Professional Documents
Culture Documents
Naloxone
Uploaded by
noddy59Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Naloxone
Uploaded by
noddy59Copyright:
Available Formats
update: naloxone
Naloxone is used with caution in the elderly and given to pregnant or lactating mothers only if absolutely necessary1. Observe for convulsions, excessive crying and hyperactive reflexes in neonates born to mothers with opioid dependence1. Close monitoring of the patient is required to detect when repeated doses of naloxone are required2. The duration of most opioids exceeds the half life of naloxone1. Ensure the resuscitation trolley is immediately available. Reversing opioid depression in the post operative period may induce nausea, vomiting, tachycardia, hypertension, tremors, seizures, arrhythmias or cardiac arrest1. Consequently, be cautious if your patient has a history of cardiovascular disease. Central nervous system effects include seizures and parasthesia1. Agitation, hallucination, hot flushes and tremors have been reported, especially in patients who are in pain1. Of note, dyspnoea and paradoxical respiratory depression may occur. Hypertension or hypotension may develop; however, elevated blood pressure is the more common event. ADMINISTRATION Naloxone is given predominantly in emergency situations, deeming the intravenous route appropriate in most cases1. Naloxone can be prepared as an infusion if required1. Some brands of naloxone are available in a pre-filled syringe1. Continuous surveillance of the patient is essential2. The intravenous dosage varies according to the underlying cause of opioid depression. Adults in suspected or known overdosage usually respond to 0.4mg to 2mg increments of naloxone every two to three minutes1. Conditions unresponsive to a cumulative dosage of 10mg are likely to be non opioid in origin1. Reduced dosage is used to reverse opioid depression in the post operative patient; 0.1mg to 0.2mg increments are sufficient1. Increments are titrated to effect based on respiratory recovery without the loss of analgesia. Children in known or suspected opioid overdosage are administered 0.01mg/kg of intravenous naloxone1. If no improvement is seen, an additional 0.1mg/kg dose is given. Children in postoperative opioid depression are given very small increments every two to three minutes until the desired reversal is achieved1. Neonates are administered 0.01mg/ kg increments of naloxone in IV, intramuscular or subcutaneous form1. REFERENCES
Read this article and complete the online quiz to earn 0.5 iFolio hours
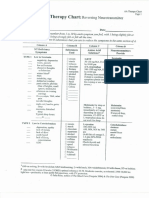
In this clinical update you will read about the pharmacology of naloxone, a drug indicated in the reversal of opioids. GENERIC NAME Naloxone hydrochloride1. TRADE NAMES Naloxone, suboxone (sublingual tablets)1. DRUG CLASS Schedule 4 opioid antagonist1. INDICATIONS Naloxone is indicated for the reversal of opioid depression caused by natural or synthetic opioids2. Respiratory depression is the most obvious sign of narcosis. Sedation and hypotension are also reversed by naloxone1. Naloxone is diagnostic in known or suspected opioid overdosage. ACTIONS Naloxone competes for opiate receptors located in the central nervous system2. Circulating opioids cannot bind to these receptors, minimising their effect. The most rapid onset of action is achieved after intravenous administration (IV); however, intramuscular or subcutaneous routes are an alternative if IV access is unavailable1. Intravenous naloxone has a shorter half life than the same dose given intramuscularly. CONTRAINDICATIONS Naloxone is generally well tolerated. It is avoided in patients with a known hypersensitivity to the drug or its additives1. PRECAUTIONS Reversing the effects of opioids in a narcotised patient will also reverse analgesic effects and will induce acute withdrawal syndrome in patients who are physically dependent on opioids1. Therefore, the roused patient may be in pain or experiencing acute withdrawal. Box one lists the signs and symptoms of acute withdrawal from opioids.
Naloxone is ineffective in patients given non-opioid drugs
ADVERSE EFFECTS Are broadly categorised according to opioid dependence or the post operative period. Abrupt reversal of opioids in the dependent patient will likely result in acute withdrawal syndrome and the signs and symptoms listed in Box one. The possible adverse effects observed in the post operative patient (not in acute withdrawal) are; nausea, vomiting, tachycardia, hypertension, tremors, seizures, arrhythmias, heart failure, acute pulmonary oedema or cardiac arrest1.
Box 1 Signs and symptoms of acute withdrawal from opioids 1 Abdominal cramps and diarrhoea Fever Hypertension Irritability, shivering or trembling Myalgia Nausea and vomiting Piloerection Sneezing and runny nose Tachycardia
1.
Naloxone (2009). MIMS online. Retrieved 8 April 2011 from MIMS database, MIMS Australia (ANF). Eckman, M., Labus, D., & Thompson, G. (Eds.). (2009). Nursing Pharmacology Made Incredibly Easy (2nd ed.). Sydney: Lippincott, Williams and Wilkins.
2.
You might also like
- Emergency Mental Health PresentationsDocument45 pagesEmergency Mental Health Presentationsnoddy59No ratings yet
- Carefoot250W CandyDocument4 pagesCarefoot250W Candynoddy59No ratings yet
- Pain MGMT With Amino AcidsDocument3 pagesPain MGMT With Amino Acidsnoddy59No ratings yet
- MagnesiumReport NoCalloutDocument14 pagesMagnesiumReport NoCalloutnoddy59No ratings yet
- The Cure For All DiseasesDocument631 pagesThe Cure For All DiseasesMirna98% (93)
- Amino Acid TherapyDocument4 pagesAmino Acid Therapynoddy59No ratings yet
- Charlie Chaplin - Poster V2Document1 pageCharlie Chaplin - Poster V2noddy59No ratings yet
- Trudy Scott Say No To Benzodiazepines ReferencesDocument4 pagesTrudy Scott Say No To Benzodiazepines Referencesnoddy59No ratings yet
- Christie Marie Sheldon - Energetic Breakthrough GuideDocument11 pagesChristie Marie Sheldon - Energetic Breakthrough Guidepowersolv100% (1)
- 22 Ways To Cancer Proof Your LifeDocument34 pages22 Ways To Cancer Proof Your LifeNicholas JonesNo ratings yet
- Body Language LogDocument1 pageBody Language Lognoddy59No ratings yet
- Bounce Back Big Ebook Nov2015Document34 pagesBounce Back Big Ebook Nov2015noddy59No ratings yet
- Scottish KingsDocument1 pageScottish Kingsrestlessnative265No ratings yet
- AnaphylaxisDocument10 pagesAnaphylaxisnoddy59No ratings yet
- DR - Mercola-Total Health CookbookDocument270 pagesDR - Mercola-Total Health CookbookGabi GrNo ratings yet
- Psychiatric GlossaryDocument31 pagesPsychiatric Glossarynoddy59No ratings yet
- Burns AssessmentDocument25 pagesBurns Assessmentnoddy59No ratings yet
- Blood - INRDocument12 pagesBlood - INRnoddy59No ratings yet
- Infection ControlDocument24 pagesInfection Controlnoddy59No ratings yet
- Handy Hints For Clinical SupervisorsDocument15 pagesHandy Hints For Clinical Supervisorsnoddy59No ratings yet
- Global WoundsDocument49 pagesGlobal Woundsnoddy59No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- RH BLOOD GROUPDocument23 pagesRH BLOOD GROUPWho KnowsNo ratings yet
- Hand Hygiene Self Assessment FrameworkDocument9 pagesHand Hygiene Self Assessment FrameworkWiDya EmiLiaNo ratings yet
- Textbook CH 9 Industrialization and ImperialismDocument17 pagesTextbook CH 9 Industrialization and Imperialismapi-234531449100% (2)
- Blood Supply of HeartDocument40 pagesBlood Supply of HeartSaket Daokar100% (1)
- Chorti DictionaryDocument285 pagesChorti DictionaryLuis Bedoya100% (1)
- Clinical Manifestations and Management of Hospitalized Women With Bartholin Versus Non Bartholin Vulvar AbscessDocument4 pagesClinical Manifestations and Management of Hospitalized Women With Bartholin Versus Non Bartholin Vulvar AbscessPaul HartingNo ratings yet
- HMIS IntroductionDocument25 pagesHMIS IntroductionMeenal KulkarniNo ratings yet
- Keto DietDocument2 pagesKeto DietdewiNo ratings yet
- Introduction PRDS and APRDSDocument13 pagesIntroduction PRDS and APRDSPrudhvi RajNo ratings yet
- You Might Need SomebodyDocument11 pagesYou Might Need SomebodyHans georg NeyNo ratings yet
- 7 Vs 14days Gram Negative SepsisDocument8 pages7 Vs 14days Gram Negative SepsisPavan KumarNo ratings yet
- ADA Guideline - Chronic Kidney Disease Evidence-Based Nutrition Practice GuidelineDocument19 pagesADA Guideline - Chronic Kidney Disease Evidence-Based Nutrition Practice GuidelineJorge SánchezNo ratings yet
- Radiographic Positioning and Related Anatomy 8Th Edition Bontrager Test Bank Full Chapter PDFDocument35 pagesRadiographic Positioning and Related Anatomy 8Th Edition Bontrager Test Bank Full Chapter PDFdecagrambarrymfh100% (5)
- Setting up MRI Scan CentresDocument86 pagesSetting up MRI Scan CentresGokilavani RajagopalNo ratings yet
- Goffman's Theory of Stigmatization and Its Impact on HealthDocument10 pagesGoffman's Theory of Stigmatization and Its Impact on HealthNaomi100% (1)
- Generic Name: Brand Name: Apo-Metoprolol, Betaloc, Lopressor, Novo-Metoprolol, Nu-Drug ClassificationDocument4 pagesGeneric Name: Brand Name: Apo-Metoprolol, Betaloc, Lopressor, Novo-Metoprolol, Nu-Drug ClassificationKat ZNo ratings yet
- Ageing - Physical and Psychological Changes. Pathological Ageing-11!19!2011Document4 pagesAgeing - Physical and Psychological Changes. Pathological Ageing-11!19!2011TaylorNo ratings yet
- Endocrine Davidson Shortlisted (Hira - Fj'23)Document45 pagesEndocrine Davidson Shortlisted (Hira - Fj'23)saifsaffa2No ratings yet
- DNA Lab Reveals Human EvolutionDocument136 pagesDNA Lab Reveals Human EvolutionMarlonLopezSilvozaNo ratings yet
- Treat Herpes Infections with AciclovirDocument1 pageTreat Herpes Infections with AciclovirAllen MendozaNo ratings yet
- Leafy Vegetables HarvestingDocument18 pagesLeafy Vegetables HarvestingSonia BadaNo ratings yet
- JAM 2022 Biotechnology QuestionsDocument28 pagesJAM 2022 Biotechnology QuestionsKumar KalyanNo ratings yet
- Lesson PlanDocument5 pagesLesson Planapi-456870847No ratings yet
- University of Barisal: AssignmentDocument7 pagesUniversity of Barisal: AssignmentFiroj AhmedNo ratings yet
- 3911515Document1 page3911515Gemmelle CangcoNo ratings yet
- Diabetic Ketoacidosis Care Guideline EdDocument2 pagesDiabetic Ketoacidosis Care Guideline EdSeno Adi WicaksonoNo ratings yet
- Fluid Volume Deficit Assessment and ManagementDocument1 pageFluid Volume Deficit Assessment and ManagementNorbert Ju NeNo ratings yet
- Practice Exam-10000 SeriesDocument12 pagesPractice Exam-10000 SeriesJuan Romero86% (28)
- Internal Medicine 5th MidtermDocument13 pagesInternal Medicine 5th MidtermIashdip iashdipNo ratings yet