
Uploaded by
Walter Manuel Yañez CamachoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Presion AI EE 2010 Jase
Uploaded by
Walter Manuel Yañez CamachoCopyright:
Available Formats
CLINICAL INVESTIGATIONS
LV DIASTOLIC FUNCTION AND LA FUNCTION
Do Additional Echocardiographic Variables Increase the Accuracy of E/e0 for Predicting Left Ventricular Filling Pressure in Normal Ejection Fraction? An Echocardiographic and Invasive Hemodynamic Study
Hisham Dokainish, MD, John S. Nguyen, MD, Ranjita Sengupta, MD, Manu Pillai, MD, Mahboob Alam, MD, Jaromir Bobek, RCIS, and Nasser Lakkis, MD, Houston, Texas
Background: There are few data on adding left atrial volume index (LAVi) or pulmonary artery systolic pressure (PAP) to the ratio of early mitral inow to mitral annular velocity (E/e0 ) for the estimation of left ventricular (LV) lling pressure in patients with preserved LV ejection fractions (LVEFs) (>50%). Methods: Patients underwent echocardiography within 20 minutes of cardiac catheterization. Echocardiographic variables were compared with invasively measured LV preatrial contraction pressure (pre-A). Results: Of the 122 patients studied (mean age, 55 6 9 years; mean LVEF, 61 6 6%), 67 (55%) were women, 108 (88%) had hypertension, and 79 (65%) had signicant coronary artery disease at catheterization. E/e0 was significantly correlated with pre-A (R = 0.63, P < .0001) compared with LAVi (R = 0.49, P < .001) and PAP (R = 0.48, P < .001). E/e0 > 13 had sensitivity of 70% and specicity of 93% (area under the curve [AUC], 0.82; P < .0001), LAVi > 31 mL/m2 had sensitivity of 78% and specicity of 76% (AUC, 0.80, P < .001), and PAP > 28 mm Hg had sensitivity of 80% and specicity of 64% for pre-A > 15 mm Hg (AUC, 0.77, P < .001). Adding LAVi >31 mL/m2 for E/e0 = 8 to 13 signicantly increased the accuracy of E/e0 > 13 alone (sensitivity, 87%; specicity, 88%; AUC, 0.89; P = .01 for comparison). However, adding PAP > 28 mm Hg for E/e0 = 8 to 13 did not signicantly increase the accuracy of E/e0 > 13 alone (AUC, 0.82; sensitivity, 82%; specicity, 72%; P = NS for comparison). Conclusions: In patients with preserved LVEFs, adding LAVi > 31 mL/m2 to E/e0 (when E/e0 was in the gray zone, but not when E/e0 was >13) signicantly increased the accuracy of E/e0 alone for the estimation of LV lling pressure. These data support the notion of using several, rather than any single, Doppler echocardiographic parameter for the accurate assessment of LV diastolic function. (J Am Soc Echocardiogr 2010;23:156-61.) Keywords: Diastolic function, Doppler tissue imaging, Hemodynamics Diastolic heart failure constitutes a major portion of the heart failure epidemic.1 Along with a suitable clinical picture and preserved left ventricular (LV) ejection fraction (LVEF) (>50%), recent clinical guidelines have recommended the use of echocardiography with Doppler (or cardiac catheterization) for the demonstration of a level of diastolic dysfunction required for a diagnosis of diastolic heart failure.2-7 Echocardiographic peak mitral inow/early diastolic annular velocity (E/e0 ) has been shown to correlate with LV lling pressure,8-15 including during exercise,16-19 and is currently recommended by the American Society of Echocardiography and the EuroFrom the Department of Medicine, Section of Cardiology, Baylor College of Medicine, Houston, Texas. Reprint requests: Hisham Dokainish, MD, McMaster University Health Sciences Centre, Department of Medicine, Section of Cardiology, 237 Barton Street E, CVSRI #C3-111, Hamilton, ON L8L 2X2, Canada (E-mail: hisham.dokainish@ phri.ca). 0894-7317/$36.00 Copyright 2010 by the American Society of Echocardiography. doi:10.1016/j.echo.2009.11.015
pean Society of Echocardiography as the initial screening variable for estimating LV lling pressure in patients with preserved LVEFs.20 Given that the accuracy of E/e0 has been recently challenged as an estimate of LV lling pressure,21-23 we sought to determine whether there was any incremental benet to adding other echocardiographic variables shown to correlate with LV lling pressureleft atrial volume index (LAVi)24 and pulmonary artery systolic pressure (PAP)25,26to E/e0 for the estimation of LV lling pressure.
METHODS This study protocol was approved by the institutional review board of the Baylor College of Medicine. Consecutive patients referred to the cardiac catheterization laboratory for coronary angiography for clinical reasons were approached for recruitment. After informed consent, patients underwent left-heart catheterization via a retrograde approach from the femoral artery. The aortic valve was crossed to determine LV diastolic pressures, and coronary angiography was performed by selective injection of the coronary ostia. LV preatrial contraction
156
Journal of the American Society of Echocardiography Volume 23 Number 2
Dokainish et al 157
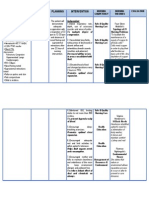
Table 1 Baseline, echocardiographic, and catheterization data
LV pre-A < 15 mm Hg Variable (n = 54) LV pre-A > 15 mm Hg (n = 68) P
Baseline characteristics Age (y) Women Body surface area (m2) Hypertension Diabetes mellitus Hypercholesterolemia Current smokers Medications b-blockers ACE inhibitors/angiotensin receptor blockers Calcium channel blockers Statins Diuretics Echocardiography and Doppler LV diastolic dimension (cm) LV mass index (g/m2) LAVi (mL/m2) RV diastolic dimension (cm) Right atrial volume index (mL/m2) LV ejection fraction (%) RV fractional area change (%) Mitral E (cm/s) Mitral A (cm/s) Mitral E/A Mitral deceleration time (cm/s) PAP (mm Hg) Mitral E0 average (cm/s) Mitral E/e0 , septal annulus Mitral E/e0 , lateral annulus Mitral E/e0 , average of annuli Catheterization data Heart rate (beats/min) Systolic blood pressure (mm Hg) Diastolic blood pressure (mm Hg) LV end-diastolic pressure (mm Hg) LV pre-A (mm Hg) Signicant CAD on angiography ACE, Angiotensin-converting enzyme; RV, right ventricular. Data are expressed as mean 6 SD or as number (percentage).
55.4 6 9.6 30 (56%) 2.0 6 0.3 46 (85%) 29 (53%) 39 (72%) 11 (20%) 39 (72%) 32 (59%) 7 (13%) 34 (63%) 13 (24%) 4.3 6 0.8 89.6 6 26.9 27.9 6 6.9 3.1 6 0.5 19.5 6 8.2 61.6 6 6.4 41.2 6 4.9 72.8 6 15.4 74.6 6 16.1 0.98 6 0.19 206.3 6 54.1 26.1 6 5.4 7.2 6 1.8 12.2 6 3.1 9.3 6 2.3 10.7 6 2.6 69.9 6 9.7 140.6 6 22.3 79.1 6 11.8 16.3 6 4.0 10.8 6 2.4 30 (56%)
55.3 6 8.4 37 (54%) 2.0 6 0.3 62 (91%) 38 (55%) 59 (86%) 16 (23%) 48 (70%) 47 (69%) 11 (16%) 51 (75%) 28 (41%) 4.7 6 0.7 105.7 6 40.8 37.1 6 16.1 3.2 6 0.4 20.1 6 4.8 60.5 6 6.2 42.0 6 7.4 89.1 6 18.0 81.4 6 22.0 1.10 6 0.30 206.7 6 49.3 33.3 6 9.4 7.0 6 2.7 17.6 6 6.5 14.0 6 5.7 15.8 6 4.8 67.0 6 11.8 140.1 6 26.5 76.0 6 12.1 26.4 6 6.7 19.5 6 4.5 49 (72%)
.94 .91 .90 .61 .91 .16 .92 .57 .61 .92 .44 .12 .05 .01 <.001 .88 .69 .40 .77 <.001 .06 .007 .96 <.001 .63 <.001 <.001 <.001 .30 .98 .25 <.001 <.001 .14
pressure (pre-A) and end-diastolic pressure were measured over 10 cardiac cycles during free respiration and then averaged. Standard diagnostic views of the left and right coronary anatomy were obtained, and lesions >70% in diameter in major epicardial arteries represented signicant coronary artery disease (CAD). Readings of invasive cardiac hemodynamics and coronary anatomy were performed by an invasive cardiologist blinded to all clinical and echocardiographic data. A comprehensive transthoracic Doppler echocardiographic examination was performed immediately after catheterization (all studies <20 minutes from catheterization). Patients were excluded if they had nonsinus rhythm, severe mitral regurgitation, any mitral stenosis, or prosthetic mitral valves, because these conditions render Doppler estimations of LV lling pressures less reliable. Studies were performed on a GE Vivid 7 ultrasonographic machine (GE Healthcare, Milwaukee, WI). Two-dimensional measurements were performed according to the American Society of Echocardiography27 and included LVEF by the biplane method of discs, maximal left atrial volume by the biplane method of discs, and LV mass by the area-
length method; the latter two variables were indexed to body surface area. Preserved LVEF was dened as >50%.2,5-7 Pulsed Doppler was used to record transmitral inow in the apical 4-chamber view.28 Tissue Doppler velocities were then acquired at the septal and lateral annular sites and averaged as previously described.11,12,29 Studies were analyzed by an echocardiologist blinded to all clinical and catheterization data. Mitral inow measurements included peak early (E) and peak late (A) velocities, the E/A ratio, and the deceleration time of E.28 PAP was estimated by adding the peak tricuspid regurgitation velocity, converted to peak pressure by the modied Bernoulli equation, to an estimate of right atrial pressure. The estimate of right atrial pressure was made using the following: right atrial pressure = 5 mm Hg if the inferior vena cava (IVC) was <2 cm in diameter and had >50% inspiratory collapse, 10 mm Hg if the IVC was >2 cm in diameter and had >50% inspiratory collapse, and 15 mm Hg if the IVC was >2 cm in diameter and had <50% inspiratory collapse.30 The early diastolic (e0 ) velocity by tissue Doppler at the septal and lateral annular sites was measured and the E/e0 ratio computed using the average of
158 Dokainish et al
Journal of the American Society of Echocardiography February 2010
Figure 1 Correlations of LV pre-A with (A) E/e0 , (B) LAVi, and (C) PAP. septal and lateral e0 , as previously described.11,12,20,29 Three cardiac cycles were measured and averaged for all Doppler measurements. Continuous data are presented as mean 6 SD and categorical data as number (percentage). For continuous variables, Students t test was performed, and for dichotomous variables, the c2 test was used. Linear regression was performed to determine the correlations between continuous variables. Sensitivity, specicity, and positive and negative predictive values were calculated according to standard denitions, and receiver operating characteristic curves were constructed and the areas under the curve (AUCs) calculated to determine the optimal cutoff values of the best correlates with LV pre-A for the prediction of LV pre-A > 15 mm Hg. For incremental accuracy, in addition to E/e0 > 13 (the optimum cutoff from AUC calculation), LAVi > 31 mL/m2 was added (the optimum cutoff from AUC calculation) for E/e0 = 8 to 13 to indicate elevated LV lling pressure.20 The same approach was applied for PAP > 28 mm Hg (the optimum cutoff from AUC calculation). The accuracy of these combined variables for predicting LV pre-A > 15 mm Hg was then recalculated. The Hanley-McNeil test was used to assess for signicant differences between AUCs. P values < .05 were considered signicant. Analyses were performed with
Journal of the American Society of Echocardiography Volume 23 Number 2
Dokainish et al 159
SigmaStat 3.0 (Systat Software, Point Richmond, CA) and GraphPad Prism Plus (GraphPad Software, San Diego, CA). RESULTS Of 275 patients referred for cardiac catheterization screened, 110 were excluded for depressed LVEFs (<50%), 27 for nonsinus rhythm, 9 for mitral stenosis or prosthetic mitral valves, and 7 in whom the aortic valve could not be crossed. Thus, 122 patients with preserved LVEFs (>50%) were enrolled, of whom 67 (55%) were women, 107 (88%) had hypertension, 67 (55%) had diabetes, and 27 (22%) were current smokers. The mean age was 55.4 6 9.0 years, the mean LVEF was 60.9 6 6.1%, and 79 (65%) had signicant CAD at catheterization. When the population was divided into the 54 patients with LV pre-A < 15 mm Hg and the 68 patients with pre-A > 15 mm Hg, there were no signicant differences in age (P = .94), systolic blood pressure (P = .98), the prevalence of diabetes (P = .91), the prevalence of hypertension (P = .61), current smoking status (P = .92), hypercholesterolemia (P = .16), and the numbers of patients on b-blockers (P = .57), angiotensin-converting enzyme inhibitors (P = .61), and statins (P = .44) (Table 1). Among echocardiographic variables, LV diastolic dimension and LAVi were larger and LV mass index, peak mitral E velocity, and PAP were higher in patients with LV pre-A > 15 mm Hg compared with those with LV pre-A < 15 mm Hg (Table 1). E/e0 had a reasonable correlation with LV pre-A (R = 0.63, P < .001), compared with LAVi (R = 0.49, P < .001) and PAP (R = 0.48, P < .001) (Figure 1). Peak E velocity was also a signicant echocardiographic correlate of LV pre-A (R = 0.48, P < .001); however, mitral deceleration time (R = 0.04, P = .66) was not correlated with LV pre-A. In the 79 patients (62%) with signicant angiographic CAD, correlation of LV pre-A with E/e0 was R = 0.66 (P < .001) compared with R = 0.58 (P < .001) in the 43 patients (38%) without signicant angiographic CAD (P = NS for comparison). Similarly, in patients with CAD, the correlation of LAVi with LV pre-A was R = 0.49 (P < .001) compared with R = 0.48 (P < .001) in patients without signicant CAD (P = NS for comparison). PAP too had a similar correlation with LV pre-A in patients with versus without signicant angiographic CAD (R = 0.47, P < .001 vs R = 0.49, P < .001; P = NS for comparison). E/e0 > 13 was the optimum cutoff value to predict LV pre-A > 15 mm Hg (sensitivity, 70%; specicity, 93%; AUC, 0.82; P < .0001; Figure 2), compared with LAVi > 31 mL/m2 (sensitivity, 78%; specicity, 76%; AUC, 0.80; P < .0001) and PAP > 28 mm Hg (sensitivity, 80%; specicity, 64%; AUC, 0.77; P = .0001). In the 53 patients with E/e0 ratios between 8 and 13, LAVi was > 31 mL/m2 in 18 (34%), of whom 13 (72%) had LV pre-A > 15 mm Hg. Therefore, adding LAVi > 31 mL/ m2 to E/e0 in these patients signicantly increased the accuracy of E/e0 > 13 alone for predicting LV pre-A > 15 mm Hg (specicity, 87%; specicity, 88%; AUC, 0.89; P = .01 for comparison; Figure 2. In the 54 patients with E/e0 ratios > 13, LAVi was < 31 mL/m2 in 14 (26%), of whom 4 (29%) had LV pre-A > 15 mm Hg; therefore, adding LAVi > 31 mL/ m2 to E/e0 did not increase the diagnostic accuracy of E/e0 alone (sensitivity, 79%; specicity, 80%; AUC, 0.81; P < .0001; P = NS for comparison). Furthermore, adding PAP > 28 mm Hg for E/e0 = 8 to 13 (or E/e0 > 13) did not signicantly change the accuracy of E/e0 > 13 alone (sensitivity, 82%; specicity, 72%; AUC, 0.82; P = NS for comparison). DISCUSSION This study for the rst time demonstrates an incremental benet in accuracy when LAVi is added to E/e0 (when E/e0 was in the gray zone, Figure 2 Receiver operating characteristic curves to predict LV pre-A > 15 mm Hg for (A) E/e0 > 13, (B) LAVi > 31 mL/m,2 and (C) E/e0 > 13, plus adding LAVi > 31 mL/m2 in patients with E/e0 ratios of 8 to 13.
160 Dokainish et al
Journal of the American Society of Echocardiography February 2010
but not when E/e0 was >13) for the prediction of invasively measured LV lling pressure in a large cohort of patients with preserved LVEFs. These data help reinforce the message, as recommended in the American Society of Echocardiography and European Society of Echocardiography guidelines for LV diastolic function20 as well as in other documents,28,31 that the sole use of any single Doppler echocardiographic parameter, including E/e0 , is not suitable for the accurate assessment of LV diastolic function; rather, the use of several parameters is preferred. Prior studies have shown that E/e0 is a reliable estimate of LV lling pressure, but most of these studies included large proportions of patients with depressed LVEFs (<50%) and further demonstrated that E/e0 was more accurate for LV lling pressure estimation in patients with depressed rather than preserved LVEFs.8-14 One study showed that E/e0 > 8 was a reasonably accurate predictor of LV end-diastolic pressure > 12 mm Hg in 43 patients with preserved LVEFs.15 Our study supports these ndings, as it validates E/e0 for the estimation of LV lling pressure in a larger group of patients with cardiac disease and preserved LVEFs. However, our study was performed in a very different population: patients referred for cardiac catheterization with a high burden of hypertension, diabetes mellitus, and CAD, as opposed to younger patients with a much lower burden of cardiac disease and risks factors.15 In patients with cardiac disease, an LV end-diastolic pressure > 12 mm Hg15 does not, in our experience, necessarily correlate with symptoms and signs of diastolic heart failure; indeed, higher cutoff values for LV lling pressure are often needed.4,20,28,31-33 Similarly, E/e0 > 8 can be considered a rather low cutoff level; rather, E/e0 > 12 is often needed in patients with preserved LVEFs to assist in the diagnosis of heart failure, as seen in this and prior studies.2-4,8-14,20,28,31 Given that some work has cast doubt on the accuracy of E/e0 in isolation for the prediction of LV lling pressure,21-23 we sought to determine the incremental value of adding other signicant correlates of LV lling pressure (LAVi and PAP) to E/e0 . Our nding that adding LAVi to E/e0 (when E/e0 is in the gray zone) signicantly increases its accuracy for the prediction of LV lling pressure strengthens the potential clinical utility of E/e0 and may cut down on errors arising from the use of E/e0 alone in patients with preserved LVEFs. That PAP did not signicantly add to E/e0 was possibly due to the ability to measure PAP in only 70% our patients, thus potentially limiting its usefulness as an added parameter in daily clinical practice. This does not necessarily mean, however, that in a given patient, when PAP is measureable, it cannot be used in conjunction with E/e0 to help determine LV lling pressure given the signicantly higher PAP in patients with LV pre-A > 15 mm Hg compared with <15 mm Hg in this study, as well as in prior data.25,26 The cutoff values in this study for the prediction of elevated LV lling pressure, namely E/e0 > 13, LAVi > 31 mL/m2, and PAP > 28 mm Hg, are similar to those recommended in the recent American Society of Echocardiography guidelines for the evaluation of diastolic function.20 In particular, we used the average of the septal and lateral mitral annuli to calculate e0 for use in the E/e0 ratio and, on the basis of receiver operating characteristic analysis, came up with a nearly identical cutoff value for E/e0 using the average of the annuli, as recommended in the guidelines.20 This speaks to the robustness of the cutoff of E/e0 > 13 for elevated LV lling pressures in patients with preserved LVEFs. The cutoff value of LAVi > 31 mL/m2, though somewhat lower than that used in the guidelines (>34 mL/m2) is nonetheless consistent with the cutoff value for LAVi used in prior papers as well as in prognostic studies.34-37 The physiologic rationale for adding LAVi to E/e0 is likely due to the fact that LAVi can be considered a barometer of elevated LV ling
pressures and LV diastolic dysfunction.20,34-37 Thus, in a given patient with a borderline E/e0 value with a preserved LVEF (for example, E/e0 = 11), if the LAVi is enlarged, this would suggest that this E/e0 value occurs in the milieu of chronic diastolic dysfunction, arguably increasing the likelihood of elevated LV lling pressure at that given time. By contrast, if that same patient with an E/e0 of 11 had a normal (or small) LAVi, that would imply that this particular E/e0 value is likely occurring in the absence of signicant chronic diastolic dysfunction, arguing against the presence of elevated LV lling pressure at that given moment. From a statistical point of view, as shown in this study, E/e0 > 13 had a higher specicity (93%) than sensitivity (70%) for LV preA > 15 mm Hg in this population. Therefore, in patients with E/e0 ratios of 8 to 13, some of whom may still have elevated LV lling pressures, an enlarged LAVi helps identify those who may have elevations of left atrial pressure that were not detected by E/e0 alone. However, the most important point of this study is arguably that, as stated in the guidelines20 as well as other diastolic function documents,28,31 the use of more than one Doppler echocardiographic parameter is preferable to using any single parameter alone, including E/e0 , for the accurate estimation of LV lling pressure, a notion supported by our data. Limitations The patients in this study had a high prevalence of hypertension, diabetes, and CAD. Therefore, these ndings may not necessarily translate to populations that contain a signicant percentage of patients without myocardial disease (ie, normal hearts with normal LV relaxation).38 Although the cutoff values for E/e0 and LAVi derived in this study were not prospectively validated in a different patient cohort, the values are nearly identical to those in the American Society of Echocardiography and European Society of Echocardiography guidelines for LV diastolic function.20 Because this was a clinical study, uid-lled catheters, not solid conductance catheters, were used for invasive measurements, but an average of 10 cardiac cycles was used to minimize measurement error for invasive hemodynamics, and these ndings may better reect invasive measurements made in daily practice. As mentioned above, PAP was obtainable in 70% of patients, potentially limiting its widespread use for the estimation of LV lling pressure.
CONCLUSIONS Adding LAVi to E/e0 (when E/e0 is in the gray zone, but not when E/e0 is >13) signicantly improves the accuracy of E/e0 alone for the estimation of LV lling pressures in patients with preserved LVEFs. This supports the notion that the use of several Doppler echocardiographic variables is preferable to using any single variable alone for the assessment of LV diastolic function. REFERENCES
1. Bursi F, Weston SA, Redeld MM, Jacobsen SJ, Pakhomov S, Nkomo VT, et al. Systolic and diastolic heart failure in the community. JAMA 2006; 296:2209-16. 2. Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 2007;28:2539-50. 3. Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur Heart J 2008;29:2388-442.
Journal of the American Society of Echocardiography Volume 23 Number 2
Dokainish et al 161
4. Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, et al. 2009 focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2009;119: e391-479. 5. Aurigemma GP, Gaasch WH. Clinical practice. Diastolic heart failure. N Engl J Med 2004;351:1097-105. 6. Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure: part I: diagnosis, prognosis, and measurements of diastolic function. Circulation 2002;105:1387-93. 7. Vasan R, Levy D. Dening diastolic heart failure: a call for standardized diagnostic criteria. Circulation 2000;101:2118-21. 8. Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of lling pressures. J Am Coll Cardiol 1997;30:1527-33. 9. Sohn DW, Chai IH, Lee DJ, Kim HC, Kim HS, Oh BH, et al. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol 1997;30:474-80. 10. Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redeld MM, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular lling pressures: a comparative simultaneous Doppler-catheterization study. Circulation 2000;102: 1788-94. 11. Rivas-Gotz C, Khoury DS, Manolios M, Rao L, Kopelen HA, Nagueh SF. Impact of left ventricular ejection fraction on estimation of left ventricular lling pressures using tissue Doppler and ow propagation velocity. Am J Cardiol 2002;91:780-4. 12. Dokainish H, Zoghbi WA, Lakkis NM, Al-Bakshy F, Dhir M, Quinones MA, et al. Optimal non-invasive assessment of LV lling pressures: a comparison of tissue Doppler echocardiography and BNP in patients with pulmonary artery catheters. Circulation 2004;109:2432-9. 13. Bruch C, Grude M, Muller J, Breithardt G, Wichter T. Usefulness of tissue Doppler imaging for estimation of left ventricular lling pressures in patients with systolic and diastolic heart failure. Am J Cardiol 2005;95:892-5. 14. Arques S, Roux E, Sbragia P, Gelisse R, Ambrosi P, Pieri B, et al. Comparative accuracy of color M-mode and tissue Doppler echocardiography in the emergency diagnosis of congestive heart failure in chronic hypertensive patients with normal left ventricular ejection fraction. Am J Cardiol 2005;96:1456-9. 15. Kasner M, Westermann D, Steendijk P, Gaub R, Wilkenshoff U, Weitmann K, et al. Utility of Doppler echocardiography and tissue Doppler imaging in the estimation of diastolic function in heart failure with normal ejection fraction: a comparative Doppler-conductance catheterization study. Circulation 2007;116:637-47. 16. Nakajima Y, Kane GC, McCully RB, Ommen SR, Pellikka PA. Left ventricular diastolic lling pressures during dobutamine stress echocardiography: relationship to symptoms and ischemia. J Am Soc Echocardiogr 2009;22: 947-53. 17. Dalsgaard M, Kjaergaard J, Pecini R, Iversen KK, Kober L, Moller JE, et al. Left ventricular lling pressure estimation at rest and during exercise in patients with severe aortic valve stenosis: comparison of echocardiographic and invasive measurements. J Am Soc Echocardiogr 2009;22:343-9. 18. Fukuta H, Little WC. Elevated left ventricular lling pressure after maximal exercise predicts increased plasma B-type natriuretic peptide levels in patients with impaired relaxation pattern of diastolic lling. J Am Soc Echocardiogr 2007;20:832-7. 19. Talreja DR, Nishimura RA, Oh JK. Estimation of left ventricular lling pressure with exercise by Doppler echocardiography in patients with normal systolic function: a simultaneous echocardiographic-cardiac catheterization study. J Am Soc Echocardiogr 2007;20:477-9. 20. Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 2009;22:107-33. 21. Mullens W, Borowski AG, Curtin RJ, Thomas JD, Tang WH. Tissue Doppler imaging in the estimation of intracardiac lling pressure in decompen-
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
sated patients with advanced systolic heart failure. Circulation 2009;119: 62-70. Geske JB, Sorajja P, Nishimura RA, Ommen SR. Evaluation of left ventricular lling pressures by Doppler echocardiography in patients with hypertrophic cardiomyopathy: correlation with direct left atrial pressure measurement at cardiac catheterization. Circulation 2007;116:2702-8. Petrie MC, Hogg K, Caruana L, McMurray JJ. Poor concordance of commonly used echocardiographic measures of left ventricular diastolic function in patients with suspected heart failure but preserved systolic function: is there a reliable echocardiographic measure of diastolic dysfunction? Heart 2004;90:511-7. Appleton CP, Galloway JM, Gonzalez MS, Gaballa M, Basnight MA. Estimation of left ventricular lling pressures using two-dimensional and Doppler echocardiography in adult patients with cardiac disease. Additional value of analyzing left atrial size, left atrial ejection fraction and the difference in duration of pulmonary venous and mitral ow velocity at atrial contraction. J Am Coll Cardiol 1993;22:1972-82. Bouchard JL, Aurigemma GP, Hill JC, Ennis CA, Tighe DA. Usefulness of the pulmonary arterial systolic pressure to predict pulmonary arterial wedge pressure in patients with normal left ventricular systolic function. Am J Cardiol 2008;101:1673-6. Lam CS, Roger VL, Rodeheffer RJ, Borlaug BA, Enders FT, Redeld MM. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol 2009;53:1119-26. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantication: a report from the American Society of Echocardiographys Guidelines and Standards Committee and the Chamber Quantication Writing Group. J Am Soc Echocardiogr 2005;18:1440-63. Lester SJ, Tajik AJ, Nishimura RA, Oh JK, Khandheria BK, Seward JB. Unlocking the mysteries of diastolic function: deciphering the Rosetta Stone 10 years later. J Am Coll Cardiol 2008;51:679-89. Dokainish H, Sengupta R, Pillai M, Bobek J, Lakkis N. Correlation of tissue Doppler and two-dimensional speckle myocardial velocities and comparison of derived ratios with invasively measured left ventricular lling pressures. J Am Soc Echocardiogr 2009;22:284-9. Kircher BJ, Himelman RB, Schiller NB. Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol 1990;66:493-6. Oh JK, Hatle L, Tajik AJ, Little WC. Diastolic heart failure can be diagnosed by comprehensive two-dimensional and Doppler echocardiography. J Am Coll Cardiol 2006;47:500-6. Zile MR, Gaasch WH, Carroll JD, Feldman MD, Aurigemma GP, Schaer GL, et al. Heart failure with a normal ejection fraction: is measurement of diastolic function necessary to make the diagnosis of diastolic heart failure? Circulation 2001;104:779-82. Kuecherer H, Ruffmann K, Kuebler W. Determination of left ventricular lling parameters by pulsed Doppler echocardiography: a noninvasive method to predict high lling pressures in patients with coronary artery disease. Am Heart J 1988;116:1017-21. Tsang TS, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol 2002;90:1284-9. Pritchett AM, Mahoney DW, Jacobsen SJ, Rodeheffer RJ, Karon BL, Redeld MM. Diastolic dysfunction and left atrial volume: a populationbased study. J Am Coll Cardiol 2005;45:87-92. Abhayaratna WP, Seward JB, Appleton CP, Douglas PS, Oh JK, Tajik AJ, et al. Left atrial size: physiologic determinants and clinical applications. J Am Coll Cardiol 2006;47:2357-63. Dokainish H, Zoghbi WA, Lakkis NM, Ambriz E, Patel R, Quinones MA, et al. Incremental predictive power of B-type natriuretic peptide and tissue Doppler echocardiography in the prognosis of patients with congestive heart failure. J Am Coll Cardiol 2005;45:1223-6. Firstenberg MS, Levine BD, Garcia MJ, Greenberg NL, Cardon L, Morehead AJ, et al. Relationship of echocardiographic indices to pulmonary capillary wedge pressures in healthy volunteers. J Am Coll Cardiol 2000;36:1664-9.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Heart Rate Response Pattern To Dialysis Hypotension in Haemodialysis PatientsDocument6 pagesThe Heart Rate Response Pattern To Dialysis Hypotension in Haemodialysis PatientsAnton SampNo ratings yet
- Quiz Week 2 (Blood Pressure)Document9 pagesQuiz Week 2 (Blood Pressure)María Paula Cristancho GalvisNo ratings yet
- Conversation Midwife With Patient On Examination PregnancyDocument5 pagesConversation Midwife With Patient On Examination Pregnancyachy chanNo ratings yet
- Fluid Guideline SaTHDocument18 pagesFluid Guideline SaTHpaulito_delgadoNo ratings yet
- Case NCPDocument25 pagesCase NCPJoher Bolante Mendez100% (1)
- The Effect of Sexual Arousal and Emotional ArousalDocument21 pagesThe Effect of Sexual Arousal and Emotional ArousalRay chijiokeNo ratings yet
- Assessing hand hygiene of nursing and medical studentsDocument12 pagesAssessing hand hygiene of nursing and medical studentsDurga Shankar DhakarNo ratings yet
- Maritime medical records portalDocument5 pagesMaritime medical records portalSoekhaidir SuripnoNo ratings yet
- ReadingSkills DevelopmentA4Document18 pagesReadingSkills DevelopmentA4ardeliaNo ratings yet
- The Pediatric Early Warning System Score: A Severity of Illness Score To Predict Urgent Medical Need in Hospitalized ChildrenDocument8 pagesThe Pediatric Early Warning System Score: A Severity of Illness Score To Predict Urgent Medical Need in Hospitalized ChildrenRavikiran SuryanarayanamurthyNo ratings yet
- Essay Practice Module Form 5 Biology Chapter 1.2Document4 pagesEssay Practice Module Form 5 Biology Chapter 1.2Thanaletchumy ChandrasegarNo ratings yet
- The Physiology of ShockDocument37 pagesThe Physiology of ShockGauxy AromboNo ratings yet
- Cardiopulmonary Resuscitation: Unit 7Document15 pagesCardiopulmonary Resuscitation: Unit 7حيدر الاسديNo ratings yet
- Central Venous PressureDocument4 pagesCentral Venous Pressuremike_steven12No ratings yet
- 2016 Esc Guidelines For The Diagnosis and Treatment of Acute and 2016Document85 pages2016 Esc Guidelines For The Diagnosis and Treatment of Acute and 2016aslinNo ratings yet
- Hypertensive Disorders in PregnancyDocument7 pagesHypertensive Disorders in PregnancyCaleb biiNo ratings yet
- Physiology and Cardiovascular System ReviewDocument29 pagesPhysiology and Cardiovascular System ReviewAssale Maen100% (1)
- This Study Resource WasDocument4 pagesThis Study Resource WasOrange AlvarezNo ratings yet
- Monitor Fetal C22Document4 pagesMonitor Fetal C22Juliana Jaramillo LedesNo ratings yet
- Normal Body TemperatureDocument2 pagesNormal Body TemperatureGrace Angelica TolitoNo ratings yet
- Chapter 6 (Cardiovascular Drugs) 2Document73 pagesChapter 6 (Cardiovascular Drugs) 2TES SENNo ratings yet
- PIIS0953620519303413Document7 pagesPIIS0953620519303413romyNo ratings yet
- Rigel Uni-SimDocument6 pagesRigel Uni-SimMatíasNo ratings yet
- Essential Hypertension - StudentsDocument43 pagesEssential Hypertension - StudentsMohamoud MohamedNo ratings yet
- LESSON PLAN On HypertensionDocument10 pagesLESSON PLAN On HypertensionPiyush Dutta100% (5)
- Xducers & P-MonitorsDocument22 pagesXducers & P-MonitorschanlalNo ratings yet
- Leadership Collaboration CommunicationDocument8 pagesLeadership Collaboration CommunicationAsma AliNo ratings yet
- FundamentsDocument57 pagesFundamentsGela CiluomNo ratings yet
- Hemodynamics in Critical CareDocument73 pagesHemodynamics in Critical CareMichael Ian Redito100% (3)
- Physical Education Grade 7: Patricia L. Meneses, LPT MapehDocument150 pagesPhysical Education Grade 7: Patricia L. Meneses, LPT MapehTrisha MenesesNo ratings yet