Professional Documents
Culture Documents
Promoting Healthy Older People
Uploaded by
Guy DewsburyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Promoting Healthy Older People
Uploaded by
Guy DewsburyCopyright:
Available Formats
Promoting healthy older people - A background paper
July 9th 2010
Guy Dewsbury PhD www.gdewsbury.com
The current trend in which older are becoming more aware and more responsible for their own health has a clear link to trends that have been identified by the Department of Health, the Kings Fund and the World Health Organisation. Tracing things back to their origin is somewhat difficult as there has always been a certain amount of rhetoric on older peoples health. A decisive change can be seen to some extent with the Governments release of Our Healthier Nation (1998) in which it is mentioned that there should be a people should improve their own health supported by communities working through local organisations against the backdrop of the Government which will be achieved through the introduction of NHS direct; Health skills programme and the expert patient. This was followed the following year by the WHO directive Health 21 (19999), which set out the agenda for a healthy society and cites healthy ageing as one of its 21 targets. In the UK 1999, the International Year of Older Persons, also saw the introduction of the Health Act (1999) which advanced pooled budgets and joint commissioning of integrated service between health and social care. Saving Lives: Our Healthier Nation (1999) set out targets by which there would be reductions in death rates of cancer, coronary heart disease, stroke, accidents, and mental illness, which will be achieved by the introduction of NHS Direct, Health Skills and Expert Patients; the establishment of the Health Development Agency and increased education and training for health and establish a new Public Health Fund. In the same year the DH released the Long Term Care The Governments response to the Health Committees Report for Long Term Care (1999) in which they introduce the National Service Framework for older people and calls for more consistent data on older people health and social policy. Urge to move towards Danish model of care of older people. The new century heralded a plethora of publications from on older peoples health, which started with the DH publication entitled Out in the open: Breaking down the barriers for older people (2000) which introduces the notion of commissioning services for older people and the NHS plan: The governments response to the Royal commission for long term care (2000) announced the development of Intermediate Care Services to enable older people retain
independence at home, integrated services for older people. These papers were followed in 2001 by the establishment NSF for older people (2001) which set out to root out age discrimination by providing person-centred care and promoting older peoples health and independence and fitting services to older peoples needs. The key passage of this NSF is the establishment of Standard 8 refers to the promotion of health and an active life in older age. Also in 2001 the DH released a paper called Caring for older people a nursing priority (2001) in which it asserts the need for nursing as a key part in enhancing older peoples autonomy and independence. Nurses, it contends, must attend to the whole person not just the acute symptoms. In this way, nursing changes its focus from acute care to prevention. The year 2002 WHO released their influential document on Active Ageing (2001) which continues where their Health21 agenda document left off by demonstrating that WHO consider health from a life-course perspective and aims to enable older people to get the best possible quality of life for as long as possible through local community strategies. The DH document Information services for older people in England (2002) considers the strategies required to provide health and social care information to older people including educational needs and other opportunities and also calls for monitoring wellbeing which underpins independence and healthy ageing. This year the Kings Fund released a document entitled Great to be Grey (2002) which reflects on the recruitment and retention of older staff. The DH document called Better health in Old age (2004) promotes the development of older people as active citizens within their communities and within their families, helping to create a stronger and more prosperous society and has a whole section on promoting health and active life in reports and case studies. Also in 2004 the DH released Choose Health: making health choices (2004) builds on previous DH documents and extols the virtues of making healthy choices; providing better information; demand for health as market influence; (Page 86 is interesting as it goes through some of the reasons why older people do not take exercise.). The DH documents were compounded in 2005 by the release of the Kings Fund report entitled The business of caring (2005) which found older people experienced restricted access to care and practical support, limited choice and control over care services, and were being put at risk by untrained staff and difficulties with funding. The document calls for a culture that sees older people as equal partners focusing on their rights as well as needs and suggests care services should be responsive to fluctuating needs and unpredictable health. The DH also released a number of documents on which the first was entitled independence, wellbeing and choice (2005) in which it advances that care service should support independence whist providing choice and control over how their needs are met and the NHS and social care should have shared agenda. The DWP and DH released Health work and well-being caring for our future A strategy for the health and well-being of working age people (2005) which focused on
promoting health in and out of work. This should also be read with A New Pension Settlement for the Twenty-First Century: The second report of the Pensions Commission [The Turner Report] (2005) which states that the current system of private funded pensions combined with the current state system will deliver increasingly inadequate and unequal results. Long-term pension policy needs to be robust in the face of rising life expectancy as a result a pensions rethink is in order. Independence, Well-being and Choice: Our vision for the future of social care for adults in England (2005) The Green Paper on older people using social care and other local authority services will be given individual budgets so that they can buy in the services they need. Opportunity Age: Meeting the challenges of ageing in the 21st century (2005) was the first ever cross-government strategy that looks specifically at the issues facing British society as people live longer, healthier lives and addresses extending people's working lives, supporting active ageing in the community and giving people more choice and independence, especially 'shedding the stereotypes' that surround older people. The SPAIN (the Social Policy on Ageing Information Network) What Price Care in Old Age? (2005) report argues that although the government has taken steps to address the failing system of social care for older people, rising costs have meant there is little sign of a reversal in the trend towards targeting care at ever fewer people with very high care needs. Little progress has been made in closing the gap between funding for older care recipients as compared to others. The National Service Framework for Long Term Conditions (2005) sets 11 quality requirements to transform the way health and social care services support people with long-term neurological conditions to live as independently as possible. Although the NSF focuses on people with long-term neurological conditions, much of the guidance it offers can apply to anyone living with a long-term condition. The Department of Health published the White Paper Our health, our care, our say (2006) on future plans for the whole health and social care system by proposing a radical shift in the way in which services are delivered through four main goals: the provision of better prevention services with earlier intervention; More choice and a louder voice; Tackling inequalities and improved access to community services; and more support for people with long-term needs. The final report from the Social Exclusion Unit of the ODPM A Sure Start to Later Life: Ending inequalities for older people (2006) details government plans to mitigate the exclusion, poverty and isolation experienced by older people by locating a single, accessible gateway to wide ranging services in the community, where potential problems can be identified quickly and prevented from becoming worse. Time to Care? An overview of home care services for older people in England, 2006: A Report from the Commission for Social Care Inspection (2006) states that home care is an essential service, which is enabling thousands of older people to remain safely at home, however, there is evidence that the current arrangements for commissioning and providing home care are
likely to be unsustainable for a number of reasons. A New Ambition for Old Age: Next steps in implementing the National Service Framework for Older People: A report from Professor Ian Philp, National Director for Older People (2006) sets out the priorities for the second phase of the governments ten-year National Service Framework (NSF) for Older People under three themes: dignity in care, joined-up care and healthy ageing. The final report of the Wanless social care review team Securing Good Care for Older People: Taking a long-term view (2006) estimated the contribution of demographic pressures and the need to improve outcomes would increase the costs of older people's social care to 29.5 billion in 2026. Funding proposals include restricting means-testing for personal care and putting in place a free package of basic care, topped up by personal contributions matched by the state. The ministerial concordat Putting People First, A shared vision and commitment to the transformation of Adult Social Care (2007) sets out the transformation of adult social care, and recognises that the sector will work across shared agendas with users and carers to transform peoples experience of local support and services. It promotes enabling people to live their own lives as they wish and promote their own individual needs for independence, wellbeing and dignity. The Public Service Agreement (PSA) 17 issued by the Department for Work on Pensions entitled Tackle Poverty and Promote Greater Independence and Well-being in Later Life (2007) set out the outcomes the government seeks to achieve in the Comprehensive Spending Review period to promote improvements in independence and well-being in later life for the longer term. In A Recipe for Care - Not a Single Ingredient: Clinical case for change: Report by Professor Ian Philp, National Director for Older People (2007) Professor Philp identifies a fivepoint plan to improve older people's care: (1) early intervention and assessment of old age conditions; (2) long-term conditions management in the community, integrated with social care and specialist services; (3) early supported discharge from hospital and whenever possible delivering care closer to home; (4) general acute hospital care whenever needed, combined with quick access to new specialist centres; (5) partnerships built around the needs and wishes of older people and their families. The result should be demonstrated by reduced need for acute hospital care and increased investment in preventive services and community based health and care services. The All Party Parliamentary Local Government Group report Never Too Late for Living Inquiry into services for older people (2008) reported the results of its inquiry into services for older people. The inquiry focused on the key role and contribution of local authorities in promoting the quality of life of older people. The Health and Social Care Act (2008) established the Care Quality Commission; reforming professional regulation; updating existing public health protection legislation; and strengthening the protection of vulnerable people using residential care by ensuring that any independent sector care home providing care on behalf of a local authority is subject to the Human Rights Act. The Independent Living, A cross-government
strategy about independent living for disabled people (2008) five-year strategy joins current and new policy initiatives to provide a coherent framework for making progress towards independent living for disabled people, including older disabled people. The Darzi report entitled High Quality care for all (2008) in which Lord Darzi identified a range of hospital services that could be delivered closer to the patients home, including minor surgery and many outpatient consultations, although some services such as stroke and heart disease should be more specialist and centralised. PCTs together with local authorities are to be responsible for commissioning comprehensive well-being and prevention services. Patients with complex longterm conditions were to be entitled to a named care coordinator, such as a community matron, to help them access the services in their personal care plans. The Personal Care at Home Bill (2009) offered free personal care at home for those with the highest needs, regardless of means, such as those with serious dementia and with Parkinson's Disease. It includes provision to invest in re-ablement and prevention to help people live at home for longer. The national review of age discrimination and age equality in the health and social care sector entitled Achieving Age Equality in Health and Social Care (2009) was set up to help health and social care organisations meet the ban on age discrimination and the new public sector equality duty in the Equality Bill. The review analysed evidence about the nature, extent and variability of age discrimination in health and social care services The white paper Building a National Care Service (2010) proposed fundamental reform of the care and support system for all adults in England building a new National Care Service. The King's Fund report Securing Good Care for More People: Options for Reform (2010) takes forward the 2006 review of social care by the King's Fund (Wanless report) to provide fresh evidence of the 'compelling need for reform' with projections drawing on revised modelling and suggests a key principle of reform is that costs of care are required to be shared responsibly between the individual and the state. The Audit Commission report on local government Under Pressure: Tackling the Financial Challenge for Councils of an Ageing Population (2010) examines the issues facing councils with an ageing population requiring a range of services as public spending reduces. It suggests that councils are not planning strategically for an ageing population and do not know enough about the costs. In addition, cost savings that could arise from preventive services and better work with other organisations are not being explored fully by councils. The Marmot Review Fair Society, Healthy Lives (2010) sort to propose an evidence based strategy for reducing health inequalities from 2010. Action on health inequalities require action across all the social determinants of health. Universal action is required but with a scale and intensity that is proportionate to the level of disadvantage - called 'proportionate universalism'. The fair distribution of health, wellbeing and sustainability are important social goals. The Green Paper Shaping the Future of Care Together (2010) set out a vision for a new
care and support system based on a National Care Service that is to be fair, simple and affordable which include prevention services; national assessments; a joined-up service; information and advice; personalised care and support; and fair funding. With the introduction of the Equality Bill (2010) will make it unlawful to discriminate against someone aged 18 or over because of age when providing services or carrying out public functions. It will not affect products or services for older people where age-based treatment is justified or beneficial. The law will only stop age discrimination where it has negative or harmful consequences.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- What Is Ehealth?Document8 pagesWhat Is Ehealth?Guy DewsburyNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Enabling and Applying Person-Centred Design For Older AdultsDocument2 pagesEnabling and Applying Person-Centred Design For Older AdultsGuy DewsburyNo ratings yet
- Putting People First: The Personalisation of Tele-Support DevicesDocument2 pagesPutting People First: The Personalisation of Tele-Support DevicesGuy DewsburyNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Putting People First: The Personalisation of Tele-Support DevicesDocument2 pagesPutting People First: The Personalisation of Tele-Support DevicesGuy DewsburyNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Baxter, Monk, Doughty, Dewsbury, - Standards and The Dependability of Electronic Assistive TechnologyDocument8 pagesBaxter, Monk, Doughty, Dewsbury, - Standards and The Dependability of Electronic Assistive TechnologyGuy DewsburyNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Sore Legs and Naked BottomsDocument10 pagesSore Legs and Naked BottomsGuy DewsburyNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Dependability and Trust in Organisational and Domestic Computer Systems SafecompDocument13 pagesDependability and Trust in Organisational and Domestic Computer Systems SafecompGuy DewsburyNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Designing Appropriate Assistive Technology For Home Users 3Document21 pagesDesigning Appropriate Assistive Technology For Home Users 3Guy DewsburyNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Easy For Everyone 2004-Bagnall-EasyDocument4 pagesEasy For Everyone 2004-Bagnall-EasyGuy DewsburyNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- While & Dewsbury (2011 Online) Nursing & ICT-A Discussion of Trends & Future DirectionsDocument9 pagesWhile & Dewsbury (2011 Online) Nursing & ICT-A Discussion of Trends & Future DirectionsGuy DewsburyNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Dewsbury Linksell Neuropaper 2011Document12 pagesDewsbury Linksell Neuropaper 2011Guy DewsburyNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- 06.2 Home MSC Dependability FinalDocument63 pages06.2 Home MSC Dependability FinalGuy DewsburyNo ratings yet
- Promoting Virtual Social Interaction With Older PeopleDocument55 pagesPromoting Virtual Social Interaction With Older PeopleGuy DewsburyNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Dewsbury, Rouncefield Clarke and Sommerville-Designing Appropriate Assistive Technology For Home Users - Developing Dependable Networks.Document14 pagesDewsbury, Rouncefield Clarke and Sommerville-Designing Appropriate Assistive Technology For Home Users - Developing Dependable Networks.Guy DewsburyNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Duplicate 07.2 HomeDocument50 pagesDuplicate 07.2 HomeGuy DewsburyNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- When Geography MattersDocument17 pagesWhen Geography MattersGuy DewsburyNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Designing Assistive Technologies For Medication Regimes in Care SettingsDocument12 pagesDesigning Assistive Technologies For Medication Regimes in Care SettingsGuy DewsburyNo ratings yet
- NNDRDocument10 pagesNNDRGuy DewsburyNo ratings yet
- Mainstreaming Telecare 2009 PresentationDocument10 pagesMainstreaming Telecare 2009 PresentationGuy DewsburyNo ratings yet
- Smart ThinkingDocument73 pagesSmart ThinkingGuy DewsburyNo ratings yet
- Smart ThinkingDocument73 pagesSmart ThinkingGuy DewsburyNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Dewsbury KT EQUAL - The User 2009Document20 pagesDewsbury KT EQUAL - The User 2009Guy DewsburyNo ratings yet
- Literature ReviewDocument7 pagesLiterature ReviewResianaPutriNo ratings yet
- New International Society of Hypertension (Ish) Guidelines 2020 - January 17TH 2021Document35 pagesNew International Society of Hypertension (Ish) Guidelines 2020 - January 17TH 2021Rhama Patria100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Quality Laboratory Standards: in KenyaDocument20 pagesQuality Laboratory Standards: in KenyaKate NjinuNo ratings yet
- Dental JOURNAL: Geographic Tongue in A 6 Year Old Child: A Case Report With Review of LiteratureDocument6 pagesDental JOURNAL: Geographic Tongue in A 6 Year Old Child: A Case Report With Review of LiteraturewennyNo ratings yet
- 2021 American College of Rheumatology Guideline For The Treatment of Rheumatoid ArthritisDocument30 pages2021 American College of Rheumatology Guideline For The Treatment of Rheumatoid Arthritisjose pablo quero reyesNo ratings yet
- HTN and Arrh AfzalDocument8 pagesHTN and Arrh AfzalAFA.BLSNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- RBC PathologyDocument7 pagesRBC PathologyKent CruzNo ratings yet
- Clinic Department InfoDocument66 pagesClinic Department InfoHumera ShaikhNo ratings yet
- MCB 11 Lab HW Kinds of PlatingDocument1 pageMCB 11 Lab HW Kinds of PlatingMaria Isabelle VillacorteNo ratings yet
- How Is Turner Syndrome DiagnosedDocument9 pagesHow Is Turner Syndrome DiagnosedAnonymous lKO78aNo ratings yet
- Can Oral Sex Cause Throat CancerDocument4 pagesCan Oral Sex Cause Throat CancerjyuldipNo ratings yet
- Mahendra Chaudhry Claims His Case As Tainted: Island Driving SchoolDocument48 pagesMahendra Chaudhry Claims His Case As Tainted: Island Driving SchoolfijitimescanadaNo ratings yet
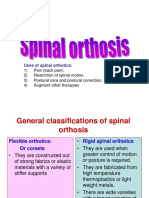
- Spinal OrthosisDocument16 pagesSpinal OrthosisChristya Ari NugrahaNo ratings yet
- 03 Orlando D. Garcia, JR., Et Al. vs. Ranida Salvador, Et Al.Document2 pages03 Orlando D. Garcia, JR., Et Al. vs. Ranida Salvador, Et Al.Raj AtmanNo ratings yet
- Substance Abuse BrochureDocument2 pagesSubstance Abuse Brochureapi-272566401No ratings yet
- Ayurveda PDFDocument12 pagesAyurveda PDFsanjit0907_982377739No ratings yet
- Classification of Mental Disorder, Antisocial Personalities, Drug and Alcohol DependenceDocument15 pagesClassification of Mental Disorder, Antisocial Personalities, Drug and Alcohol DependenceAdrian SingsonNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Menastil Complete Clinical Trials - Pain Relief That Works.Document43 pagesMenastil Complete Clinical Trials - Pain Relief That Works.emoryholstNo ratings yet
- Betz Rebecca ResumeDocument2 pagesBetz Rebecca Resumeapi-316054946No ratings yet
- Erectile Dysfunction PDFDocument288 pagesErectile Dysfunction PDFMikaelNJonssonNo ratings yet
- Running Head: Normal Saline vs. Heparin 1Document9 pagesRunning Head: Normal Saline vs. Heparin 1MaureenAmilcaNo ratings yet
- Yoga-and-Ayurveda-David-Frawley.07104 - 3prana, Tejas and Ojas PDFDocument7 pagesYoga-and-Ayurveda-David-Frawley.07104 - 3prana, Tejas and Ojas PDFlelis2013No ratings yet
- Summer Training Project ReportDocument55 pagesSummer Training Project ReportShikha TrehanNo ratings yet
- InflammationDocument41 pagesInflammationbharath goNo ratings yet
- Jurnal Serumen PropDocument21 pagesJurnal Serumen Proprowin93No ratings yet
- Clinical Mycology 2nd Ed (PDF) (Tahir99) VRGDocument674 pagesClinical Mycology 2nd Ed (PDF) (Tahir99) VRGbiliboiNo ratings yet
- Mapping Bedah Saraf, 1 Juli 2019Document1 pageMapping Bedah Saraf, 1 Juli 2019Dessy FarwasNo ratings yet
- Teaching Plan For HypertensionDocument5 pagesTeaching Plan For HypertensionMaureen Mae Binohlan100% (1)
- Intertrigo and Secondary Skin InfectionsDocument5 pagesIntertrigo and Secondary Skin Infectionskhalizamaulina100% (1)
- Nervous SystemDocument92 pagesNervous SystemmaricarNo ratings yet
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryFrom EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryRating: 4.5 out of 5 stars4.5/5 (157)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)