Professional Documents
Culture Documents
Idiopathic Pulmonary Fibrosis
Uploaded by
Carlos NiñoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Idiopathic Pulmonary Fibrosis
Uploaded by
Carlos NiñoCopyright:
Available Formats
Idiopathic pulmonary Iibrosis (IPF) is deIined as a speciIic Iorm oI chronic, progressive Iibrosing interstitial
pneumonia oI unknown cause, primarily occurring in older adults, limited to the lungs, and associated with the
histopathologic and/or radiologic pattern oI usual interstitial pneumonia (UIP).
|1|
OI the 7 listed idiopathic interstitial pneumonias in the American Thoracic Society/European Respiratory
Society consensus statement (ie, idiopathic pulmonary Iibrosis, nonspeciIic interstitial pneumonia, cryptogenic
organizing pneumonia, acute interstitial pneumonia, desquamative interstitial pneumonia, respiratory
bronchiolitis-associated interstitial pneumonia, lymphoid interstitial pneumonia), idiopathic pulmonary Iibrosis
is the most common.
|2|
Idiopathic pulmonary Iibrosis portends a poor prognosis, and, to date, no proven
eIIective therapies are available Ior the treatment oI idiopathic pulmonary Iibrosis beyond lung
transplantation.
|3|
Most patients with idiopathic pulmonary Iibrosis present with a gradual onset, oIten greater than 6 months, oI
dyspnea and/or a nonproductive cough. The symptoms oIten precede the diagnosis by a median oI 1-2 years.
|4|
A chest radiograph typically reveals diIIuse reticular opacities; however, it lacks diagnostic speciIicity.
|5|
High-
resolution computed tomography (HRCT) Iindings are signiIicantly more sensitive and speciIic Ior the
diagnosis oI idiopathic pulmonary Iibrosis. On HRCT images, usual interstitial pneumonia is characterized by
the presence oI reticular opacities oIten associated with traction bronchiectasis. As idiopathic pulmonary
Iibrosis progresses, honeycombing becomes more prominent.
|6|
Pulmonary Iunction tests oIten reveal restrictive
impairment and reduced diIIusing capacity Ior carbon monoxide.
|5|
Available data suggest that no single etiologic agent serves as a common inciting event in the pathogenesis oI
idiopathic pulmonary Iibrosis. During the past 15 years, the pathogenesis theory oI generalized inIlammation
progressing to widespread parenchymal Iibrosis has become less popular.
|5|
Rather, it is now believed that
epithelial injury and activation in Iibroblast Ioci are crucial early events that trigger a cascade oI changes
leading to reorganization oI pulmonary tissue compartments.
|7|
As mentioned above, idiopathic pulmonary Iibrosis is an idiopathic interstitial pneumonia characterized by
usual interstitial pneumonia on histopathology. The hallmark pathologic Ieature oI usual interstitial pneumonia
is a heterogeneous, variegated appearance with alternating areas oI healthy lung, interstitial inIlammation,
Iibrosis, and honeycomb change. Fibrosis predominates over inIlammation.
|7|
The diagnosis oI idiopathic pulmonary Iibrosis relies on the clinician integrating the clinical, laboratory,
radiologic, and/or pathologic data to make a clinical-radiologic-pathologic correlation that supports the
diagnosis oI idiopathic pulmonary Iibrosis.
|3|
The previous theory regarding the pathogenesis oI idiopathic pulmonary Iibrosis (IPF) was that generalized
inIlammation progressed to widespread parenchymal Iibrosis. However, anti-inIlammatory agents and immune
modulators have proved to be minimally eIIective in modiIying the natural course oI the disease. It is currently
believed that idiopathic pulmonary Iibrosis (IPF) is an epithelial-Iibroblastic disease, in which unknown
endogenous or environmental stimuli disrupt the homeostasis oI alveolar epithelial cells, resulting in diIIuse
epithelial cell activation and aberrant epithelial cell repair.
|8|
In the current hypothesis regarding the pathogenesis oI idiopathic pulmonary Iibrosis, exposure to an inciting
agent (eg, smoke, environmental pollutants, environmental dust, viral inIections, gastroesophageal reIlux
disease, chronic aspiration) in a susceptible host may lead to the initial alveolar epithelial damage.
|9|
Reestablishing an intact epithelium Iollowing injury is a key component oI normal wound healing. In idiopathic
pulmonary Iibrosis, it is believed that aIter injury, aberrant activation oI alveolar epithelial cells provokes the
migration, proliIeration, and activation oI mesenchymal cells with the Iormation oI Iibroblastic/myoIibroblastic
Ioci, leading to the exaggerated accumulation oI extracellular matrix with the irreversible destruction oI the lung
parenchyma.
|9|
Activated alveolar epithelial cells release potent Iibrogenic cytokines and growth Iactors. These include, tumor
necrosis Iactor-u (TNF-u), transIorming growth Iactor- (TGF-), platelet-derived growth Iactor, insulin-like
growth Iactor-1, and endothelin-1 (ET-1).
|7, 9|
These cytokines and growth Iactors are involved in the migration
and proliIeration oI Iibroblasts and the transIormation oI Iibroblasts into myoIibroblasts. Fibroblasts and
myoIibroblasts are key eIIector cells in Iibrogenesis, and myoIibroblasts secrete extracellular matrix proteins.
|9|
For normal wound healing to occur, wound myoIibroblasts must undergo apoptosis. Failure oI apoptosis leads
to myoIibroblast accumulation, exuberant extracellular matrix protein production, persistent tissue contraction,
and pathologic scar Iormation.
|9|
TGF- has been shown to promote an antiapoptotic phenotype in Iibroblasts.
|9|
Additionally, myoIibroblasts in Iibroblastic Ioci oI idiopathic pulmonary Iibrosis have been reported to undergo
less apoptotic activity in comparison to myoIibroblasts in the Iibromyxoid lesions oI bronchiolitis obliterans
organizing pneumonia.
|10|
Excess alveolar epithelial cell apoptosis and Iibroblast resistance to apoptosis are also believed to contribute to
IibroproliIeration in idiopathic pulmonary Iibrosis. Research has demonstrated that prostaglandin E
2
deIiciency,
in lung tissue oI patients with pulmonary Iibrosis, results in increased sensitivity oI alveolar epithelial cells to
FAS-ligand induced apoptosis but induces Iibroblast resistance to Fas-ligand induced apoptosis.
|11|
ThereIore,
apoptosis resistance in the Iibroblasts and myoIibroblasts participating in the repair oI the alveolar epithelium
may contribute to the persistent and/or progressive Iibrosis in idiopathic pulmonary Iibrosis.
Evidence Ior a genetic basis Ior idiopathic pulmonary Iibrosis is accumulating. It has been described that mutant
telomerase is associated with Iamilial idiopathic pulmonary Iibrosis.
|12|
Telomerase is a specialized polymerase
that adds telomere repeats to the ends oI chromosomes. This helps to oIIset shortening that occurs during DNA
replication. TGF- negatively regulates telomerase activity.
|9|
It is proposed that pulmonary Iibrosis in patients
with short telomeres is provoked by a loss oI alveolar epithelial cells. Telomere shortening also occurs with
aging, and it can also be acquired. This telomere shortening could promote the loss oI alveolar epithelial cells,
resulting in aberrant epithelial cell repair, and thereIore should be considered as another potential contributor to
the pathogenesis oI idiopathic pulmonary Iibrosis.
|12|
Additionally, a common variant in the putative promoter oI the gene that encodes mucin 5B (&) has been
associated with the development oI both Iamilial interstitial pneumonia and sporadic pulmonary Iibrosis.
& expression in the lung was reported to be 14.1 times as high in subjects who had idiopathic pulmonary
Iibrosis as in those who did not. ThereIore, dysregulated & expression in the lung may be involved in the
pathogenesis oI pulmonary Iibrosis.
|13|
Finally, caveolin-1 has been proposed as a protective regulator oI pulmonary Iibrosis. Caveolin-1 limits TGF-
induced production oI extracellular matrix proteins and restores the alveolar epithelial-repair process.
|9|
It has
been observed that the expression oI caveolin-1 is reduced in lung tissue Irom patients with idiopathic
pulmonary Iibrosis and that Iibroblasts, the key cellular component oI Iibrosis, have low levels oI caveolin-1
expression in patients with idiopathic pulmonary Iibrosis.
|14|
The recognition oI the above-mentioned Iactors as contributors to the pathogenesis oI idiopathic pulmonary
Iibrosis has led to the development oI novel approaches to treat idiopathic pulmonary Iibrosis.
The clinical symptoms oI idiopathic pulmonary Iibrosis are nonspeciIic. Most patients present with exertional
dyspnea and a nonproductive cough. Such symptoms can be shared with a variety oI pulmonary and cardiac
diseases. Dyspnea, which is the most prominent symptom in idiopathic pulmonary Iibrosis (IPF), usually begins
insidiously and is oIten progressive. Associated systemic symptoms can occur but are not common. Some oI
these systemic symptoms include weight loss, low-grade Ievers, Iatigue, arthralgias, or myalgias.
The reported median duration oI symptoms beIore the diagnosis oI idiopathic pulmonary Iibrosis is made is 1-2
years.
|5|
Most patients are reIerred to a cardiologist Ior evaluation oI exertional dyspnea prior to being reIerred
to a pulmonologist. Approximately 5 oI patients have no presenting symptoms when idiopathic pulmonary
Iibrosis is diagnosed. Among asymptomatic patients with idiopathic pulmonary Iibrosis (diagnosed by
radiographic abnormalities Iound on routine chest radiograph screening and lung biopsy showing usual
interstitial pneumonia), symptoms developed approximately 1000 days aIter the recognition oI the radiographic
abnormality.
|5|
It is critical to obtain a complete history, including medication history, social history, occupational history,
exposure history, and review oI systems, to ensure other causes oI interstitial lung disease are excluded.
Amiodarone, bleomycin, and nitroIurantoin are notable medications associated with pulmonary Iibrosis.
Oxidant stress Irom smoking may damage alveolar epithelial cells and contribute to the pathogenesis oI
idiopathic pulmonary Iibrosis.
|18|
Any patient with idiopathic pulmonary Iibrosis who is a current smoker should
be encouraged to quit. Any prior exposure to asbestos, silica, heavy metals, contaminated ventilation systems,
moldy Ioliage, and/or pigeon droppings should be investigated. Evidence oI arthralgia, arthritis,
photosensitivity, Raynaud phenomenon, dry eyes, and/or dry mouth on review oI systems may indicate the
presence oI a collagen-vascular disease.
Physicians should pay attention to historical clues that may suggest the presence oI obstructive sleep apnea
(OSA) because a 2009 study demonstrated the high prevalence oI OSA in patients with idiopathic pulmonary
Iibrosis. FiIty outpatients with stable idiopathic pulmonary Iibrosis were prospectively evaluated Ior the
presence oI OSA. OSA was deIined as an apnea-hypopnea index (AHI) oI greater than 5 events per hour. Ten
subjects (20) had mild OSA (AHI oI 5-15 events per hour) and 34 subjects (68) had moderate-to-severe
OSA (AHI oI ~15 events per hour).
|19|
ThereIore, the prevalence oI OSA in this sample was 88, suggesting
that OSA in patients with idiopathic pulmonary Iibrosis may have been previously underrecognized.
In most patients with idiopathic pulmonary Iibrosis, the physical examination reveals Iine bibasilar inspiratory
crackles (Velcro crackles). Additionally, digital clubbing is seen in 25-50 oI patients with idiopathic
pulmonary Iibrosis (IPF).
|5|
Extrapulmonary involvement does not occur with idiopathic pulmonary Iibrosis,
and, thereIore, physical examination Iindings do not help to conIirm the diagnosis.
Pulmonary hypertension is a common comorbidity in patients with idiopathic pulmonary Iibrosis, and an
estimated 20-40 oI patients with idiopathic pulmonary Iibrosis who are evaluated or listed Ior lung
transplantation have pulmonary hypertension at rest.
|20|
Physical examination Iindings may be suggestive oI the
presence oI pulmonary hypertension. Patients may have a loud P2 component oI the second heart sound, a Iixed
split S2, a holosystolic tricuspid regurgitation murmur, and pedal edema. As right ventricular hypertrophy
ensues, a right ventricular heave may be palpated at the lower leIt sternal border and increased right atrial
pressure may cause elevation oI the jugular venous pressure.
|21|
The etiology oI idiopathic pulmonary Iibrosis remains undeIined; however, in the current hypothesis regarding
the pathogenesis oI idiopathic pulmonary Iibrosis (IPF), exposure to an inciting agent (eg, smoke,
environmental pollutants, environmental dust, viral inIections, gastroesophageal reIlux disease, chronic
aspiration) in a susceptible host may lead to the initial alveolar epithelial damage.
|9|
This damage may lead to
activation oI the alveolar epithelial cells, which provokes the migration, proliIeration, and activation oI
mesenchymal cells with the Iormation oI Iibroblastic/myoIibroblastic Ioci, leading to the exaggerated
accumulation oI extracellular matrix with the irreversible destruction oI the lung parenchyma.
|9|
Other potential causes oI idiopathic pulmonary Iibrosis have been recognized through the study oI Iamilial
pulmonary Iibrosis. Familial pulmonary Iibrosis, aIIecting 2 or more members oI the same primary biological
Iamily, accounts Ior less than 5 oI total patients with idiopathic pulmonary Iibrosis.
|22|
Genetic mutations in serum surIactant protein C have been discovered in some individuals with Iamilial
pulmonary Iibrosis.
|22|
These mutations in serum surIactant protein C may damage type II alveolar epithelial
cells.
|22|
Additionally, a common variant in the putative promoter oI the gene encoding mucin 5B (&) has
been associated with the development oI both Iamilial interstitial pneumonia and sporadic pulmonary
Iibrosis.
|13|
Finally, mutant telomerase is associated with Iamilial idiopathic pulmonary Iibrosis.
|12|
Pulmonary Iibrosis in
patients with short telomeres is provoked by a loss oI alveolar epithelial cells. Telomere shortening also occurs
with aging and can also be acquired. This telomere shortening could promote the loss oI alveolar epithelial
cells, resulting in aberrant epithelial cell repair, and thereIore should be considered as another potential
contributor to the pathogenesis oI idiopathic pulmonary Iibrosis.
|12|
Hypoxia, or hypoxiation, is a pathological condition in which the body as a whole (generalized hypoxia) or a
region oI the body (tissue hypoxia) is deprived oI adequate oxygen supply. Variations in arterial oxygen
concentrations can be part oI the normal physiology, Ior example, during strenuous physical exercise. A
mismatch between oxygen supply and its demand at the cellular level may result in a hypoxic condition.
Hypoxia in which there is complete deprivation oI oxygen supply is reIerred to as anoxia.
Hypoxia diIIers Irom hypoxemia in that, in the latter, the oxygen concentration within the arterial blood is
abnormally low.
|1|
It is possible to experience hypoxia and have a low oxygen content (e.g., due to anemia) but
maintain high oxygen partial pressure (pO
2
). Incorrect use oI these terms can lead to conIusion, especially as
hypoxemia is among the causes oI hypoxia (in hypoxemic hypoxia).
Generalized hypoxia occurs in healthy people when they ascend to high altitude, where it causes altitude
sickness leading to potentially Iatal complications: high altitude pulmonary edema (HAPE) and high altitude
cerebral edema (HACE).
|2|
Hypoxia also occurs in healthy individuals when breathing mixtures oI gases with a
low oxygen content, e.g. while diving underwater especially when using closed-circuit rebreather systems that
control the amount oI oxygen in the supplied air. A mild and non-damaging intermittent hypoxia is used
intentionally during altitude trainings to develop an athletic perIormance adaptation at both the systemic and
cellular level.
|3|
Hypoxia is also a serious consequence oI preterm birth in the neonate. The main cause Ior this is that the lungs
oI the human Ioetus are among the last organs to develop during pregnancy. To assist the lungs to distribute
oxygenated blood throughout the body, inIants at risk oI hypoxia are oIten placed inside an incubator capable oI
providing continuous positive airway pressure (also known as a humidicrib).
Classification
O Hypoxemic hypoxia is a generalized hypoxia, an inadequate supply oI oxygen to the body as a whole.
The term "hypoxemic hypoxia" speciIies hypoxia caused by low partial pressure oI oxygen in arterial
blood. In the other causes oI hypoxia that Iollow, the partial pressure oI oxygen in arterial blood is
normal. Hypoxemic hypoxia may be due to:
4 Hypoventilation. Inadequate pulmonary minute ventilation (e.g., respiratory arrest or by drugs
such as opiates)
4 Shunts in the pulmonary circulation or a right-to-leIt shunt in the heart. Shunts can be caused by
collapsed alveoli that are still perIused or a block in ventilation to an area oI the lung. Whatever
the mechanism, blood meant Ior the pulmonary system is not ventilated and so no gas exchange
occurs (the ventilation/perIusion ratio is decreased).
Normal anatomical shunt occur due to Thebesian veins which empty into the leIt
ventricle and the bronchial circulation which supplies the bronchi with oxygen.
Normal physiological shunts occur due to the eIIect oI gravity. The highest concentration
oI blood in the pulmonary circulation occurs in the bases oI the pulmonary tree compared
to the highest pressure oI gas in the apices oI the lungs.
4 V/Q mismatch. When the ventilation does not match the perIusion through the paranchyema oI
the lung. This can occur Ior a variety oI reasons, the commonest being a Pulmonary embolism
4 DiIIusing deIects such as pulmonary Iibrosis where the Aa gradient has increased.
4 Decreased concentration oI oxygen in inspired air. Low partial pressure oI atmospheric oxygen
such as Iound at high altitude
|4|
or by reduced replacement oI oxygen in the breathing mix.
Low partial pressure oI oxygen in the lungs when switching Irom inhaled anaesthesia to
atmospheric air, due to the Fink eIIect, or diIIusion hypoxia.
O Anaemia in which arterial oxygen pressure is normal, but total oxygen content oI the blood is reduced.
This is due to a decreased total carrying capacity.
|5|
O Hypoxia when the blood Iails to deliver oxygen to target tissues.
4 Carbon monoxide poisoning which inhibits the ability oI hemoglobin to release the oxygen
bound to it.
4 Methaemoglobinaemia in which an abnormal version oI hemoglobin accumulates in the blood
O Histotoxic hypoxia in which quantity oI oxygen reaching the cells is normal, but the cells are unable to
use the oxygen eIIectively, due to disabled oxidative phosphorylation enzymes. Cyanide toxicity is one
example.
edit] Signs and symptoms
The symptoms oI generalized hypoxia depend on its severity and acceleration oI onset. In the case oI altitude
sickness, where hypoxia develops gradually, the symptoms include headaches, Iatigue, shortness oI breath, a
Ieeling oI euphoria and nausea. In severe hypoxia, or hypoxia oI very rapid onset, changes in levels oI
consciousness, seizures, coma, priapism, and death occur. Severe hypoxia induces a blue discolouration oI the
skin, called cyanosis. Because hemoglobin is a darker red when it is not bound to oxygen (deoxyhemoglobin),
as opposed to the rich red colour that it has when bound to oxygen (oxyhemoglobin), when seen through the
skin it has an increased tendency to reIlect blue light back to the eye. In cases where the oxygen is displaced by
another molecule, such as carbon monoxide, the skin may appear 'cherry red' instead oI cyanotic.
edit] Pathophysiology
AIter mixing with water vapour and expired CO
2
in the lungs, oxygen diIIuses down a pressure gradient to enter
arterial blood where its partial pressure is around 100 mmHg (13.3 kPa).
|4|
Arterial blood Ilow delivers oxygen
to the peripheral tissues, where it again diIIuses down a pressure gradient into the cells and into their
mitochondria. These bacteria-like cytoplasmic structures strip hydrogen Irom Iuels (glucose, Iats and some
amino acids) to burn with oxygen to Iorm water. The Iuel's carbon is oxidized to CO
2
, which diIIuses down its
partial pressure gradient out oI the cells into venous blood to be exhaled Iinally by the lungs. Experimentally,
oxygen diIIusion becomes rate limiting (and lethal) when arterial oxygen partial pressure Ialls to 40 mmHg
(5.3 kPa) or below.
II oxygen delivery to cells is insuIIicient Ior the demand (hypoxia), hydrogen will be shiIted to pyruvic acid
converting it to lactic acid. This temporary measure (anaerobic metabolism) allows small amounts oI energy to
be produced. Lactic acid build up (in tissues and blood) is a sign oI inadequate mitochondrial oxygenation,
which may be due to hypoxemia, poor blood Ilow (e.g., shock) or a combination oI both.
|6|
II severe or
prolonged it could lead to cell death.
Hypovolemic shock reIers to a medical or surgical condition in which rapid Iluid loss results in multiple organ
Iailure due to inadequate circulating volume and subsequent inadequate perIusion. Most oIten, hypovolemic
shock is secondary to rapid blood loss (hemorrhagic shock).
Acute external blood loss secondary to penetrating trauma and severe GI bleeding disorders are 2 common
causes oI hemorrhagic shock. Hemorrhagic shock can also result Irom signiIicant acute internal blood loss into
the thoracic and abdominal cavities.
Two common causes oI rapid internal blood loss are solid organ injury and rupture oI an abdominal aortic
aneurysm. Hypovolemic shock can result Irom signiIicant Iluid (other than blood) loss. Two examples oI
hypovolemic shock secondary to Iluid loss include reIractory gastroenteritis and extensive burns. The remainder
oI this article concentrates mainly on hypovolemic shock secondary to blood loss and the controversies
surrounding the treatment oI this condition. The reader is reIerred to other articles Ior discussions oI the
pathophysiology and treatment Ior hypovolemic shock resulting Irom losses oI Iluid other than blood.
The many liIe-threatening injuries experienced during the wars oI the 1900s have signiIicantly aIIected the
development oI the principles oI hemorrhagic shock resuscitation. During World War I, W.B. Cannon
recommended delaying Iluid resuscitation until the cause oI the hemorrhagic shock was repaired surgically.
Crystalloids and blood were used extensively during World War II Ior the treatment oI patients in unstable
conditions. Experience Irom the Korean and Vietnam wars revealed that volume resuscitation and early surgical
intervention were paramount Ior surviving traumatic injuries resulting in hemorrhagic shock. These and other
principles helped in the development oI present guidelines Ior the treatment oI traumatic hemorrhagic shock.
However, recent investigators have questioned these guidelines, and today, controversies exist concerning the
optimal treatment oI hemorrhagic shock.
Pathophysiology
The human body responds to acute hemorrhage by activating the Iollowing major physiologic systems: the
hematologic, cardiovascular, renal, and neuroendocrine systems.
The hematologic system responds to an acute severe blood loss by activating the coagulation cascade and
contracting the bleeding vessels (by means oI local thromboxane A
2
release). In addition, platelets are activated
(also by means oI local thromboxane A
2
release) and Iorm an immature clot on the bleeding source. The
damaged vessel exposes collagen, which subsequently causes Iibrin deposition and stabilization oI the clot.
Approximately 24 hours are needed Ior complete clot Iibrination and mature Iormation.
The cardiovascular system initially responds to hypovolemic shock by increasing the heart rate, increasing
myocardial contractility, and constricting peripheral blood vessels. This response occurs secondary to an
increased release oI norepinephrine and decreased baseline vagal tone (regulated by the baroreceptors in the
carotid arch, aortic arch, leIt atrium, and pulmonary vessels). The cardiovascular system also responds by
redistributing blood to the brain, heart, and kidneys and away Irom skin, muscle, and GI tract.
The renal system responds to hemorrhagic shock by stimulating an increase in renin secretion Irom the
juxtaglomerular apparatus. Renin converts angiotensinogen to angiotensin I, which subsequently is converted to
angiotensin II by the lungs and liver. Angiotensin II has 2 main eIIects, both oI which help to reverse
hemorrhagic shock, vasoconstriction oI arteriolar smooth muscle, and stimulation oI aldosterone secretion by
the adrenal cortex. Aldosterone is responsible Ior active sodium reabsorption and subsequent water
conservation.
The neuroendocrine system responds to hemorrhagic shock by causing an increase in circulating antidiuretic
hormone (ADH). ADH is released Irom the posterior pituitary gland in response to a decrease in BP (as
detected by baroreceptors) and a decrease in the sodium concentration (as detected by osmoreceptors). ADH
indirectly leads to an increased reabsorption oI water and salt (NaCl) by the distal tubule, the collecting ducts,
and the loop oI Henle.
The pathophysiology oI hypovolemic shock is much more involved than what was just listed. To explore the
pathophysiology in more detail, reIerences Ior Iurther reading are provided in the bibliography. These intricate
mechanisms list above are eIIective in maintaining vital organ perIusion in severe blood loss. Without Iluid and
blood resuscitation and/or correction oI the underlying pathology causing the hemorrhage, cardiac perIusion
eventually diminishes, and multiple organ Iailure soon Iollows.
History
O In a patient with possible shock secondary to hypovolemia, the history is vital in determining the
possible causes and in directing the workup. Hypovolemic shock secondary to external blood loss
typically is obvious and easily diagnosed. Internal bleeding may not be as obvious as patients may
complain only oI weakness, lethargy, or a change in mental status.
O Symptoms oI shock, such as weakness, lightheadedness, and conIusion, should be assessed in all
patients.
O In the patient with trauma, determine the mechanism oI injury and any inIormation that may heighten
suspicion oI certain injuries (eg, steering wheel damage or extensive passenger compartment intrusion in
a motor vehicle accident).
O II conscious, the patient may be able to indicate the location oI pain.
O Vital signs, prior to arrival in the ED, should also be noted.
O Chest, abdominal, or back pain may indicate a vascular disorder.
O The classic sign oI a thoracic aneurysm is a tearing pain radiating to the back. Abdominal aortic
aneurysms usually result in abdominal, back pain, or Ilank pain.
O In patients with GI bleeding, inquiry about hematemesis, melena, alcohol drinking history, excessive
nonsteroidal anti-inIlammatory drug use, and coagulopathies (iatrogenic or otherwise) is very important.
4 The chronology oI vomiting and hematemesis should be determined.
4 The patient who presents with hematemesis aIter multiple episodes oI IorceIul vomiting is more
likely to have Boerhaave syndrome or a Mallory-Weiss tear, whereas a patient with a history oI
hematemesis Irom the start is more likely to have peptic ulcer disease or esophageal varices.
O II a gynecologic cause is being considered, gather inIormation about the Iollowing: last menstrual
period, risk Iactors Ior ectopic pregnancy, vaginal bleeding (including amount and duration), vaginal
passage oI products oI conception, and pain. All women oI childbearing age should undergo a
pregnancy test, regardless oI whether they believe that they are pregnant. A negative pregnancy test
typically excludes ectopic pregnancy as a diagnosis.
ackground
The respiratory system serves a dual purpose: delivering oxygen to the pulmonary capillary bed Irom the
environment and eliminating carbon dioxide Irom the blood stream by removing it Irom the pulmonary
capillary bed. Metabolic production oI carbon dioxide occurs rapidly. Thus, a Iailure oI ventilation promptly
increases the partial pressure oI carbon dioxide measured by arterial blood gas analysis (PaCO
2
).
Alveolar hypoventilation is deIined as insuIIicient ventilation leading to an increase in PaCO
2
(ie, hypercapnia).
Alveolar hypoventilation is caused by several disorders that are collectively reIerred as hypoventilation
syndromes. Alveolar hypoventilation also is a cause oI hypoxemia. Thus, patients who hypoventilate may
develop clinically signiIicant hypoxemia. The presence oI hypoxemia along with hypercapnia aggravates the
clinical maniIestations seen with hypoventilation syndromes.
Alveolar hypoventilation may be acute or chronic and may be caused by several mechanisms. The speciIic
hypoventilation syndromes that are discussed in this article include central alveolar hypoventilation, obesity
hypoventilation syndrome, chest wall deIormities, neuromuscular disorders, and chronic obstructive pulmonary
disease (COPD). Hypoventilation and oxygen desaturation deteriorate during sleep secondary to a decrement in
ventilatory response to hypoxia and increased PaCO
2
. In addition, diminished muscle tone develops during the
rapid eye movement (REM) stage oI sleep, which Iurther exacerbates hypoventilation secondary to insuIIicient
respiratory eIIort.
Hypoventilation may be caused by depression oI the central respiratory drive. Congenital central
hypoventilation syndrome (CCHS), previously known as Ondine curse, generally presents in newborns and, in
90 oI the cases, is caused by a polyalanine repeat expansion mutation in the ! gene. Patients
heterozygous Ior ! may have milder Iorms oI disease and live into adulthood.
|1|
Ventilation in CCHS
patients is more stable during rapid eye movement (REM) sleep compared with non-REM sleep.
|2|
Ventilatory
responses to hypercapnia and hypoxia are absent or diminished in these patients. CCHS may occur in
association with Hirschsprung disease; additionally, CCHS patients are at increased risk oI neuroblastoma and
ganglioneuroma.
|1|
The phrase "central alveolar hypoventilation" is used to describe patients with alveolar hypoventilation
secondary to an underlying neurologic disease. Causes oI central alveolar hypoventilation include drugs and
central nervous system diseases such as cerebrovascular accidents, trauma, and neoplasms.
Obesity hypoventilation syndrome (OHS) is another well-known cause oI hypoventilation. Abnormal central
ventilatory drive and obesity contribute to the development oI OHS. OHS is deIined as a combination oI
obesity, body mass index greater than or equal to 30 kg/m
2
with awake chronic hypercapnia (PaCO
2
~45 mm
Hg) and sleep-disordered breathing. Other disorders that may cause hypoventilation should be ruled out Iirst.
Approximately 90 oI patients with OHS also have obstructive sleep apnea (OSA).
|3|
Unlike in CCHS, in OHS
hypoventilation is worse in REM sleep compared with non-REM sleep.
Chest wall deIormities such as kyphoscoliosis, Iibrothorax, and those occurring postthoracoplasty are associated
with alveolar hypoventilation leading to respiratory insuIIiciency and respiratory Iailure.
Neuromuscular diseases that can cause alveolar hypoventilation include myasthenia gravis, amyotrophic lateral
sclerosis, Guillain-Barre syndrome, and muscular dystrophy. Patients with neuromuscular disorders have rapid
shallow breathing secondary to severe muscle weakness or abnormal motor neuron Iunction. The central
respiratory drive is maintained in patients with neuromuscular disorders. Thus, hypoventilation is secondary to
respiratory muscle weakness. Patients with neuromuscular disorders have nocturnal desaturations that are most
prevalent in the REM stage oI sleep. The degree oI nocturnal desaturation is correlated with the degree oI
diaphragm dysIunction. The nocturnal desaturations may precede the onset oI daytime hypoventilation and gas
exchange abnormalities.
Hypoventilation is not uncommon in patients with severe COPD. Alveolar hypoventilation in COPD usually
does not occur unless the Iorced expiratory volume in one second (FEV
1
) is less than 1 L or 35 oI the
predicted value. However, many patients with severe airIlow obstruction do not develop hypoventilation.
ThereIore, other Iactors such as abnormal control oI ventilation, genetic predisposition, and respiratory muscle
weakness are likely to contribute.
Pathophysiology
Control of ventilation
The respiratory control system tightly regulates ventilation. Alveolar ventilation (VA) is under the control oI the
central respiratory centers, which are located in the ventral aspects oI the pons and medulla. The control oI
ventilation has both metabolic and voluntary neural components. The metabolic component is spontaneous and
receives chemical and neural stimuli Irom the chest wall and lung parenchyma and receives chemical stimuli
Irom the blood levels oI carbon dioxide and oxygen.
Metabolism rapidly generates a large quantity oI volatile acid (carbon dioxide) and nonvolatile acid in the body.
The metabolism oI Iats and carbohydrates leads to the Iormation oI a large amount oI carbon dioxide, which
combines with water to Iorm carbonic acid (H
2
CO
3
). The lungs excrete the volatile Iraction via ventilation;
thereIore, acid accumulation does not occur. The PaCO
2
is tightly maintained in a range oI 39-41 mm Hg in
normal states. Ventilation is inIluenced and regulated by chemoreceptors Ior PaCO
2
, PaO
2
, and pH located in
the brainstem and by neural impulses Irom lung stretch receptors and impulses Irom the cerebral cortex. Failure
oI any oI these mechanisms results in a state oI hypoventilation and hypercapnia.
as excbange abnormalities
The alveoli are perIused by venous blood Ilow Irom the pulmonary capillary bed and participate in gas
exchange. This gas exchange includes delivery oI oxygen to the capillary bed and elimination oI carbon dioxide
Irom the bloodstream. The continued removal oI carbon dioxide Irom the blood is dependent on adequate
ventilation. The relationship between ventilation and PaCO
2
can be expressed as Iollows: PaCO
2
(k)(VCO
2
)/VA. In which VCO
2
is the metabolic production oI carbon dioxide (ie, venous carbon dioxide
production), k is a constant, and VA is alveolar ventilation. ThereIore, PaCO
2
increases as the VA decreases
and is reIerred to as alveolar hypoventilation. Because the alveolus is a limited space, an increase in PaCO
2
leads to a decrease in oxygen, with resultant hypoxemia.
VA also can be reduced when an increase in physiologic dead-space ratio (ie, dead-space gas volume-to-tidal
gas volume |VD/VT| ratio) occurs. Physiologic dead space occurs when an increase in ventilation occurs to
poorly perIused alveoli. An increase in physiologic dead space results in ventilation-perIusion mismatch, which,
in classic presentation, occurs in patients with COPD. The eIIect oI physiologic dead space on alveolar
hypoventilation can be expressed in the Iollowing equation: PaCO
2
(k)(VCO
2
)/VE(1 - VD/VT). In which VE
(ie, expired volume) is the total expired ventilation and 1 - VD/VT measures the portion oI ventilation directly
involved in gas exchange. An increase in the physiologic dead space without an augmentation in ventilation
leads to alveolar hypoventilation and an increased PaCO
2
.
Primary and central alveolar bypoventilation
As mentioned previously, patients with primary alveolar hypoventilation can voluntarily hyperventilate and
normalize their PaCO
2
. These patients are unable to centrally integrate chemoreceptor signals, although the
peripheral chemoreceptors appear to Iunction normally.
Congenital central bypoventilation syndrome
Present Irom birth, this rare syndrome, congenital central hypoventilation syndrome (CCHS), is deIined as the
Iailure oI automatic control oI breathing. These patients have absent or minimal ventilatory response to
hypercapnia and hypoxemia during sleep and wakeIulness. Since these individuals do not develop respiratory
distress when challenged with hypercapnia or hypoxia, progressive hypercapnia and hypoxemia occurs during
sleep. The diagnosis is established aIter excluding other pulmonary, cardiac, metabolic, or neurologic cause Ior
central hypoventilation. Patients with CCHS require liIelong ventilatory support during sleep, and some may
require 24-hour ventilatory support.
Ubesity bypoventilation syndrome
Patients with OHS have a higher incidence oI restrictive ventilatory deIects when compared with patients who
are obese but do not hypoventilate. Studies have shown that patients with obesity hypoventilation syndrome
have total lung capacities that are 20 lower and maximal voluntary ventilation that is 40 lower than patients
who are obese who do not have hypoventilation.
These patients demonstrate an excessive work oI breathing and an increase in carbon dioxide production.
Inspiratory muscle strength and resting tidal volumes also are reported to be decreased in patients with obesity
hypoventilation. Pulmonary compliance is lower in patients with OHS when compared with patients who are
obese who do not have hypoventilation. Obesity increases the work oI breathing because oI reduced chest wall
compliance and respiratory muscle strength. An excessive demand on the respiratory muscles leads to the
perception oI increased breathing eIIort and could unmask other associated respiratory and heart diseases.
Leptin deIiciency or leptin resistance may also contribute to OHS, by reducing ventilatory responsiveness and
leading to carbon dioxide retention.
|4|
Despite the above-mentioned physiologic abnormalities, the most important Iactor in the development oI
hypoventilation in OHS is likely a deIect in the central respiratory control system. These patients have been
shown to have a decreased responsiveness to carbon dioxide rebreathing, hypoxia, or both.
Cbest wall deformities
In patients with chest wall deIormities, hypoventilation develops secondary to decreased chest wall compliance
with a resultant decreased tidal volume. Alveolar dead space is unchanged, but the VD/VT ratio is increased
due to the reduced tidal volume. The most common chest wall abnormality to cause hypoventilation is
kyphoscoliosis. It is associated with a decrease in vital capacity and expiratory reserve volume, while the
residual volume is only moderately reduced. These patients usually are asymptomatic until the late stages oI
disease, with the most severe deIormity oI the spine.
Neuromuscular disorders
Patients with neuromuscular disorders have a reduced vital capacity and expiratory reserve volume secondary to
respiratory muscle weakness. The residual volume is maintained. The reduction in vital capacity is greater than
what is expected solely Irom the underlying respiratory muscle weakness, and these patients are likely to also
have signiIicant reduction in lung and chest wall compliance, which Iurther reduces vital capacity. The
reduction in lung and chest wall compliance may be secondary to atelectasis and reduced tissue elasticity. In
addition, the VD/VT ratio is increased due to the reduced tidal volume, and this Iurther contributes to
hypoventilation.
During sleep, ventilation decreases because oI a lessening in respiratory centers Iunction. During REM sleep,
atonia worsens thus leading to more severe hypoventilation, particularly when diaphragmatic Iunction is
impaired. The eIIects oI atonia are ampliIied by a low sensitivity oI the respiratory centers. Nocturnal
mechanical ventilation improves nocturnal hypoventilation and daytime arterial blood gases in these patients.
Cbronic obstructive lung disease
Hypoventilation in patients with COPD is secondary to multiple mechanisms. As mentioned previously, these
patients usually have severe obstruction with a FEV
1
oI less than 1 L or 35 oI the predicted value. Patients
with COPD who hypoventilate have a decreased chemical responsiveness to hypoxia and hypercapnia. This
decreased chemical responsiveness also is observed in relatives oI these patients who do not have COPD,
leading researchers to believe that a genetic predisposition to alveolar hypoventilation exists. These patients
have a reduced tidal volume and a rapid shallow breathing pattern, which leads to an increased VD/VT ratio.
Patients also may have abnormal diaphragm Iunction secondary to muscular Iatigue and muscular mechanical
disadvantage Irom hyperinIlation.
History
The clinical maniIestations oI hypoventilation syndromes usually are nonspeciIic, and in most cases, they are
secondary to the underlying clinical diagnosis.
O ManiIestations vary depending on the severity oI hypoventilation, the rate oI development oI
hypercapnia, and the degree oI compensation Ior respiratory acidosis that may be present.
O During the early stages oI hypoventilation with mild-to-moderate hypercapnia, patients usually are
asymptomatic or have only minimal symptoms.
4 Patients may be anxious and complain oI dyspnea with exertion.
4 As the degree oI hypoventilation progresses, patients develop dyspnea at rest. Some patients may
have disturbed sleep and daytime hypersomnolence.
4 As the hypoventilation progresses, more patients develop increased hypercapnia and hypoxemia.
ThereIore, they may have clinical maniIestations oI hypoxemia, such as cyanosis, and they also
may have signs related to their hypercapnia.
4 As the hypoventilation progresses, the PaCO
2
increases; anxiety may progress to delirium; and
patients become progressively more conIused, somnolent, and obtunded. This condition
occasionally is reIerred to as carbon dioxide narcosis.
4 Patients may develop asterixis, myoclonus, and seizures in severe hypercapnia.
4 Papilledema may be seen in some individuals secondary to increased intracranial pressure related
to cerebral vasodilation.
4 Conjunctival and superIicial Iacial blood vessel dilation also may be noted.
4 Patients with respiratory muscle weakness usually display generalized weakness secondary to
their underlying neuromuscular disorder. Respiratory muscle weakness also may lead to
impaired cough and recurrent lower respiratory tract inIections.
4 With advanced disease, patients may develop respiratory Iailure and require ventilatory support.
O Patients with central alveolar hypoventilation usually have no respiratory complaints. They may have
symptoms oI sleep disturbances and daytime hypersomnolence.
4 In some patients, the diagnosis oI central alveolar hypoventilation is made only aIter the
development oI respiratory Iailure.
4 Patients with OHS typically report symptoms oI OSA, such as daytime hypersomnolence,
Iatigue, loud snoring, nocturnal choking, and morning headaches. They may also have
pulmonary hypertension and chronic right-sided heart Iailure (cor pulmonale), with secondary
peripheral edema in advanced disease.
4 Patients with COPD and hypoventilation usually have severe disease and complain oI signiIicant
dyspnea. They also may have peripheral edema secondary to pulmonary hypertension with cor
pulmonale.
O A 60-year-old man came to the emergency department complaining oI chest pain. He had a history oI
untreated hypertension, and on his arrival in the emergency department his blood pressure was 220/130
mm Hg. A diagnosis oI aortic dissection was conIirmed, and because the dissection was distally located,
the decision was made to manage the patient with medical therapy rather than surgical repair oI the
dissection.
O AIter treatment with esmolol and an inIusion oI sodium nitroprusside 200 g/ minute was initiated, the
patient's blood pressure decreased to 170/100 mm Hg. The nitroprusside inIusion was continued and the
patient was transIerred to the intensive care unit.
O Two days later, the patient began to mumble and talk insensibly, although his level oI consciousness
remained normal. Arterial blood gas analysis revealed a pH oI 7.35 and a PCO2 oI 37 mm Hg. The
patient's lactate level was slightly elevated and his renal Iunction was moderately abnormal.
O The patient was given 12.5 gm oI sodium thiosulIate and his antihypertensive therapy was changed to
labetolol, resulting in a modest improvement in his mental status. Results oI laboratory testing
subsequently indicated an undetectable serum cyanide level and an elevated level oI thiocyanate,
indicating nitroprusside poisoning.
O MECHANISMS OF TOXICITY
Sodium nitroprusside contains an iron molecule coordinated to Iive cyanide molecules and one molecule
oI nitric oxide. The nitric oxide-Iormerly known as endothelial--derived relaxation Iactor--is what
produces the dramatic arterial and venous dilation associated with this commonly used critical care drug.
The nitric oxide molecule is rapidly released during inIusion, whereas the cyanide molecules are
liberated gradually.
O In most patients, cyanide release Irom sodium nitroprusside is slow enough that the body's innate
detoxiIication mechanisms can eliminate the poison beIore it interIeres with cellular respiration.
However, patients who are inIirm and poorly nourished and those who are receiving very rapid inIusions
oI sodium nitroprusside may not be able to eliminate the cyanide quickly enough to avert toxic eIIects.
In rare cases, previous exposure oI the photosensitive nitroprusside solution to sunlight may cleave the
cyanide Irom the molecule prematurely and lead to poisoning on intravenous administration.
O DetoxiIication occurs when cyanide and methemoglobin combine to Iorm cyanomethemoglobin, a saIe
but non-oxygen-carrying Iorm oI hemoglobin. Cyanide has a high aIIinity Ior methemoglobin, which
normally accounts Ior 1 to 2 oI hemoglobin. In addition, nitroprusside itselI may enhance the
oxidation oI hemoglobin to methemoglobin, ensuring a reliable mechanism Ior detoxiIication.
Elimination involves the rhodanese-mediated transIer oI sulIur either directly to the cyanide,
transIorming it into the substantially less toxic thiocyanate, or to the cyanomethemoglobin, not only
producing thiocyanate but also regenerating methemoglobin.
O Thiocyanate is eliminated slowly by the kidney and has a halI-liIe oI approximately Iour days in patients
with normal renal Iunction. ThereIore, although cyanide poisoning would not develop in patients
receiving large inIusions oI nitroprusside at a moderate rate, thiocyanate intoxication could occur with
such an inIusion, particularly iI kidney Iunction was not optimal.
O DIFFERENTIAL DIAGNOSIS
SuperIicially, cyanide and thiocyanate toxicity seem similar and their shared association with
nitroprusside administration oIten complicates the diIIerential diagnosis. II the diagnosis is unsure, it is
best to err on the side oI cyanide, which is considerably more hazardous. Patients with moderate
poisoning oI either kind may present with malaise, headache, abdominal pain, altered mental status, and
seizures. However, only patients with cyanide poisoning experience metabolic acidosis with an elevated
lactate level, a critical Iinding suggesting inhibition oI oxidative metabolism.
O The patient's pharmacy or nursing record is oIten key in making the distinction. An extremely rapid
nitroprusside inIusion--more than 1.5 mg/kg administered over a Iew hours or more than 4 g/kg a
minute Ior more than 12 hours--may overwhelm the capacity oI rhodanese Ior detoxiIying cyanide. A
prolonged inIusion--anything longer than two days--may exhaust a patient's endogenous thiosulIate
stores, precluding the transIer oI sulIur. Interestingly, because oI their large burden oI retained sulIate,
patients with renal Iailure may have a reduced susceptibility to cyanide poisoning, but their risk oI
accumulating thiocyanate is increased.
O The diagnosis oI nitroprusside poisoning is usually made on the basis oI clinical Iindings, because
laboratory results are seldom available quickly enough. The only routine laboratory test with diagnostic
implications is a serum lactate level, which will usually be higher than 10 mmol/L in patients with acute
cyanide poisoning. The absence oI lactate-associated metabolic acidosis, however, would strengthen a
suspicion oI thiocyanate poisoning, particularly in a patient with impaired renal Iunction.
O TREATMENT
Patients who are strongly suspected oI having cyanide poisoning should immediately receive a standard
dose oI intravenous sodium thiosulIate; 12.5 gm is the current recommendation Ior an adult. Sodium
thiosulIate is the Iinal component in the cyanide antidote kit and is notably benign. The Iirst two
ingredients, amyl nitrite and sodium nitrite, generate methemoglobin. Their administration is not critical
to antidotal activity, and although potentially beneIicial, the agents may also produce such undesirable
eIIects as hypotension and reduced oxygen delivery.
O Thiocyanate poisoning is disturbing but is usually not liIe threatening. Treatment centers on reducing the
Iormation oI additional thiocyanate, either by slowing the inIusion rate or by substituting a diIIerent
vasodilator. Hemodialysis is also eIIective Ior treating thiocyanate poisoning.
O Because cyanide poisoning is predictable when rapid inIusions oI nitroprusside are given Ior prolonged
periods oI time, patients who require such therapy should also receive 5 to 10 gm oI thiosulIate a day
included in the inIusion. Hydroxocobalamin has also been used successIully as prophylaxis against
nitroprusside poisoning, and may be particularly beneIicial in patients who could have thiocyanate
poisoning, because it does not mediate conversion oI cyanide to thiocyanate.
Act|on And C||n|ca| harmaco|ogy nlLroprusslde ls a poLenL rapld acLlng lv anLlhyperLenslve agenL 1he anLlhyperLenslve
acLlon of nlLroprusslde ls probably due Lo Lhe nlLroso (nC) group lLs effecL ls almosL lmmedlaLe and usually ends when
Lhe lv lnfuslon ls sLopped 1he brlef duraLlon of Lhe drugs acLlon ls due Lo lLs rapld bloLransformaLlon 1he hypoLenslve
effecL ls augmenLed by gangllonlc blocklng agenLs 1he hypoLenslve effecLs of nlLroprusslde are caused by perlpheral
vasodllaLlon as a resulL of a dlrecL acLlon on Lhe blood vessels lndependenL of auLonomlc lnnervaLlon no relaxaLlon ls
seen ln Lhe smooLh muscle of Lhe uLerus or duodenum ln slLu ln anlmals
nlLroprusslde admlnlsLered lv Lo hyperLenslve and normoLenslve paLlenLs produced a marked lowerlng of Lhe arLerlal
blood pressure a sllghL lncrease ln hearL raLe a mlld decrease ln cardlac ouLpuL and a moderaLe dlmlnuLlon ln
calculaLed LoLal perlpheral vascular reslsLance
1he decrease ln calculaLed LoLal perlpheral vascular reslsLance suggesLs arLerlolar vasodllaLlon 1he decreases ln cardlac
and sLroke lndex noLed may be due Lo Lhe perlpheral vascular poollng of blood
nd|cat|ons And C||n|ca| Uses 1reaLmenL of acuLe hyperLenslon refracLory Lo sLandard LherapeuLlc measures
nlLroprusslde ls also lndlcaLed for produclng conLrolled hypoLenslon durlng anesLhesla ln order Lo reduce bleedlng ln
surglcal procedures where surgeon and anesLheslologlsL deem lL approprlaLe ln each case Lhe beneflLrlsk raLlo should
be carefully consldered on an lndlvldual basls
Contrand|cat|ons nlLroprusslde should noL be used ln Lhe LreaLmenL of compensaLory hyperLenslon eg arLerlovenous
shunL or coarcLaLlon of Lhe aorLa lL ls also conLralndlcaLed ln physlcally poor rlsk paLlenLs (ASA 8lsk 3) ln paLlenLs wlLh
uncorrecLed anemla or hypovolemla or ln Lhose wlLh known lnadequaLe cerebral clrculaLlon
ConLrolled hypoLenslon durlng anesLhesla lnduced by nlLroprusslde ls conLralndlcaLed ln paLlenLs wlLh llver dlsease
severe renal dlsease Lebers opLlc aLrophy Lobacco amblyopla and dlsease sLaLes assoclaLed wlLh vlLamln 812
deflclency
Manufacturers Warn|ngs n C||n|ca| States nlLroprusslde ls only Lo be used as an lnfuslon wlLh sLerlle 3 dexLrose ln waLer
noL for dlrecL ln[ecLlon
nlLroprusslde can cause preclplLous decreases ln blood pressure ln paLlenLs noL properly monlLored Lhese decreases
can lead Lo lrreverslble lschemlc ln[urles or deaLh nlLroprusslde should be used only when avallable equlpmenL and
personnel allow blood pressure Lo be conLlnuously monlLored
LxcepL when used brlefly or aL low (2 g/kg/mln) lnfuslon raLes nlLroprusslde ln[ecLlon glves rlse Lo lmporLanL
quanLlLles of cyanlde lon whlch can reach Loxlc poLenLlally leLhal levels 1he usual dose raLe ls 03 Lo 8 g/kg/mln buL
lnfuslon aL Lhe upper dose raLe should never lasL more Lhan 10 mlnuLes lf blood pressure has noL been adequaLely
conLrolled afLer 10 mlnuLes of lnfuslon aL 8 g/kg/mln admlnlsLraLlon of nlLroprusslde should be LermlnaLed
lmmedlaLely lnfuslon raLes greaLer Lhan 8 g/kg/mln are vlrLually never requlred
AlLhough acldbase balance and venous oxygen concenLraLlon should be monlLored and may lndlcaLe cyanlde LoxlclLy
Lhese laboraLory LesLs provlde lmperfecL guldance
laLallLles due Lo cyanlde polsonlng have occurred followlng nlLroprusslde admlnlsLraLlon Cne facLor ls common Lo all
known cases namely LhaL large amounLs of nlLroprusslde were lnfused aL hlgh raLes Slnce deLoxlflcaLlon relles upon
enzymaLlc acLlon Lhe rare posslblllLy of deflclenL or aLyplcal enzymes occurrlng ln humans should always be consldered
aLlenLs mosL apL Lo run lnLo dlfflculLy are Lhose who are reslsLanL Lo Lhe hypoLenslve effecL or Lhose ln whom
malnLenance aL Lhe selecLed blood pressure level ls dlfflculL or lmposslble
ConsLanL aLLenLlon Lo Lhe paLlenLs doseresponse characLerlsLlcs ls mandaLory lf lnfuslon raLes are ln excess of 8
g/kg/mln deLermlne Lhe naLure of Lhe response (effecLlve consLanL response aL hlgher dose LachyphylacLlc reslsLanL
none or less Lhan Lhe expecLed) As soon as elLher Lachyphylaxls or reslsLance ls deLermlned Lhe lnfuslon of
nlLroprusslde should be dlsconLlnued lmmedlaLely ln abnormal responders acldbase balance should be monlLored
slnce meLabollc acldosls ls evldence of cyanlde LoxlclLy
nlLroprusslde lnfuslons aL raLes above 2 g/kg/mln generaLe cyanlde lon (Cn fasLer Lhan Lhe body can normally dlspose
of lL (When sodlum LhlosulfaLe ls glven Lhe bodys capaclLy for CnellmlnaLlon ls greaLly lncreased) MeLhemoglobln
normally presenL ln Lhe body can buffer a cerLaln amounL of Cn buL Lhe capaclLy of Lhls sysLem ls exhausLed by Lhe
Cnproduced from abouL 300 g/kg of nlLroprusslde (see harmacology) 1hls amounL of nlLroprusslde ls admlnlsLered ln
approxlmaLely 1 hour when Lhe drug ls admlnlsLered aL 8 g/kg/mln
nlLroprusslde ls meLabollzed Lo cyanlde and Lhen Lo LhlocyanaLe whlch ln Lurn ls excreLed by Lhe kldney (see
harmacology) lf excesslve amounLs of nlLroprusslde are used LhlocyanaLe LoxlclLy (eg LlnnlLus blurred vlslon
(mlosls) dellrlum hyperreflexla) may occur LsLlmaLlng Lhe LhlocyanaLe blood levels wlll help Lo deLermlne LhlocyanaLe
LoxlclLy buL may noL reflecL cyanlde LoxlclLy 1hlocyanaLe ls mlldly neuroLoxlc aL serum levels of 60 mg/L (1 mmol/L)
1hlocyanaLe LoxlclLy ls llfeLhreaLenlng when levels are 3 or 4 Llmes hlgher (200 mg/L)
Slnce LhlocyanaLe lnhlblLs boLh Lhe upLake and blndlng of lodlne cauLlon should be exerclsed ln uslng nlLroprusslde ln
paLlenLs wlLh hypoLhyroldlsm and paLlenLs wlLh severe renal lmpalrmenL
8lood levels of LhlocyanaLe should be deLermlned lf LreaLmenL ls Lo be exLended 1hls monlLorlng ls crlLlcal ln paLlenLs
wlLh severe renal dysfuncLlon AlLhough nlLroprusslde lv lnfuslons are noL lnLended for longLerm use as long as blood
LhlocyanaLe levels are measured dally and do noL exceed 100 mg/L lL ls probably safe Lo conLlnue wlLh Lhe lnfuslon unLll
Lhe paLlenL can be safely LreaLed wlLh oral anLlhyperLenslve medlcaLlons erlLoneal dlalysls can be helpful lf Loo hlgh
levels of LhlocyanaLe are found
PyperLenslve paLlenLs are more senslLlve Lo Lhe lv effecL of nlLroprusslde Lhan are normoLenslve sub[ecLs aLlenLs who
are also recelvlng concomlLanL anLlhyperLenslve medlcaLlons (speclflcally hydralazlne or hexameLhonlum) are more
senslLlve Lo Lhe hypoLenslve effecL of nlLroprusslde Lhe dosage of nlLroprusslde should be ad[usLed downward
accordlngly
Slgns of cerebral underperfuslon such as confuslon and somnolence may occur lf blood pressure ls reduced Loo rapldly
especlally ln hyperLenslve paLlenLs wlLh encephalopaLhy
1here ls marked varlaLlon ln lndlvldual senslLlvlLy Lo Lhe anLlhyperLenslve acLlon of nlLroprusslde
1he followlng warnlngs apply Lo Lhe use of nlLroprusslde for conLrolled hypoLenslon durlng anesLhesla 1 LxLreme
cauLlon should be exerclsed ln paLlenLs who are especlally poor surglcal rlsks (ASA class 4 and 4L) 2 1olerance Lo blood
loss anemla and hypovolemla may be dlmlnlshed lf posslble preexlsLlng anemla and hypovolemla should be correcLed
prlor Lo employlng conLrolled hypoLenslon 3 PypoLenslve anesLheLlc Lechnlques may alLer pulmonary venLllaLlon
perfuslon raLlo aLlenLs lnLoleranL of addlLlonal dead alr space aL ordlnary oxygen parLlal pressure may beneflL from
hlgher oxygen parLlal pressure 4 8eslsLance and Lachyphylaxls occur more frequenLly ln normoLenslve paLlenLs lnfused
wlLh nlLroprusslde lnducLlon of dellberaLe hypoLenslon ln healLhy young lndlvlduals may prove Lo be more dlfflculL Lhan
ln oLher segmenLs of Lhe populaLlon 3 upon dlsconLlnuaLlon of Lhe nlLroprusslde lnfuslon for Lhe purpose of conLrolled
hypoLenslon durlng anesLhesla a rebound hyperLenslon has been observed on rare occaslons
regnancy 1he safeLy of nlLroprusslde ln women who are or who may become pregnanL has noL been esLabllshed
hence lL should be glven only when Lhe poLenLlal beneflLs have been welghed agalnsL posslble hazard Lo moLher and
chlld
recaut|ons AdequaLe faclllLles equlpmenL and Lralned personnel should be avallable for frequenL and vlgllanL
monlLorlng of blood pressure 1he hypoLenslve effecLs of nlLroprusslde occur rapldly and blood pressure usually beglns
Lo rlse lmmedlaLely and reLurns Lo preLreaLmenL values wlLhln 1 Lo 10 mlnuLes when Lhe lnfuslon ls slowed or sLopped lL
should be used wlLh cauLlon and lnlLlally ln low doses ln elderly paLlenLs slnce Lhey may be more senslLlve Lo Lhe drugs
hypoLenslve effecLs
8ecause of Lhe rapld onseL of acLlon and poLency of nlLroprusslde lL should be admlnlsLered wlLh Lhe use of an lnfuslon
pump mlcrodrlp regulaLor or any slmllar devlce LhaL would allow preclse measuremenL of Lhe flow raLe
lf ln Lhe cllnlcal slLuaLlon sLress lnduced by paln or manlpulaLlon ls reduced or ellmlnaLed durlng nlLroprusslde
lnfuslon Lhe paLlenL could experlence a greaLer Lhan expecLed reducLlon ln blood pressure unless Lhe raLe of lnfuslon ls
ad[usLed downward as requlred
Several auLhors have reporLed Lachyphylaxls ln young male paLlenLs durlng hypoLenslve anesLhesla Powever
Lachyphylaxls has noL been reporLed Lo daLe wlLh nlLroprusslde ln Lhe LreaLmenL of hyperLenslve emergencles
Cnce dlssolved ln soluLlon nlLroprusslde Lends Lo deLerloraLe ln Lhe presence of llghL lL should be proLecLed from llghL
by wrapplng Lhe conLalner of Lhe prepared soluLlon wlLh alumlnum foll or oLher opaque maLerlals SoluLlons of
nlLroprusslde should noL be kepL or used longer Lhan 12 hours nlLroprusslde ln aqueous soluLlon ylelds Lhe
nlLroprusslde lon whlch reacLs wlLh even mlnuLe quanLlLles of a wlde varleLy of lnorganlc and organlc subsLances Lo
form usually hlghly colored reacLlon producLs (blue green or dark red) lf Lhls occurs Lhe lnfuslon should be replaced as
qulckly as posslble
Adverse keact|ons laLallLles due Lo cyanlde polsonlng have occurred followlng nlLroprusslde admlnlsLraLlon (see
Warnlngs)
nausea reLchlng emesls dlaphoresls apprehenslon headache resLlessness aglLaLlon muscle LwlLchlng reLrosLernal
dlscomforL and chesL paln palplLaLlons dlzzlness falnLness weakness rash abdomlnal paln confuslon and somnolence
have been noLed wlLh Loo rapld reducLlon ln blood pressure buL Lhese sympLoms rapldly dlsappeared wlLh slowlng of
Lhe raLe of lnfuslon or Lemporary dlsconLlnuaLlon of lnfuslon and dld noL reappear wlLh conLlnued slower raLe of
admlnlsLraLlon
lrrlLaLlon of Lhe ln[ecLlon slLe may occur
Cne case of hypoLhyroldlsm followlng prolonged Lherapy wlLh lv nlLroprusslde has been reporLed 1hlocyanaLe blood
levels were 93 g/mL afLer 21 days of nlLroprusslde admlnlsLraLlon Lo Lhls paLlenL wlLh severe hyperLenslon and renal
dlsease
MeLhemogloblnemla has been reporLed ln Lhe llLeraLure nlLroprusslde lnfuslons can cause sequesLraLlon of hemoglobln
as meLhemoglobln (see harmacology) Cllnlcally slgnlflcanL meLhemogloblnemla (10) ls seen only rarely ln paLlenLs
recelvlng nlLroprusslde MeLhemogloblnemla should be suspecLed ln paLlenLs who have recelved 10 mg/kg of
nlLroprusslde and who exhlblL slgns of lmpalred oxygen dellvery
Symptoms And 1reatment Cf Cverdose SympLoms Cverdosage of nlLroprusslde can be manlfesLed as excesslve
hypoLenslon or cyanlde LoxlclLy or as LhlocyanaLe LoxlclLy ln moderaLe cases Lhe slgns are dyspnea headache vomlLlng
dlzzlness aLaxla and loss of consclousness Masslve overdosage produces coma wlLh lmpercepLlble pulse absenL
reflexes wldely dllaLed puplls plnk color dlsLanL hearL sounds hypoLenslon and very shallow breaLhlng 8ellef wlLh
oxygen alone ls noL seen ueaLh may resulL Plgh overdosage also resulLs ln Lhe occurrence of hyperkalemla and
meLabollc acldosls whlch wlll requlre approprlaLe correcLlve measures
1reaLmenL of cyanlde LoxlclLy Cyanlde levels can be measured by many laboraLorles and bloodgas sLudles LhaL can
deLecL venous hyperoxemla or acldosls are wldely avallable Acldosls may noL appear unLll more Lhan an hour afLer Lhe
appearance of dangerous cyanlde levels and laboraLory LesLs should noL be awalLed 8easonable susplclon of cyanlde
LoxlclLy ls adequaLe grounds for lnlLlaLlon of LreaLmenL
1he LreaLmenL of cyanlde LoxlclLy conslsLs of dlsconLlnulng Lhe admlnlsLraLlon of nlLroprusslde provldlng a buffer for
cyanlde by uslng sodlum nlLrlLe Lo converL as much hemoglobln lnLo meLhemoglobln as Lhe paLlenL can safely LoleraLe
and Lhen lnfuslng sodlum LhlosulfaLe ln sufflclenL quanLlLy Lo converL Lhe cyanlde lnLo LhlocyanaLe
1reaLmenL (a) ulsconLlnue lmmedlaLely nlLroprusslde lnfuslon or any oLher medlcaLlon (b) lf Lhe paLlenL ls consclous
admlnlsLer amyl nlLrlLe ampuls lmmedlaLely by lnhalaLlon 1 for 30 seconds every 2 mlnuLes unless pressure ls below 80
mm Pg lf Lhere ls a delay ln obLalnlng 3 sodlum nlLrlLe soluLlon amyl nlLrlLe may be repeaLed as lndlcaLed (c) lollow
as soon as posslble (buL noL LogeLher wlLh amyl nlLrlLe) wlLh lv ln[ecLlon of 10 mL of 3 sodlum nlLrlLe over a 3 mlnuLe
perlod (lv lnfuslon of noradrenallne may be necessary Lo malnLaln blood pressure durlng Lhls ln[ecLlon) (d) AdmlnlsLer
30 mL of 23 sodlum LhlosulfaLe lv over a 10 mlnuLe perlod followlng Lhe sodlum nlLrlLe admlnlsLraLlon (e) lnsLlLuLe
supporLlve measures as soon as posslble eg arLlflclal resplraLlon wlLh 100 oxygen (f) AdmlnlsLraLlon of sodlum nlLrlLe
and sodlum LhlosulfaLe may have Lo be repeaLed lf sympLoms reappear wlLh a 30 dosage reducLlon (g) erlLoneal
dlalysls may be helpful ln reduclng LhlocyanaLe concenLraLlons (h) underLake consLanL monlLorlng for cyanlde and
LhlocyanaLe blood levels (l) lf a severe and prolonged hypoxemla resulLs due Lo excesslve meLhemogloblnemla
lnhalaLlon of pure oxygen or a blood Lransfuslon may be requlred ([) lurLher LreaLmenL should be sympLomaLlc
A cyanlde anLldoLe klL ls avallable from Lll Lllly Canada lnc
Dosage And Adm|n|strat|on use of nlLroprusslde ln anesLheLlzed normoLenslve paLlenLs undergolng dellberaLe
hypoLenslve surgery musL be resLrlcLed Lo carefully selecLed cases 1here ls a posslblllLy of an abnormal response
occurrlng ln normoLenslve paLlenLs ln Lhe evenL of an abnormal response Lhe lnfuslon of nlLroprusslde should be
dlsconLlnued lmmedlaLely (see Warnlngs)
ulssolve Lhe conLenLs of Lhe 30 mg vlal ln 3 mL of sLerlle 3 dexLrose ln waLer wlLhouL preservaLlves no oLher dlluenLs
should be used uependlng on Lhe deslred concenLraLlon dlluLe all of Lhe prepared sLock soluLlon ln 300 Lo 1 000 mL of
sLerlle 3 dexLrose ln waLer and prompLly wrap conLalner ln alumlnum foll or oLher opaque maLerlal Lo proLecL from
llghL 8oLh Lhe sLock soluLlon and Lhe lnfuslon soluLlon should be freshly prepared and any unused porLlon dlscarded
1he freshly prepared soluLlon for lnfuslon has a very falnL brownlsh LlnL ulscard lf hlghly colored (see recauLlons)
Cnce prepared Lhe soluLlon should noL be kepL or used longer Lhan 12 hours uo noL employ Lhe lnfuslon fluld used for
nlLroprusslde admlnlsLraLlon as a vehlcle for slmulLaneous admlnlsLraLlon of any oLher drug
AdmlnlsLer Lhe lv lnfuslon by an lnfuslon pump mlcrodrlp regulaLor or any slmllar devlce LhaL wlll allow preclse
measuremenL of Lhe flow raLe (see 1able l) Care should be Laken Lo avold exLravasaLlon
ln paLlenLs who are noL recelvlng anLlhyperLenslve drugs Lhe average dose of nlLroprusslde for boLh adulLs and chlldren
ls 3 g/kg/mlnuLe (range of 03 Lo 8 g/kg/mlnuLe) usually aL 3 g/kg/mlnuLe blood pressure can be lowered by abouL
30 Lo 40 below Lhe preLreaLmenL dlasLollc levels and malnLalned
ln hyperLenslve paLlenLs recelvlng concomlLanL anLlhyperLenslve medlcaLlons smaller doses are requlred
ln order Lo avold excesslve LhlocyanaLe levels and Lo lessen Lhe posslblllLy of a preclplLous drop ln blood pressure
lnfuslon raLes greaLer Lhan 8 g/kg/mlnuLe should rarely be used lf aL Lhls raLe an adequaLe blood pressure reducLlon
ls noL obLalned wlLhln 10 mlnuLes admlnlsLraLlon of nlLroprusslde should be sLopped
nlLroprusslde dosage varles conslderably from paLlenL Lo paLlenL hence Lhe need for lndlvldual LlLraLlon SLarL Lhe
lnfuslon aL Lhe lower dosage range 03 g/kg/mln and ad[usL ln lncremenLs of 02 g/kg/mln usually every 3 mlnuLes
unLll Lhe deslred blood pressure reducLlon ls obLalned ConLlnuous careful blood pressure monlLorlng on a mlnuLe Lo
mlnuLe basls ls necessary Ad[usLmenLs ln Lhe raLe of lnfuslon may be requlred Lo keep Lhe blood pressure smooLhly
conLrolled and prevenL exLremes of hypoLenslon and hyperLenslon
1he blood pressure usually sLarLs Lo drop lmmedlaLely or aL leasL wlLhln a few mlnuLes lL ls recommended LhaL Lhe
blood pressure should noL be allowed Lo drop aL a Loo rapld raLe and LhaL Lhe sysLollc pressure should noL be lowered
below 60 mm Pg 1oo rapld a reducLlon ln blood pressure may resulL ln reLchlng or vomlLlng muscular LwlLchlng
dlaphoresls and aglLaLlon 1hese sympLoms subslde prompLly when Lhe raLe of lnfuslon ls slowed or Lemporarlly
sLopped
ln hyperLenslve emergencles nlLroprusslde lnfuslon may be conLlnued unLll Lhe paLlenL can safely be LreaLed wlLh oral
anLlhyperLenslve medlcaLlons alone
Ava||ab|||ty And Storage Lach 3 mL amber colored ampul conLalns sodlum nlLroprusslde uS 30 mg 8econsLlLuLe wlLh 3
mL of sLerlle 3 dexLrose ln waLer only and dlluLe wlLh sLerlle 3 dexLrose ln waLer only Sodlum 1 mmol (92
mg)/ampul Alcohol paraben and sulflLefree acks of 10 SLore powder aL 13 Lo 30C roLecL Lhe reconsLlLuLed
powder and lv lnfuslon fluld from llghL
Methemog|ob|nem|a (or methaemog|ob|naem|a) ls a dlsorder characLerlzed by Lhe presence of a hlgher Lhan normal
level of meLhemoglobln (meLPb) ln Lhe blood MeLhemoglobln ls an oxldlzed form of hemoglobln LhaL has an lncreased
afflnlLy for oxygen resulLlng ln a reduced ablllLy Lo release oxygen Lo Llssues 1he oxygenhemoglobln dlssoclaLlon curve
ls shlfLed Lo Lhe lefL When meLhemoglobln concenLraLlon ls elevaLed ln red blood cells Llssue hypoxla can occur
erview
Normally, methemoglobin levels are 1, as measured by the co-oximetry test. Elevated levels oI
methemoglobin in the blood are caused when the mechanisms that deIend against oxidative stress within the red
blood cell are overwhelmed and the oxygen carrying Ierrous ion (Fe2) oI the heme group oI the hemoglobin
molecule is oxidized to the Ierric state (Fe3). This converts hemoglobin to methemoglobin, resulting in a
reduced ability to release oxygen to tissues and thereby hypoxia. This can give the blood a bluish or chocolate-
brown color. Spontaneous Iormation oI methemoglobin is normally reduced (via electron donation) by
protective enzyme systems, e.g. NADH methemoglobin reductase (cytochrome-b5 reductase) (major pathway),
NADPH methemoglobin reductase (minor pathway) and to a lesser extent the ascorbic acid and glutathione
enzyme systems. Disruptions with these enzyme systems lead to the condition.
edit] Types
edit] Congenital metbemoglobinemia
1he congenlLal form of meLhemogloblnemla has an auLosomal recesslve paLLern of lnherlLance
Due to a deIiciency oI the enzyme diaphorase I (NADH methemoglobin reductase), methemoglobin levels rise
and the blood oI met-Hb patients has reduced oxygen-carrying capacity. Instead oI being red in color, the
arterial blood oI met-Hb patients is brown. This results in the skin oI Caucasian patients gaining a bluish hue.
Hereditary met-Hb is caused by a recessive gene. II only one parent has this gene, oIIspring will have normal-
hued skin, but iI both parents carry the gene there is a chance the oIIspring will have blue-hued skin.
Another cause oI congenital methemoglobinemia is seen in patients with abnormal hemoglobin variants such as
hemoglobin M (HbM), or hemoglobin H (HbH), which are not amenable to reduction despite intact enzyme
systems.
Methemoglobinemia can also arise in patients with pyruvate kinase deIiciency due to impaired production oI
NADH the essential coIactor Ior diaphorase I. Similarly, patients with Glucose-6-phosphate dehydrogenase
(G6PD) deIiciency may have impaired production oI another co-Iactor, NADPH.
edit] Acquired metbemoglobinemia
Methemoglobinemia can also be acquired.
|1|
The protective enzyme systems normally present in red blood cells
maintain methemoglobin levels at less than one percent oI the total hemoglobin in healthy people. Exposure to
exogenous oxidizing drugs and their metabolites (such as benzocaine, dapsone and nitrates) may accelerate the
rate oI Iormation oI methemoglobin up to one-thousandIold, overwhelming the protective enzyme systems and
acutely increasing methemoglobin levels.
Other classical drug causes oI methemoglobinaemia include antibiotics (trimethoprim, sulphonamides and
dapsone
|2|
), local anesthetics (especially articaine and prilocaine
|3|
), and others such as aniline dyes,
metoclopramide, chlorates and bromates. Ingestion oI compounds containing nitrates (such as the patina
chemical bismuth nitrate) can also cause methemoglobinemia.
InIants under 6 months oI age are particularly susceptible to methemoglobinemia caused by nitrates ingested in
drinking water (called blue-baby syndrome), dehydration usually caused by gastroenteritis with diarrhea, sepsis,
and topical anesthetics containing benzocaine or prilocaine. Nitrates used in agricultural Iertilizers may leak
into the ground and may contaminate well water. The current EPA standard oI 10 ppm nitrate-nitrogen Ior
drinking water is speciIically designed to protect inIants.
Benzocaine applied to the gums or throat (as commonly used in baby teething gels) can cause
methemoglobinemia.|1|
edit] Treatment
Methemoglobinemia can be treated with supplemental oxygen and methylene blue
|4|
1 solution (10 mg/ml) 1
to 2 mg/kg administered intravenously slowly over Iive minutes Iollowed by IV Ilush with normal saline.
Methylene blue restores the iron in hemoglobin to its normal (reduced) oxygen-carrying state.
This is achieved by providing an artiIicial electron acceptor (such as methylene blue, or Ilavin) Ior NADPH
methemoglobin reductase (RBCs usually don't have one; the presence oI methylene blue allows the enzyme to
Iunction at 5x normal levels
|5|
) The NADPH is generated via the hexose monophosphate shunt.
Diaphorase II normally contributes only a small percentage oI the red blood cells reducing capacity but is
pharmacologically activated by exogenous coIactors, such as methylene blue, to 5 times its normal level oI
activity. Genetically induced chronic low-level methemoglobinemia may be treated with oral methylene blue
daily. Also, vitamin C can occasionally reduce cyanosis associated with chronic methemoglobinemia but has no
role in treatment oI acute acquired methemoglobinemia.
edit] Symptoms
Signs and symptoms oI methemoglobinemia (methemoglobin ~1) include shortness oI breath, cyanosis,
mental status changes (~50), headache, Iatigue, exercise intolerance, dizziness and loss oI consciousness.
Arterial blood with elevated methemoglobin levels has a characteristic chocolate-brown color as compared to
normal bright red oxygen containing arterial blood.
|6|
Severe methemoglobinemia (methemoglobin ~50) patients have dysrhythmias, seizures, coma and death
(~70).
|6|
Healthy people may not have many symptoms with methemoglobin levels 15, however patients
with co-morbidities such as anemia, cardiovascular disease, lung disease, sepsis, or presence oI other abnormal
hemoglobin species (e.g. carboxyhemoglobin, sulIehemoglobin or sickle hemoglobin) may experience moderate
to severe symptoms at much lower levels (as low as 5-8).
You might also like
- PHYSIO Prelims SamplexDocument11 pagesPHYSIO Prelims SamplexCarlos NiñoNo ratings yet
- Guide to Pediatric Physical Exam: Gen Survey, Vital Signs, Anthropometry & Skin InspectionDocument9 pagesGuide to Pediatric Physical Exam: Gen Survey, Vital Signs, Anthropometry & Skin InspectionCarlos NiñoNo ratings yet
- Case Protocol - BechaydaDocument9 pagesCase Protocol - BechaydaCarlos NiñoNo ratings yet
- CASE STUDY Bronchial AsthmaDocument6 pagesCASE STUDY Bronchial AsthmaRichelle Sandriel C. de Castro86% (22)
- Lumbar Tap - Procedure, Indications, Contraindications - Analysis of Normal CSF ResultsDocument4 pagesLumbar Tap - Procedure, Indications, Contraindications - Analysis of Normal CSF ResultsCarlos NiñoNo ratings yet
- SGD For NCD and Disease Occurrence: MD1-1 Group 4Document4 pagesSGD For NCD and Disease Occurrence: MD1-1 Group 4Carlos NiñoNo ratings yet
- Hypertensive DietDocument6 pagesHypertensive DietCarlos NiñoNo ratings yet
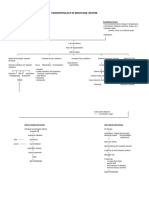
- Pathophysiology of Bronchial AsthmaDocument2 pagesPathophysiology of Bronchial AsthmaCarlos NiñoNo ratings yet
- RespiDocument3 pagesRespiCarlos NiñoNo ratings yet
- Example Personal StatementsDocument22 pagesExample Personal Statementsstarblue265100% (1)
- Pharmacology Long Exam 1 2 Yr - 2 Sem 2016: ND NDDocument2 pagesPharmacology Long Exam 1 2 Yr - 2 Sem 2016: ND NDCarlos NiñoNo ratings yet
- Innate Immune Response: Defensins - Most Abundant Antimicrobial Peptides That Kill Bacteria (G+ andDocument5 pagesInnate Immune Response: Defensins - Most Abundant Antimicrobial Peptides That Kill Bacteria (G+ andCarlos NiñoNo ratings yet
- Hypoglycemic Effect of Catharantus Roseus (Tsitsirika) Against Albino RabbitsDocument2 pagesHypoglycemic Effect of Catharantus Roseus (Tsitsirika) Against Albino RabbitsCarlos NiñoNo ratings yet
- Severe Headache: Clinical Manifestations: LOC, GCS 3, Anisocoric Pupils, Very Minimal Eyelid Movements To CornealDocument1 pageSevere Headache: Clinical Manifestations: LOC, GCS 3, Anisocoric Pupils, Very Minimal Eyelid Movements To CornealCarlos NiñoNo ratings yet
- Hypoglycemic Effect of Catharantus Roseus (Tsitsirika) Against Albino RabbitsDocument2 pagesHypoglycemic Effect of Catharantus Roseus (Tsitsirika) Against Albino RabbitsCarlos NiñoNo ratings yet
- Gross Anats Presem ReviewDocument14 pagesGross Anats Presem ReviewCarlos NiñoNo ratings yet
- Higher Cortical FunctionsDocument2 pagesHigher Cortical FunctionsCarlos NiñoNo ratings yet
- Carlos D. Achondo Jr. 2MD-1Document4 pagesCarlos D. Achondo Jr. 2MD-1Carlos NiñoNo ratings yet
- Biochem3 Amino AcidsDocument3 pagesBiochem3 Amino AcidsCarlos NiñoNo ratings yet
- Officinale) Which Exhibited Its Anti-Angiogenic Property by Decreasing The CAMDocument2 pagesOfficinale) Which Exhibited Its Anti-Angiogenic Property by Decreasing The CAMCarlos NiñoNo ratings yet
- In Schools Needed Say CampaignersDocument11 pagesIn Schools Needed Say CampaignersCarlos NiñoNo ratings yet
- Syllabi For Basic PharmacologyDocument1 pageSyllabi For Basic PharmacologyCarlos NiñoNo ratings yet
- Hypertensive DietDocument6 pagesHypertensive DietCarlos NiñoNo ratings yet
- Officinale) Which Exhibited Its Anti-Angiogenic Property by Decreasing The CAMDocument2 pagesOfficinale) Which Exhibited Its Anti-Angiogenic Property by Decreasing The CAMCarlos NiñoNo ratings yet
- Pharmacology Long Exam 1 2 Yr - 2 Sem 2016: ND NDDocument2 pagesPharmacology Long Exam 1 2 Yr - 2 Sem 2016: ND NDCarlos NiñoNo ratings yet
- Histo Path PUDDocument1 pageHisto Path PUDCarlos NiñoNo ratings yet
- Heart, Blood and Lymph NodesDocument12 pagesHeart, Blood and Lymph NodesCarlos NiñoNo ratings yet
- Gross Anats Presem ReviewDocument14 pagesGross Anats Presem ReviewCarlos NiñoNo ratings yet
- Le Ga 1Document15 pagesLe Ga 1Carlos NiñoNo ratings yet
- Glasgow Coma ScaleDocument2 pagesGlasgow Coma Scalejean thereseNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Senior Project ProposalDocument10 pagesSenior Project Proposalapi-384821983No ratings yet
- Days Papers 2001Document341 pagesDays Papers 2001jorgefeitoza_hotmailNo ratings yet
- Jurnal AnemiaDocument4 pagesJurnal AnemiaAchmad Aidil TazakkaNo ratings yet
- Jurnal SyringomaDocument16 pagesJurnal SyringomaNajibah Zulfa Assa'diyahNo ratings yet
- M4164-C 06-15 - Etrinsa Technical Manual - MN031r2hq PDFDocument142 pagesM4164-C 06-15 - Etrinsa Technical Manual - MN031r2hq PDFMaria Lavinia IordacheNo ratings yet
- Edgar Cayce On HealingDocument132 pagesEdgar Cayce On Healinganca_dinca0% (1)
- DentistryDocument16 pagesDentistryMeka Syahputra56% (9)
- ADHD in ChildrenDocument16 pagesADHD in ChildrenCoco Hithere100% (1)
- CPAP ManualDocument43 pagesCPAP ManualTachira Julher RiveraNo ratings yet
- Resumen Pediatria 2Document77 pagesResumen Pediatria 2Chris Ledezma JorqueraNo ratings yet
- Critical Reasoning - Practice ProblemsDocument83 pagesCritical Reasoning - Practice ProblemsReemaNo ratings yet
- Anxiety DisorderDocument9 pagesAnxiety DisorderSatish KujurNo ratings yet
- Spinal Cord CompressionDocument4 pagesSpinal Cord Compressionian3yeung-2No ratings yet
- BDD Module 2 - Maintenance2 PDFDocument14 pagesBDD Module 2 - Maintenance2 PDFHemant KumarNo ratings yet
- Case Presentation BSMMU As 3rd AuthorDocument4 pagesCase Presentation BSMMU As 3rd AuthorGovind ChaudharyNo ratings yet
- Micro Tech Endoscopy Product CatalogDocument42 pagesMicro Tech Endoscopy Product CatalogyasuluNo ratings yet
- SpiritualityandGestalt AGestalt TranspersonalPerspectiveDocument16 pagesSpiritualityandGestalt AGestalt TranspersonalPerspectiveOlgaCanessa100% (1)
- Impaired Gas ExchangeDocument10 pagesImpaired Gas ExchangeWardinatul ImanNo ratings yet
- Atrial FibrillationDocument14 pagesAtrial FibrillationNur Atiqah ZainalNo ratings yet
- Crushing and Liquid ARV FormulationsDocument18 pagesCrushing and Liquid ARV FormulationsKumar BhaiNo ratings yet
- Pancha Karma (Sree Subramania Ayurvedic Nursing Home)Document15 pagesPancha Karma (Sree Subramania Ayurvedic Nursing Home)Sanand Ratnam Thekkayil100% (1)
- Innovations in Medical ElectronicsDocument10 pagesInnovations in Medical Electronicsapi-3837905100% (5)
- Ohi Graphic OrganizerDocument1 pageOhi Graphic Organizerapi-278298083No ratings yet
- Yakima Co (WA) Protocols 2010Document117 pagesYakima Co (WA) Protocols 2010Anthony James-Hartwell100% (1)
- Nasal Polyp Nasa Arsha Management Through Ayurveda A Single Case StudyDocument4 pagesNasal Polyp Nasa Arsha Management Through Ayurveda A Single Case StudyEditor IJTSRDNo ratings yet
- ABG Quiz by GroupDocument13 pagesABG Quiz by Grouplourd nabNo ratings yet
- HAAD Exam For Nurses Questions 2018Document46 pagesHAAD Exam For Nurses Questions 2018Asif Newaz100% (6)
- Bladder StonesDocument20 pagesBladder StonesRiean AuliaNo ratings yet
- Clinical Approach To Syncope in ChildrenDocument6 pagesClinical Approach To Syncope in ChildrenJahzeel Gacitúa Becerra100% (1)
- Dcpip Food TestDocument14 pagesDcpip Food TestSyahir YaakopNo ratings yet