Professional Documents
Culture Documents
2003 Blood Bank Procedures
Uploaded by
Devvi Riasari BunardiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2003 Blood Bank Procedures
Uploaded by
Devvi Riasari BunardiCopyright:
Available Formats
6TH ANNUAL WORKSHOP HEMATOLOGY AND BLOOD TRANSFUSION
05 09 MUHARRAM 1424 (08-12 MARCH 2003)
BLOOD BANK PROCEDURES
TABLE OF CONTENTS
Specimen Receipt Grading of Agglutination Reactions Reagent Quality Control ABO Grouping Discrepancies Resolution Antibody Screen Crossmatch Antibody Identification Basic Panel Antibody Identification Ficin Panel Antigen Typing Direct Antiglobulin Testing Elusion Acid (Elu-kit) Elution Lui Freeze Emergency Transfusion Transfusion Reaction Investigations W.A.R.M Adsorption Technique Antibody Titration 1-5 6-8 9-12 13-16 17-22 23-29 30-38 39-44 45-49 50-53 54-57 58-61 62-67 68-79 80-82 83-85 86-95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
TITLE / DESCRIPTION:
INDEX NUMBER(S):
SPECIMEN RECEIPT
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
610
FEB92
REV11 / AUG02
DP XM
PRINCIPLE Proper collection and labeling of Blood Bank specimens is of the utmost importance to ensure patient safety.
POLICY All samples received in the Blood Bank will be labeled in accordance with AABB Standards 5.11 Samples not meeting the labeling requirements must be recollected. Although samples of insufficient quantity should generally not be received, it may be necessary to process these samples when difficulties in collection were encountered. All specimens are drawn according to Specimen Collection and Processing Policies SCP-02-05, SCP-02-06 and SCP-02-07. Rejection of inadequately collected or labeled samples will be handled in accordance with LABOM-01-69 Handling and Documentation of Sample Integrity Issues. Specimen Collections and Processing will receive all Blood Bank samples initially. necessary they may reject samples not meeting Blood Bank criteria. Where
A second sample receipt and acceptance will occur in the Blood Bank. At this time, a Transfusion Service staff member will confirm that all identifying information on the request is in agreement with that on the sample label. Only after this confirmation can testing begin. In certain situations it may be necessary to process an inadequately labeled sample, but only with approval of the Blood Bank Supervisor or Medical Director.
Page 1 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
SPECIMEN
CROSSMATCH TEST Type and Screen* Crossmatch* Ab Titre ABO Iso DAT Red Cell Phenotype Group Confirmation Transfusion Reaction Cord Blood Fetal Blood Blood Group only RhIG TYPE OF TUBE Red Top Red Top Red Top Red Top Lavender Top Red Top Red Top Red Top Lavender Top Lavender Top Lavender Top Lavender Top Red Top Lavender Top ADULT VOL. (mL) (MINIMUM VOL.) 10 (7) 10 (7) 10 (7) 10 (7) 5 (3) 10 (7) 5 (3) 10 (7) 5 (3) N/A N/A 3 (3) 10 (7) 5 PEDIATRIC VOL. (mL) (MINIMUM VOL.) 5 (3) 5 (3) 5 (3) 5 (3) 3 (1) 5 (3) 3 (1) 5 (3) 3 (1) 5 (3) 3 (1) 3 (3) N/A
For Type and Screens or Crossmatches on newborns (collected by heelstick), a minimum of two full bullets is required
DONOR PROCESSING TEST HIV1/2 HTLVI/II HBsAg RIBA Delta HIV Antigen Western Blot (HIV1 & HTLVI) Viral Marker (Combination Order) PCR
TYPE OF TUBE Red Top Red Top Red Top Red Top Red Top Red Top Red Top Red Top Green Top
ADULT VOL. (mL) (MINIMUM VOL.) 7 (3) 7 (3) 7 (3) 7 (3) 7 (3) 7 (3) 7 (3) 7 (3) 7
PEDIATRIC VOL. (mL) (MINIMUM VOL.) 7 (3) 7 (3) 7 (3) 7 (3) 7 (3) 7 (3) 7 (3) 7 (3)
REAGENTS, SUPPLIES, EQUIPMENT Specimen labels generated by computer Blood Bank Specimen Labeling poster (Appendix I) Specimen Revision / Rejection Form (Appendix II)
SAFETY PRECAUTIONS All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual.
Page 2 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
PROCEDURE 1. Upon receipt of a sample, check to ensure that the following requirements have been met: tube is firmly stoppered. label is firmly attached (sticky label is preferred). label information is legible and indelible. label information matches the information on the request. label information includes: Patient full name. Patient Medical Record Number. Date / time drawn. I.D. number of phlebotomist.
When all the above criteria are met, the sample may be processed. 1.1 Log-in sample by Accession Number. This will be the default method for receiving samples and Product orders. Samples should be bar-coded into the application to avoid transcription errors. Open the LOG-IN application and click on the button next to Accession. Click RETRIEVE and press ENTER. Patient demographics will populate the Demographics field and the specimen information will populate the row of the spreadsheet. A red check mark will display in the row header of the specimen. Enter the correct Collection date, Collection time and Collector ID. If there is more than one order associated with an accession then you will see an ellipsis next to the order. 1.5.1 Click on the ellipsis button to view a list of the tests ordered. Click on the ellipsis button next to Cont/Vol to view the list of containers collected. Click on the DETAILS button to see all details if there is more than a single test associated with the accession.
1.2 1.3
1.4 1.5
1.5.2
1.5.3
If there are tests associated with the accession that are not Blood Bank tests then it is VERY important to only receive the correct sample. 1.5.4 This can be done by only ticking the line associated with the Blood Bank specimen. Clicking the first ticked line will deselect the ticks and allow you to select the desired container. Click on DETAILS again to close.
1.5.5
1.5.6
Page 3 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Page 4 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
1.6
Multiple accession numbers may be entered on the spreadsheet. Patient demographics will change for each entry selected. If all specimens have been entered select a location from the location drop-down box where you want to log the specimen. Click on LOG IN. The status will be changed to Collected and the specimen will be In-Lab. The sample is ready for processing now.
1.7
1.8
2.
Do not receive any sample which: the tube is cracked or broken, compromising the integrity of the sample the label is inadequately attached. the label information is incomplete. has inadequate volume. the specimen date is different than date collected. (patient samples only). the information on label does not match the information on the request. (patient samples only). If patient samples must be rejected for one of the above reasons or if hemolyzed, they must be cancelled in Cerner. 3.1 Click on CANCEL ORDERS to select the patient for whom you want to cancel the order. Alternatively, you can go to TASK and select the CANCEL ORDERS option. 3.2 The top of the screen indicates the mode of Department Order Entry that you are currently in either : Result Entry (default), Cancel Orders or Accession Add On The mode for canceling orders is CANCEL ORDERS. 3.3 Enter the patient MRN. 3.4 Click on the FILTER button, located just beneath the patients name. 3.4.1 This mechanism allows you to choose to search on orders by Laboratory or Radiology. Furthermore, it allows you to search for all encounters associated with the patient or only the encounter you chose in the Encounter Search screen when initially selecting the patient. The column headers will display. Orderable, Order Status, Departmental, Start/Time and Order Details
Page 5 of 95
3.
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3.4.2
These can be arranged into a desired order by clicking on any of the column orders and the system will sort to your selected criteria.
3.5 Select the order you want to cancel and the cancel format will display in the Details section. All fields are highlighted and mandatory. 3.6 The Cancel Reason can be selected from the drop-down box or by typing the first letter of the reason you wish to choose.
3.6.1
At this point it is also essential to add a Chartable Cancel Comment. The cancel reason selected from the drop-down box does not pass to the on-line chart and so a cancel comment needs to be added by clicking the COMMENT icon. This will open a Cancel Reason Dialogue Box, Click EDIT and add a more detailed cancellation reason. This can be viewed in the patients on-line notes attached to the cancelled order and also can be seen in Order Result Viewer.
3.6.2
3.7 Click ADD ORDER TO SCRATCH PAD and then SUBMIT ORDERS, which will process the cancellation. 3.8 Complete a Specimen Revision / Rejection Form (Appendix II) with all the required information. Especially important is the phlebotomist ID number, note this under other on the form. 3.9 Forward to the Quality Assurance Coordinator for follow-up. 4. If the sample does not meet criteria but must be accepted, get Medical Director or Supervisor to approve acceptance. Write a variance report (refer to IPP904). If samples from donors cannot be tested, due to the above reasons, the unit must be discarded physically in and Lifeline with comment stating why the sample could not be tested.
5.
PROCEDURE NOTES 1. The sample should not be drawn from the tubing used for infusion of intravenous fluid or from the contiguous vein, but from a fresh venipuncture site. Sample must be drawn from an arm without I.V. If site not available, draw below I.V. Do not allow nursing staff or phlebotomy staff to re-label improperly labeled specimens. Specimens must be recollected. Do not accept samples for crossmatching and / or Type and Screen if the specimen date is not the same as the date collected.
Page 6 of 95
2. 3.
4.
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Exception: This does not apply to group confirm samples, cord bloods, or samples ordered and drawn close to midnight. The collection date must be handwritten if it doesnt match the specimen date. 5. If computer-generated labels are not available, imprinted labels (e.g. addressograph labels) may be used provided all required information is included. The following items must be handwritten, if they are not included on the addressograph label: The specimen number. Specimen date. Collection time. ID # of the person drawing the specimen. Store crossmatch samples for 14 days, donor clot tubes for 1 month and donor segments for 3 months. Store patient samples for viral marker testing at 1-6C in walk-in refrigerator #10 in bags labeled with date of testing for at least 14 days after testing. Refer to viral marker manufacturer inserts for suitability of sample for testing. If the specimen is improperly labeled, phone floor to explain what is wrong. Send floor a copy of the Blood Bank Specimen Labeling poster (Appendix I). The Blood Bank Quality Assurance Coordinator will forward the Specimen Revision / Rejection Form to Laboratory and Nursing Quality Improvement Coordinators who will initiate the corrective action.
6.
7.
8.
9.
REFERENCE 1. Accreditation Requirements Manual, 6th edition, Washington, DC: American Association of Blood Banks, 1995. Standards for Blood Banks and Transfusion Services, 21st Edition. American Association of Blood Banks, 2002. Technical Manual, 13 Banks, 1999.
th
2.
Bethesda, MD:
3.
Edition, Bethesda, MD:
American Association of Blood
4.
Cerner HNA Millenium Integrated Clinical Information System PathNet User Training st Manual, 1 Edition, King Faisal Specialist Hospital and Research Center, July 2002.
Page 7 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Page 8 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
TITLE / DESCRIPTION:
INDEX NUMBER(S):
GRADING OF AGGLUTINATION REACTIONS
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
624
JAN92
REV8 / OCT01
DP XM
PRINCIPLE The grading of agglutination reactions will be standardized among the members of the Blood Bank staff in the interest of uniformity and reproducibility of test results. Scoring of reactions will only be used for antibody titration.
POLICY All Blood Bank staff will assign numerical values (grades) to reactions observed. Score values will be assigned for antibody titrations. Correct grading will be verified for each staff member during their annual competency assessments.
REAGENTS, SUPPLIES AND EQUIPMENT Agglutination viewer Microscope
SAFETY PRECAUTIONS All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual.
PROCEDURE 1. Spin the cell / serum mixtures at a time appropriate to the calibration of the centrifuge (refer to time posted on the centrifuge being used). Observe for presence of hemolysis. Gently shake the tube and disrupt the cell button in the tube. Observe the cells as they disperse.
2. 3. 4.
Page 9 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
5.
If agglutination is present, record the reactivity by comparing the agglutinates to descriptions in the table under Reporting Results. Record the results of the test immediately after observations are made.
6.
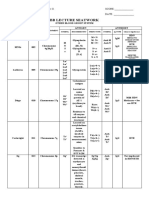
REPORTING RESULTS SCORE VALUE
GRADE H PH 4+ 3+ 2+ 1+ W M
APPEARANCE Red supernatant, few or no intact red cells. Pink supernatant, some intact red cells. A single agglutinate. No free cells detected. Clear background. Strong reaction. A number of large agglutinates. Clear background. Large agglutinates in a sea of smaller clumps. Clear to slightly cloudy background. Numerous small agglutinates. Cloudy red background. Very small agglutinates easily dispersed. Cloudy red background. Macroscopically: appears negative. Microscopically: A few agglutinates in most fields.
12 10 8 5
PROCEDURE NOTES 1. Serum surrounding the centrifuged cell button must be observed for hemolysis. Hemolysis is generally regarded as a positive reaction, but may be the consequence of bacterial or chemical contamination and should not be interpreted as a positive result without further investigation. Most often, antibodies capable of producing hemolysis have specificity in the ABO, P, Lewis, Kidd, or Vel blood group systems. Mixed field reactions (small medium aggregates in a field of otherwise unagglutinated cells) should be noted as such, as well as graded e.g. 2;MF.
2.
REFERENCES 1. Technical Manual, 13th Edition. Bethesda, MD: American Association of Blood Banks, 1999. Rudman, Sally V, Textbook of Blood Banking and Transfusion Medicine. Philadelphia, PA: W. B. Saunders Company, 1995.
2.
Page 10 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
TITLE / DESCRIPTION:
INDEX NUMBER(S):
REAGENT QUALITY CONTROL
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
760
SEP91
REV4 / JAN99
(Reviewed OCT01)
XM
PRINCIPLE Blood Bank reagents are subject to extensive quality control testing by the manufacturer, but factors such as duration of storage, severe changes in temperature and contamination during usage may affect the integrity and performance of the product. Daily Quality Control testing is performed to confirm that reagents are giving expected results and to provide a means to recognize deteriorating potency or reactivity of reagents. POLICY In accordance with AABB Standard 5.1.3 and Code of Federal Regulations Title 21 Part 606.65(c), quality control of reagent red blood cells and antisera will be performed on each day of use. Records of this quality control testing will be retained for five years in compliance with AABB Standard 6.0. REAGENTS, SUPPLIES, EQUIPMENT 1. Gamma RQC Kit, consisting of: A1B D-negative cells 3-4% in Alsevers solution O D-positive cells 3-4% in Alsevers solution Antibody reagent - polyclonal / monoclonal antibodies in 6% bovine albumin Routine blood grouping reagents, consisting of: Anti-A, Anti-B Anti-D A1 and B cells Routine Antibody Detection Reagents, consisting of: Antibody screening cells Antibody enhancement media Antihuman globulin reagent Coombs control cells 6% bovine albumin Equipment: 12 x 75 mm glass test tubes Serofuge and/or automatic cell washer Agglutination viewer 37C heat block or water bath Reagent Quality Control Weekly Record Sheet (Appendix I)
2.
3.
4.
5.
Page 11 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
SAFETY PRECAUTIONS 1. All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual. Do not attempt to pick up broken glass with fingers. Use a dustpan or other scooping implement and dispose of glass fragments in sharps disposal container.
2.
PROCEDURE 1. Locate the Reagent Quality Control Weekly Record Sheet (Appendix I) specific to your reagent rack number in the Daily QC folder. If filling out a new Record Sheet, record RQC lot number, expiry date and rack number at the top. Under "Reagent Identification," record the manufacturer, lot number, and expiry date of the reagents in use in your rack. If any reagents are expired, replace them with in-date reagents. If no in-date reagents are available, refer to Expired Reagents/Products Certification IPP 113. Examine the visual appearance of the reagents in use for hemolysis, turbidity, discoloration, etc. 4.1 If the visual appearance is satisfactory, under "Reagent Appearance mark a tick in the appropriate column. If the visual appearance is NOT satisfactory, under "Reagent Appearance put an X in the appropriate column and replace the reagent. Make a note of the change in the Comment section.
2.
3.
4.
4.2
5. 6.
Record any changes of lot numbers on the blank lines under Reagent Identification. Label ten (10) 12 x 75 mm test tubes from 1 to 10, which will contain the following:
Tube #1 #2 #3 #4 #5 #6 #7 #8 #9 #10 Test Reagent Anti-A Anti-B Anti-D Anti-D A1 cells B cells Screening Cell 1 Screening Cell 2 Screening Cell 3 6% Albumin # drops 1 1 1 1 1 1 1 1 1 1 RQC reagent A1B, D negative cells A1B, D negative cells A1B, D negative cells O, D positive cells Antibody reagent Antibody reagent Antibody reagent Antibody reagent Antibody reagent A1B, D negative cells # drops 1 1 1 1 2 2 2 2 2 1 LISS no no no no no no yes yes yes no # drops 0 0 0 0 0 0 2 2 2 0
Page 12 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
7.
Add one drop of reagent antisera or red cells to be tested to the appropriately labeled tube. Add one drop of the corresponding RQC cells or 2 drops of the RQC Antibody reagent to the appropriately labeled tube. Mix all tubes and centrifuge for time indicated on centrifuge (20 seconds). Examine macroscopically for agglutination and record on the Record Sheet. Grade reactions according to Grading of Agglutination Reactions IPPD 624.) Add two drops of LISS additive to tubes 7, 8 and 9. Incubate tubes 3, 7, 8, 9 and 10 for 15 minutes at 37C. Centrifuge and examine for hemolysis and/or agglutination. Record on Record Sheet. Wash 4 times on automatic cycle in cell washer (CW2), then add 2 drops of anti-IgG AHG reagent. Centrifuge and observe for agglutination macroscopically. Record results on Record Sheet. Add one drop of Coombs control cells to all negative AHG tubes. Centrifuge and examine macroscopically for agglutination. Record results on Record Sheet.
8.
9.
10. 11.
12.
REPORTING RESULTS 1. Interpret results using Record Sheet Expected Rx as a guide. If any results are not acceptable, do not use the reagents. Exchange the reagent(s) in question for a new vial. Repeat the quality control test. If still not acceptable, report to the Senior in Crossmatch. If QC was not done on the previous day or days, write Not In Use in the column(s). When a new lot number of reagent red cells is placed in use, use a new Weekly Record Sheet rather than recording the new numbers on the previous form. On the previous form, write See Other Sheet in the blank spaces. On the new form, write See Other Sheet in the blank spaces. The Senior Technologist will review, date and initial each Record Sheet at the end of each week. Tests performed with these reagents are not valid unless the quality control results are acceptable. Record Sheets will be retained for 5 years.
2. 3.
4.
5.
6.
PROCEDURE NOTES 1. Test each reagent rack each day of use. Make a note on Record Sheet indicating a rack is NOT IN USE for each day the rack is not used. Use a new Weekly Record Sheet at the beginning of each week. Blank forms are in the front of the Daily Reagent QC binder. When there are multiple components within a reagent kit, the components will only be used with kits of the same lot numbers.
Page 13 of 95
2.
3.
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
REFERENCES 1. Accreditation Requirements Manual, 5th edition, Bethesda, MD: American Association of Blood Banks, 1994, pages 23-24. Technical Manual, 13 1999.
th
2.
Edition, Bethesda, MD:
American Association of Blood Banks,
3. 4.
Product Insert, RQC Kit (Reagent Quality Control). Gamma Biologicals Inc. January 1996. Standards for Blood Banks and Transfusion Services, 20 American Association of Blood Banks, 2000.
th
Edition.
Bethesda, MD:
Page 14 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
TITLE / DESCRIPTION: INDEX NUMBER(S):
ABO GROUPING DISCREPANCIES - RESOLUTION
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
702
DEC91
REV12 / AUG02
XM
PRINCIPLE Under most circumstances individuals possess ABO antibodies directed against those ABO antigens absent from their own cells. Discrepancies, however, do occur and may result from technical errors, from intrinsic properties of the red blood cells or from intrinsic properties of the serum. Resolution of ABO problems may depend upon information about the patients age, diagnosis, medication, and history of pregnancy and transfusion.
POLICY In accordance with AABB Standards 5.12.1 and 5.12.2 blood shall not be released for a patient until any discrepancy in patients ABO grouping is resolved. If blood must be transfused prior to resolution of the discrepancy, group O red blood cells will be issued. SPECIMEN Freshly drawn clotted whole blood (Preferred) Anti coagulated (EDTA) specimen
REAGENTS, SUPPLIES, EQUIPMENT Anti-A, anti-B and Anti-AB A1 , A2 and B cells Anti-Human Globulin Screening cells ABO compatible cord serum or plasma Anti-A1 (lectin) Other antisera and neutralizing substances as indicated. Refrigerator (4-6C) Resolution of ABO Discrepancies Worksheet (Appendix I)
SAFETY PRECAUTIONS All blood and blood products must be treated as potentially infectious. precautions detailed in the Laboratory Safety Manual. Follow safety
Page 15 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
QUALITY CONTROL 1. Routine daily quality control of antisera and cells. IPP760. Refer to Reagent Quality Control
2.
All other anti-sera used must be tested against cells positive and negative for the corresponding antigen the same day of testing. All reagent red cells must be checked against the corresponding antisera the same day of testing (refer to Antigen Typing IPP710).
PROCEDURE 1. If the discrepancy exists between a previous blood group and the current group, order a third sample with a new accession number under DEPARTMENT ORDER ENTRY and LABORATORY ORDER ENTRY, and repeat the testing. 1.1. If the new sample confirms the original blood group, the second sample was incorrectly drawn. Complete a variance report with printouts of the testing results. 1.2. If the new sample confirms the discrepancy, refer to the Senior Technologist or Supervisor for resolution. After making printouts of the original testing results and medical record data, remove the historical ABO/Rh. Complete a variance report. 2. If the discrepancy exists between the forward group and the reverse group, obtain patient history including diagnosis, treatment, medications, and transfusions. Then proceed as follows: UNEXPECTED NEGATIVE REACTIONS:
3.
3.1. IN REVERSE GROUP 3.1.1. Repeat the testing of both serum and cells with the following modifications to the reverse group: 3.1.2. Add autocontrol. 3.1.3. Use three to four drops of serum per tube. 3.1.4. Incubate for 30 min. at RT, then if negative, 15 minutes at 4 C. 3.1.5. Read microscopically, comparing result against autocontrol. 3.2. IN FORWARD GROUP 3.2.1. Repeat the testing with the following modifications: 3.2.2. Wash patient cells 2-3 times. 3.2.3. Test with different antibody source. 3.2.4. Incubate for 30 min. at RT, then if negative, 15 minutes at 4 C.
o o
Page 16 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3.2.5. Read microscopically, comparing result against negative saline control. 3.2.6. Look for mixed field and evidence that the patient has been transfused with group O blood. 3.2.7. Absorb/elute with human source reagents may help to establish true group. 4. UNEXPECTED POSITIVE REACTIONS 4.1. IN REVERSE GROUP 4.1.1. Incubate reverse group reactions for 5 minutes at 37 C to dissipate any cold non-significant reactivity. 4.1.2. Perform antibody screen, including auto control. 4.1.3 If all screening cells are positive including the positive control
o
4.1.3.1 If AHG phase is negative, suspect rouleaux 4.1.3.1.1 Repeat positive reactions and read using saline replacement technique (Technical Manual 13th Ed). 4.1.3.2 If AHG phase is positive, an autoantibody may be present.
4.1.3.2.1 If cold autoantibody, prewarm the cells and serum at 37C prior to testing. 4.1.3.2.2 Autoabsorb serum with autologous cells and repeat reverse group, antibody screen and crossmatch. [See W.A.R.M. (Warm Autoantibody Removal Medium) IPP781]. 4.1.4 If one or more screening cells are positive
4.1.4.1 Suspect unexpected antibody in serum. Perform antibody identification according to Antibody Identification Basic Panel IPP 707. 4.1.4.2 Type A cells and B cells used in the reverse typing for the corresponding antigen. 4.1.4.3 Repeat reverse group with: 4.1.4.3.1 A and B cells negative for corresponding antigen OR 4.1.4.3.2 Serum neutralized with appropriate neutralizing substance. 4.1.5 If screen is negative
4.1.5.1 Suspect presence of Anti-A1 4.1.5.2 Test serum against A2 cells. Incubate for 5 minutes. 4.1.5.3 Centrifuge at calibrated spin time and read macroscopically.
Page 17 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
4.1.5.4 If Anti-A1 is identified type patient with anti-A1 (refer to Antigen Typing IPP 710). 4.2. IN FORWARD GROUP 4.2.1 4.2.2 Wash patient cells 3 times with warm saline (37C) and repeat testing. If Test Results Now Coincide With Reverse Group
4.2.2.1 Results caused by cold agglutinin or rouleaux. 4.2.3 If Test Results Are Still Discrepant
4.2.3.1 Repeat test with different source reagents. 4.2.3.2 Suspect acquired B if the patient is group A. 4.2.3.3 Perform DAT. Suspect protein-induced agglutination if the DAT is positive. Look for mixed field agglutination due to blood group chimera, recent transfusion, contamination of sample, recent bone marrow transplant. 4.2.3.4 Retest with fresh ABO compatible human adult and cord serum. If the adult serum is positive and the cord serum negative suspect polyagglutinable RBC.
REPORTING RESULTS 1. Record the initial reactions observed on the Resolution of ABO Discrepancies worksheet (Appendix I) under Initial Blood Group Reactions. Record any repeat testing performed, on a new specimen or treated specimen (e.g. prewarmed or absorbed) or if alternative reagents (e.g. human source vs. monoclonal, or antigen typed reverse cells) are used, on the worksheet under Repeat Testing after Sample Change / Modification. The initial results will indicate what repeat testing is required, if any. Record the results of an antibody screen or anti-A1 identification on the worksheet in the appropriate places. If a further panel is required, attach the completed panel sheet to the worksheet and record the antibody identified on the worksheet. Complete and leave the discrepancy worksheet and any panel sheets or antigen typing forms for Senior review. All work will be reviewed by Supervisor and Blood Bank physician prior to filing in Immunohematology binders. Enter final results in computer under BLOOD BANK RESULT ENTRY and the accession number. Enter reactions with Anti-A, Anti-B, A1 Cells, and B Cells and the ABO interpretation in the computer. Enter free text comments, by selecting the COMMENTS icon, as necessary to explain the additional procedures used to obtain the final results. If anti-A1 is identified, enter results under antibody screen interpretation. Enter antigen typing into computer according to Antigen Typing IPP 710.
2.
3.
4.
5.
6.
Page 18 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
PROCEDURE NOTES 1. Eliminate technical errors by repeating the test with strict adherence to proper procedure and technique. Use quality controlled reagents, appropriate positive and negative controls, careful observation, recording and interpretation of reactions. Until correct ABO group can be determined, the patient must be transfused with O cells (if additional sample is required for investigation, have it collected prior to transfusion). In most cases, the correct ABO group of a patient can be determined once the causes of discrepancies have been recognized and resolved or interpreted correctly. Problems that cannot be resolved after investigation should be referred to the supervisor. Recorded discrepancies (e.g. following bone marrow transplant, immunosuppressed children etc.) do not require reinvestigation each time a specimen is received. Enter identification of anti-A1 under antibody screen results. Refer to AABB Technical Manual (latest edition) for help with difficult resolutions.
2.
3.
4.
5. 6.
REFERENCES 1. Technical Manual, 13 Edition, Bethesda, MD: American Association of Blood Banks, 1999. Standards for Blood Banks and Transfusion Services, 21st Edition. American Association of Blood Banks, 2002. Bethesda, MD:
th
2.
3.
Cerner HNA Millenium Integrated Clinical Information System PathNet User Training st Manual, 1 Edition, King Faisal Specialist Hospital and Research Center, July 2002.
Page 19 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
TITLE / DESCRIPTION:
INDEX NUMBER(S):
ANTIBODY SCREEN
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
706
DEC91
REV10 / AUG02
XM
PRINCIPLE Immunization to foreign red cell antigens may occur through pregnancy, transfusion or deliberate injection with immunization materials. Antibody screening is performed on: 1. Obstetric patients: to identify women with allo-antibodies that might cause hemolytic disease of the newborn. Potential candidates for transfusion: to detect allo-antibodies that might cause a hemolytic transfusion reaction. Donors: to detect allo-antibodies that might cause passive transfer of antibody.
2.
3.
Antibody screening tests allow serum of the patient or donor to react with selected red blood cells under conditions that demonstrate antibodies active at 37C. The antiglobulin phase is required.
POLICY Antibody screens will be performed on all samples received with a request for transfusion, and when specifically requested. In accordance with AABB Standards 5.12.3, samples will be tested by a method that will demonstrate all clinically significant unexpected antibodies. o Pretransfusion testing will include 37 C incubation and an antiglobulin phase using cells that are not pooled. IgG sensitized cells will be added to all antiglobulin tests interpreted as negative. If the patient has been transfused in the preceding 3 months with blood or a blood component containing red blood cells or has been pregnant within the preceding 3 months or if the history is uncertain or unavailable, the sample must be obtained from the patient within 3 days of the scheduled transfusion. Antibodies that are known to exist need not be re-identified; it is necessary to run a selected cell panel to exclude any additional clinically significant unexpected antibodies.
SPECIMEN Serum and cells from 10 mL (minimum 7 mL) clotted whole blood.
Page 20 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
REAGENTS, SUPPLIES, EQUIPMENT 12 x 75 mm glass test tubes Saline (0.9%) LISS additive Anti-human serum globulin reagent Antibody Screening cells IgG sensitized RBC's Serofuge and/or automatic cell washer Agglutination viewer Microscope 37C heat block or water bath Disposable pipettes
SAFETY PRECAUTIONS 1. All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual. Do not attempt to pick up broken glass with fingers. Use a dustpan or other scooping implement and dispose of glass fragments in sharps disposal container.
2.
QUALITY CONTROL Reagent Quality Control IPP 760.
PROCEDURE 1. Place two drops of serum to be tested into three properly labeled test tubes (one tube for each screening cell I, II, III). Add one drop of 2-5% suspension of red cells to the corresponding tube and mix. Add two drops of LISS additive and mix. Incubate at 37C for 15 to 30 minutes in the dri-bath incubator. Centrifuge immediately upon completion of incubation. Examine for hemolysis. Dislodge the cell button and observe for agglutination. Record results in computer. Wash 4 times with saline. After last wash decant completely. Add 2 drops of anti-human globulin reagent and mix. Centrifuge. Examine macroscopically with agglutination viewer for agglutination. Record results in computer.
2. 3. 4. 5.
6. 7. 8.
Page 21 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
9.
To all negative tests, add 1 drop of IgG sensitized red cells. Centrifuge and examine for agglutination. If no agglutination is present, test must be repeated. Record results in computer.
Interpretation of results 1. A negative test indicates that the serum tested has no antibodies that react with the screening cells. When a positive antibody screening result is obtained, proceed with Antibody Identification - Basic Panel IPP 707. When there is a discrepancy between the results of the antibody screening and the crossmatch, (i.e., reagent red cells are positive and the crossmatch is negative, or vice versa) one of the following antibodies may be responsible: 3.1 Anti-H, in the serum of A1 and A1B individuals, may agglutinate all group "O" reagent cells and A2 cells. Group A1 and A1B cells have very little H antigen. Anti-Le Le(b+).
bH
2.
3.
3.2
reacts with group "O" Le(b+) cells, but not with A1 or A1B cells that are
3.3
Anti-A1 in the serum of A2 individuals will test negative with group O cells (antibody screen), while A1 donor cells will be positive (80% of As are A1). Antibody reactive with a low frequency antigen. Low incidence antigens present on screening cells or donor cells cause sporadic positive results. Antibody reactive only with cells homozygous for the corresponding antigen.
3.4
3.5 4.
If a negative result is obtained when the presence of an antibody is suspected, one of the following enhancement methods may be used: 4.1 4.2 4.3 Enzymes: use Ficin Panel (see Antibody Identification Ficin Panel 708). Increased incubation time: Do not incubate more than 30 minutes with LISS. Increased ratio of serum to cells: Do not do this with LISS.
REPORTING RESULTS 1. 2. 3. See procedure for Grading of Agglutination Reactions IPP 624. Record all results as soon as they are read. Record results in the computer under BLOOD BANK RESULT ENTRY. 3.1.1 Complete the New Worksheet Dialogue box. Select the accession number format, optionally name the worksheet and press OK. Enter the accession number associated with the Antibody Screen procedure to be resulted.
Page 22 of 95
3.1.2
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3.1.3
The system will retrieve the order information and reference data for use in the worksheet. When this data has been displayed, you can enter additional accession numbers. Click on, or use the arrow key to move to the first cell to be resulted, represented by a white cell in the worksheet. Enter or select a result from the list. To enter a result, type the first letter or number associated with the result (e.g. type 1 for 1+, n for Not Performed) or click the down arrow key to display the list of options.
3.1.4
3.1.5
3.1.6
3.2 Press ENTER to move to the next result cell. 3.2.1 For negative antibody screens, the system will automatically interpret the AB Screen Interpretation. For positive antibody screens, or incomplete antibody screen results, the AB Screen Interpretation will not automatically interpret and a warning Pattern match not found will be displayed. The result of the AB Screen Interpretation will have to be entered manually either by: 3.2.4 3.2.5 Typing the first letter of the result, N-Negative or P-Positive or Using the drop down box and selecting the result
3.2.2
3.2.3
The system will display the Blood Bank Exception dialogue box. To accept the result, select YES in the Override group box, then select a reason for the override and Click OK to return to Result Entry. Click PERFORM or VERIFY to save the results.
3.10 4.
The Coombs Control cell results must be weakly positive (1+ or 2+). Repeat any test that is negative with Coombs Control cells.
PROCEDURE NOTES 1. Although the minimum incubation time quoted for the Ortho Antibody Enhancement o Solution (LISS) is 10 minutes at 37 C, incubate for a minimum of 15 minutes as Dri-baths are not thought to heat as quickly as waterbaths. The specimen expiration time may be extended for up to 7 days if it is certain the patient has not been transfused or pregnant in the past 3 months. Do not rely on computer transfusion history as the patient may have been transfused elsewhere or have been pregnant. This is an exception that requires the Medical Directors approval.
2.
Page 23 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
LIMITATIONS OF PROCEDURE 1. Using LISS additive, the ionic strength of the test system is dependent on the amount of serum used. Therefore it is not acceptable to increase the serum-to-cell ratio as it will increase the ionic strength and weaken the sensitivity.
REFERENCES 1. AABB Technical Manual, 13th Edition. Bethesda, MD: American Association of Blood Banks, 1999. Standards for Blood Banks and Transfusion Services, 21st Edition. Bethesda, MD: American Association of Blood Banks, 2002. Cerner HNA Millenium Integrated Clinical Information System PathNet User Training st Manual, 1 Edition, King Faisal Specialist Hospital and Research Center, July 2002.
2.
3.
Page 24 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Page 25 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
TITLE / DESCRIPTION:
INDEX NUMBER(S):
CROSSMATCH
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
722
DEC91
REV12 / AUG02
XM
PRINCIPLE The crossmatch is an in-vitro procedure to determine serologic compatibility between the donor's red cells and the recipient's serum. This is accomplished by adding a suspension of donor cells to the recipient serum and observing for agglutination and/or hemolysis in the various phases. Massive transfusion is defined as infusion, within a 24-hour period, of a volume of blood approaching or exceeding replacement of the recipients total blood volume (approximately 10 units). So little is left of the patients original blood that complete crossmatching has little or no benefit.
POLICY Prior to issuing blood, the patient history must be reviewed, and the review documented, to compare current ABO/Rh with historical results and to check for history of antibodies or severe reactions. In accordance with AABB Standards 5.13.1.1, an immediate spin crossmatch is acceptable for patients with no currently detectable or history of previously identified clinically significant antibodies. The following antibodies are considered clinically insignificant and require immediate spin a b a a crossmatching only: P1, M, N, Le , Le , Sd , Bg , and A1, if they are only reactive at the immediate spin phase OR if they become negative upon prewarming the 37C and the AHG o phases. If these antibodies are still reactive at 37 C or AHG phase using a prewarming technique, they will be considered clinically significant and therefore antigen negative, full crossmatch compatible units are required. Patients with currently detectable or previously identified clinically significant antibodies must receive full crossmatch compatible antigen negative units. Patients who have received RhIG will have full crossmatch compatible units while the anti-D is detectable, once the anti-D is no longer detectable, an immediate spin crossmatch is acceptable. In accordance with AABB Standards 5.15.4 and internal policies, massively transfused patients will receive ABO compatible blood which is antigen negative for any existing or pre-existing antibodies. The unit group will be confirmed prior to issue and normal crossmatch procedure will be resumed once a 24-hour period has elapsed since the massive transfusion protocol was initiated.
Page 26 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
SPECIMEN See IPPs 610 - Specimen Receipt- and 787 - Pretransfusion Testing - for specimen labeling and request requirements and acceptance criteria Serum and cells from clotted whole blood: obtained from patient within 3 days of scheduled transfusion. Donor cells from segment originally attached to the unit being crossmatched.
REAGENTS, SUPPLIES, EQUIPMENT 12 mm x 75 mm glass test tubes Disposable Pasteur pipettes Saline (0.9%) Anti-Human Serum IgG Sensitized RBC's Serofuge and/or Automatic Cell Washer Agglutination Viewer Microscope 37C Heat Block or Water Bath LISS additive Polyethylene Glycol (PEG)
SAFETY PRECAUTIONS 1. All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual. Do not attempt to pick up broken glass with fingers. Use a dustpan or other scooping implement and dispose of glass fragments in sharps disposal container.
2.
QUALITY CONTROL See Reagent Quality Control IPP760
PROCEDURE 1. Immediate Spin Crossmatch Note: If the patient has currently detectable or a history of clinically significant antibodies (see Procedure Note 1) the Immediate Spin crossmatch is NOT sufficient. Perform a full crossmatch. The immediate spin crossmatch is intended to detect ABO incompatibility. Do not use for neonates (less than 4 months of age) or patients with current reverse type interpretations of less than 2+; instead perform a Group Check on the unit.
Page 27 of 95
Note:
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
1.1
Place 2 drops of recipient serum in a properly labeled test tube (1 tube for each unit to be crossmatched). Add 1 drop of 3-5% saline suspension of donor red cells. Mix. Centrifuge immediately. Examine for hemolysis. Dislodge the cell button and observe for agglutination macroscopically. Record the results in the computer.
1.2 1.3
2.
Coombs (AHG) Crossmatch Note: If the patient has currently detectable or a history of clinically significant antibodies (see Procedure Note 1) the Immediate Spin crossmatch is NOT sufficient. Perform a full crossmatch on units lacking the corresponding red cell antigens. Refer to Antigen Typing IPP 710.
2.1
Make a 3-4% twice-washed donor red cell suspension. 2.1.1 Place 4 drops of donor whole blood from segment into a test tube. Fill the test tube with 0.9% normal saline and mix gently with a pipette. Centrifuge for 20 30 seconds. Aspirate and discard the saline supernatant, leaving donor red cells in the test tube. Repeat steps 2.2.2 to 2.2.4 for the second wash. Add 0.9% normal saline to the donor red cells making a 34% red cell suspension.
2.1.2
2.1.3 2.1.4
2.1.5 2.1.6
2.2
Place 2 drops of recipient serum in a properly labeled test tube (1 tube for each unit to be crossmatched). Add 1 drop of 3-4% saline suspension of twice-washed donor red cells. Mix. Spin and observe for agglutination or hemolysis. Read and record results. Add 2 drops of LISS additive. Incubate at 37C for 15 to 30 minutes. Centrifuge immediately upon completion of incubation. Examine for hemolysis. Dislodge the cell button and observe for agglutination macroscopically. Record results in computer. Wash 4 times with saline. After last wash, decant completely. Add 2 drops of anti-human globulin and mix.
2.3 2.4 2.5 2.6 2.7
2.8 2.9
Page 28 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
2.10 Centrifuge. Dislodge the cell button and examine macroscopically for agglutination or hemolysis using the agglutination viewer. Record results in the computer immediately after reading. 2.11 To all negative tests, add 1 drop of IgG sensitized red cells. Centrifuge and examine macroscopically for agglutination. If no agglutination is present, test must be repeated.
3.
Massive Transfusion 3.1 If the patient's antibody screen is negative, and 10 units of red blood cells have been transfused in a 24 hour period, group checks (typing with antiA and Anti-B) may be performed on ABO compatible red cells (IPP 754) for all subsequent crossmatches requested in association with the indate specimen. 3.1.2 For ABO compatible units that have been typed as in 3.1, result in the computer as GP CHK.
3.2
After a lapse of 24 hours from the time the massive transfusion protocol was initiated, a new Type and Screen must be requested and tested irregardless of there being an indate Type and Screen specimen. The first 10 units using this specimen must be tested for serological compatibility as dictated by the patients serologic history. If the specimen outdates before the 24 hours have elapsed, subsequent to the initiation of the massive transfusion protocol, the first 10 units crossmatched on the new specimen must be serologically compatible with the patients serum in association with the patients serologic history. If the patient has a history of clinically significant alloantibodies, full crossmatch is only required on the first 10 units transfused. Additional red cells may be group checked, provided all units are ABO compatible and antigen negative. Exceptions to this must be evaluated and approved by the Blood Bank Medical Director. Dispense the units according to Dispensing Blood Components (IPP746).
3.3
3.4
3.5
REPORTING RESULTS 1. Interpretation: Both hemolysis and agglutination in immediate spin, 37C or AHG phases of the crossmatch indicate incompatibility. Perform further testing according to Antibody Identification - Basic Panel (IPP 707). Enter the unit numbers in the computer for the units being crossmatched. Record reactions in the computer as they are observed. Grade reactions according to Grading of Agglutination Reactions - IPP 624. Save all computer results in the computer.
2.
3.
For each unit found to be compatible for the patient:
Page 29 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3.1
Print a Crossmatch Transfusion Tag hand write the date and the accession # of the specimen in the top right hand corner and attach it to blood bag with mini tach-it. This will be the unit identifier attached to the unit. Place labeled units in Revco #1 in the drawer corresponding to the last digit of the patients medical record number.
3.2
4.
If an ABO retype was performed on the unit instead of an immediate spin crossmatch, result the Immediate Spin crossmatch as GP CHK.
PROCEDURE NOTES 1. A clinically significant antibody is one whose specificity has been known to cause hemolytic disease of the newborn, hemolytic transfusion reactions, or unacceptably shortened survival of transfused red blood cells. The following antibodies are considered clinically insignificant: P1, M, N, Lea, Leb, Sda, Bga, and A1, unless they are reacting at 37C and/or AHG using a prewarm technique (Prewarm Technique IPP 759). Reactions at 37C may be due to carry-over after binding of IgM agglutinins at room temperature. Prewarm crossmatch according to IPP759. If testing is now negative at 37C and AHG, the previous reactions are considered to be due to cold reacting clinically insignificant antibodies. Give priority to 'STAT' crossmatch orders over routine orders. Blood should be available under normal circumstances in one hour. Crossmatch all blood products containing significant amounts of red cells (greater than 2 mL) for compatibility before issue. This includes Leukapheresis products and plateletpheresis. Give random platelets that are bloody to group specific patients if the inventory levels cannot justify discarding them. If the inventory levels are good, discard the blood random donor platelets. Consult the Senior Technologist if there are excessive numbers of bloody random platelets before discarding. Do not use an immediate spin crossmatch for neonates, or patients who have current reverse type interpretation of less than 2+, or in cases where immediate spin crossmatch are positive due to cold agglutinins or clinically insignificant alloantibodies. Since an immediate spin crossmatch is intended to detect ABO incompatibilities, the ABO must be rechecked on the unit by performing a retype (Group Check) on the unit and resulting as IS crossmatch as GP CHK.
2.
3.
4.
5.
6.
5.
Page 30 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
6.
Acceptable blood groups of red cells for transfusion:
FIRST CHOICE ACCEPTABLE ALTERNATE ACCEPTABLE WITH APPROVAL OF MEDICAL DIRECTOR
PT BLOOD TYPE
O pos O neg A pos A neg B pos B neg AB pos AB neg
O pos O neg A pos A neg B pos B neg AB pos AB neg
O neg ----A neg, O pos, O neg O neg B neg, O pos, O neg O neg AB neg, A pos, A neg, B pos, B neg, O pos, O neg A neg, B neg, O neg
----O pos ----A pos, O pos ----B pos, O pos ----AB pos, A pos, B pos, O pos
7.
Rh negative patients may switched to RH positive red cells, only by approval from the Blood Bank Medical Director, during exceptional circumstances. 7.1 Enter a Blood Bank comment in the patients historical records that approval was granted by the Medical Director, for the number of units approved, the date and your ID#. 7.2 The ICIS will allow the crossmatch and dispense of Rh positive units to Rh negative individuals with an override reason.
8. Rh negative patients transfused with Rh positive red cells will be serologically monitored by: 8.1 Performing all subsequent antibody screens with polyethylene glycol (PEG) and low ionic strength (LISS) in parallel until further notice. 8.2 Performing a direct antiglobulin test (DAT) using polyspecific antihuman globulin on all red cell specimens until further notice. 8.3 Performing any additional testing as requested by the Senior and/or Supervisor. 8.4 A comment will be entered into the patients history by the Senior Technologist outlining 8.1.1 to 8.1.3.
Page 31 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
9.
In a normal adult, the volume of blood transfused which is considered to be replacement of the original volume is 10 units of packed red cells. In pediatric cases, the volume will be less but as calculation of that volume is virtually impossible; 10 units of packed red cells is considered the safe cut-off. If there is insufficient serum to perform a crossmatch, perform a group check on the units until a new sample can be obtained. Order the new sample and perform a Type and Screen on the new sample prior to crossmatching units.
10.
LIMITATIONS OF PROCEDURE 1. The crossmatch has many limitations. A compatible crossmatch will not guarantee normal survival of transfused cells, prevent immunization of the recipient, or detect all unexpected red cell antibodies in the recipients serum. An immediate spin crossmatch performed on a patient with low titred or absent isohemagglutinins may or may not detect an ABO incompatibility. Perform group check on the units. Insufficient washing of donor red cells for the full crossmatch procedure may result in false negative reactions due to serum protein interference.
2.
3.
REFERENCES 1. 2. Technical Manual, 13 Banks, 1999.
th
Edition, Bethesda, MD:
American Association of Blood
Standards for Blood Banks and Transfusion Services, 21st Edition. Bethesda, MD: American Association of Blood Banks, 2002. Cerner HNA Millenium Integrated Clinical Information System PathNet User Training st Manual, 1 Edition, King Faisal Specialist Hospital and Research Center, July 2002.
3.
Page 32 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
TITLE / DESCRIPTION:
INDEX NUMBER(S):
ANTIBODY IDENTIFICATION - BASIC PANEL
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
707
DEC91
REV9 / JUL01
(Reviewed JUL02)
XM
PRINCIPLE When an antibody is detected in patient serum by a positive antibody screen or an incompatible crossmatch, and/or is eluted from red cells, a panel of red cells of known antigenic configuration is used to identify the antibody. Determining the specificity of antibodies encountered in pretransfusion testing is important in assessing the need to select antigen-negative blood for transfusion. In prenatal testing, knowing the specificity and immunoglobulin class of an antibody helps predict the likelihood of HDN. The serum is tested at all test phases at which antibody activity was initially detected. Additional antibodies may become apparent at different test phases, and the reactivity of some antibodies may be increased by altering incubation time and / or temperature, serum/cell ratio, or by using additive solutions. POLICY A full reagent red cell panel is performed as the initial investigation for all patients who have a positive antibody screen, including Rhig, and no history of previously identified antibodies. Test as many reagent red cells as necessary to confirm or exclude antibody specificities. At least three positive homozygous cells are required to confirm an antibody on its first presentation. For patients with previously identified antibodies, including previously identified Rhig, serum is tested against a selected cell panel of antigen negative cells to exclude any additional clinically significant antibodies. Previously identified antibodies need not be re-identified. All clinically significant antibodies on panel sheet are excluded using a cell with homozygous expression of the corresponding antigen when available, or with two heterozygous cells when homozygous is not available. An auto control is run with all serum panels. SPECIMEN Serum and cells from 10mL (min. 7mL) clotted whole blood Eluate
Page 33 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
REAGENTS, SUPPLIES, EQUIPMENT 12mm x 75 mm test tubes Pasteur pipettes 0.9% saline LISS additive (Ortho Antibody Enhancement solution) Anti-human globulin reagent IgG Sensitized red cells Commercially prepared red cell panel and corresponding panel sheet Immunohematology Report form (Appendix I) Reagent Red Cell Panel; Negative Auto Control Flow Sheet (Appendix II)
SAFETY PRECAUTIONS 1. All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual. Do not attempt to pick up broken glass with fingers. Use a dustpan or other scooping implement and dispose of glass fragments in sharps disposal container.
2.
QUALITY CONTROL Reagent Quality Control IPP760. PROCEDURE 1. 2. Select an indate panel from Jewett refrigerator #5. Select a copy of the panel sheet with the lot number that matches the lot number of the panel cells. Fill in essential information on the panel sheet: Date of testing, Tech ID # Patient name and medical record number Phases of testing, additive and conditions: IS = Immediate Spin phase 37 = 37oC incubation phase AHG = Antihuman globulin phase CC = Coombs Control (or Check Cells) Ficin = Ficin Neat = No additive LISS = LISS additive (Others as indicated)
NEW ANTIBODY
Page 34 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
1. Select appropriate cells for testing. This must be an 11- cell panel at the very minimum. 2. Label reagent red cell tubes with patient identification. Label the last tube "AC" (Auto Control). 3. Place 2 drops of patient's serum in each of the tubes. 4. Gently mix the panel cells well. Add 1 drop of reagent red cells to the labeled tube, Mix well. 5. Prepare a 2-5% cell suspension of the patients own cells using saline. Add 1 drop of this cell suspension to the auto control tube. 6. Centrifuge all tubes in a properly calibrated centrifuge (saline spin time is designated on specific Serofuge or cell washer). 7. Examine for hemolysis and record if present. Gently resuspend the cell button and examine for agglutination macroscopically. Record results in the immediate spin column on the panel sheet. 8. Add 2 drops of LISS Additive to each tube and mix well. (Do not add LISS when testing eluates or if an enzyme panel used). 9. Incubate the tubes for 15 minutes at 37oC. Incubation can be extended for up to 30 minutes for greater sensitivity. 10. Centrifuge as before. Examine for hemolysis and record if present. Gently resuspend the cell button and examine for agglutination macroscopically. Record results in the 37 o C column on the panel sheet. 11. Wash all tubes 4 times with saline. After last wash decant completely. 12. Add 2 drops of anti-human globulin reagent and mix. 13. Centrifuge. Gently resuspend the cell button and carefully examine for agglutination macroscopically. Record results in the AHG column on the panel sheet. 14. To all negative tests, add 1 drop of IgG-sensitized red cells (Coombs control cells). Centrifuge and examine for agglutination. Record results in the CC column on the panel sheet. If no agglutination is present, test must be repeated. INTERPRETATION: Interpret positive and negative results according to the following table: Test Result: Definition: Positive Result Negative Result
Absence of hemolysis or Agglutination or hemolysis in agglutination. immediate spin or incubation phase, or agglutination in antiglobulin phase. Absence of detectable antibodies Indication: Presence of one or more antibodies to antigens present on the cells. directed at antigens present on the particular cells. Grade reactions and record on panel sheet according to Grading of Agglutination
Page 35 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Reactions - IPP624. Refer to Flow Sheet (Appendix II) for interpretation of patterns of reactivity and suggestions of further testing to perform.
If a pattern of positive and negative reactions is observed, antibodies can be eliminated to the antigens present on the non-reactive cells. Using the panel sheet and considering one cell at a time, eliminate all of the antigens that are represented homozygously on the cells giving negative reactions. Cross out the antigens at the top of the page. 3.1 3.2 All Rh Negative individuals with positive antibody screens will have Anti-D, Anti-C and Anti-E ruled out / differentiated by testing an Ro, rr, and rr reagent red cell with PEG. Additional alloantibodies may be excluded using these cells if the corresponding antigen is in the homozygous state of expression.
3.3 LISS additive will be used for additional exclusions using the applicable zygosity rules. 4. If only one antigen is remaining: 4.1 Observe the overall pattern of positive and negative cells to see if the pattern of serum reactions matches that of the positive cells of that antigen. 4.1.1 4.1.2 4.2 If a match is observed and there are a minimum of 3 positive and 3 negative cells, the antibody has been identified. If there are not 3 positive and 3 negative cells, select additional cells.
Antigen type the patient for the corresponding antigen according to Antigen Typing IPP 710. 4.2.1 4.2.2 4.2.3 If an Rh antibody has been identified, perform a full Rh phenotype. If the antigen has an allele, type for both alleles. The patient should be negative for the antigen that the antibody is directed against. If the patient has been transfused in the past 3 months, phenotyping may not be reliable due to the presence of transfused cells.
5.
Reaction phase: 5.1 5.2 Reactivity at room temperature indicates the presence of a cold reacting antibody to M, N, P, or Lewis system antigens, (for example). Reactivity at 37oC and AHG indicates the presence of a warm reacting antibody such as those reacting to S, s, Rh, Kell, Duffy or Kidd system antigens.
6. 7.
If more than one antigen is remaining, refer to Extended Workup in this IPP. Auto Control: 7.1 If the serum reacts with both the panel cells and the autologous cells, this suggests the presence of an autoantibody, but does not exclude an alloantibody.
Page 36 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Auto absorption may be necessary to rule out the presence of coexisting alloantibodies. See Adsorption Technique IPP 703. 7.2 If the autocontrol is positive in the AHG phase, perform a DAT according to Direct Antiglobulin Testing IPP 728. If DAT is positive, perform an eluate according to Elution Acid (Elukit) IPP 704. If the patient has been recently transfused, a mixed-field reaction in the Auto Control and DAT may be seen, indicating an alloantibody directed at an antigen present on surviving donor cells.
7.3
8.
Dosage: 8.1 Some antibodies react stronger or only with cells homozygous for the corresponding antigen. Anti-M, anti-c, anti-Jka often show dosage.
9.
Antibody to high frequency antigen: 9.1 Reactivity with all cells except the patient control cells may indicate reactivity to a high frequency antigen. High frequency antigens usually react with equal strength against all cells tested. It may be useful to test the patients serum against red cells from siblings and other first degree relatives in the search for compatible blood.
10.
Panagglutination: 10.1 10.2 10.3 Equal strength reactivity with all cells, including the patient control cells, indicates non-specific panagglutination activity. Perform auto adsorption according to Adsorption Technique IPP 703 to rule out underlying alloantibodies. Additive solutions or Ingredients in preservatives in reagent red cells may cause reactivity with some patients, which may be reduced by eliminating the additive, using a different additive, or washing the reagent cells prior to use.
11.
Phase of reactivity: 11.1 Take into account the known characteristics of antibody reactivity. For example, if immediate spin reactions seem to correspond to an anti-Fya, it should not be considered as the first choice, because its optimum phase of reactivity is AHG phase.
EXTENDED WORKUP 1. Perform a selected cell panel by choosing additional cells to include cells both positive (homozygous) and negative for each of those antigens not excluded. 1.1 Consider the possibility of antibodies to additional antigens other than the obvious ones that are not ruled out in its presence. For example, if the reactions correspond to an anti-c and all E positive cells are also c positive, the presence of anti-E cannot be ruled out. Select cells from other red cell panels that are c negative and E positive and repeat the tests. Anti-c frequently occurs with anti-E and anti-e with anti-C. 1.2 Similarly, an anti-c may conceal the presence of an anti-K or other antibody. Select cells negative for c antigen and positive for the questionable antigen.
Page 37 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
2. If the observed pattern does not fit any specific pattern, there may be a combination of antibodies present. Perform the following steps to identify and rule out antibodies. 2.1 Antigen type the patient for antigens corresponding to all antibodies not ruled out. A patient will not produce allo-antibodies toward an antigen present on their own red cells. Therefore, if the patients red cells type positive for the antigen, they cannot develop the corresponding antibody and it can be ruled out as an alloantibody. If it appears that Anti-Fya or anti-Fyb is present, run an enzyme panel (see Antibody Identification -- Ficin Panel IPP 708) to detect antibodies that are masked by the anti-Fya or anti-Fyb. If anti-P1 or anti-Le or anti-Le is present, or if anti-Sd is suspected, neutralization (Neutralization with Group Specific Substances IPP753) will frequently confirm an antibody or remove one or more antibodies allowing the identification of others. Adsorption (Adsorption Technique IPP703) and / or adsorption-elution studies (Elution Acid (Elukit) IPP704) can be used to separate specific antibodies.
a b a
2.2
2.3
2.4
3. If a specific antibody pattern isnt demonstrated, it may be due to weak reactivity of the antibody. Weak reactions may be enhanced in several ways: 3.1 3.2 3.3 Increase the incubation time. minutes). (Do not incubate LISS additive longer than 30
Increase the ratio of serum to cells e.g., 4 or 5 drops of serum to 1 drop of cells. (DO NOT use LISS Additive). Perform Dry Button technique: (DO NOT use LISS Additive). 3.3.1 3.3.2 3.3.3 Add one drop of each panel cell to appropriately labeled tube. Wash in cell washer (or Serofuge) for one wash cycle, decant to dry button. Add two or more drops of serum to dry button of cells.
3.4 3.5
Test serum against a FICIN Panel (Antibody Identification -- Ficin Panel IPP708). Use different enhancement reagent -- e.g. PEG, NHance. insert for directions.) (Refer to package
4. An antibody which reacts best at room temperature and decreases in reactivity as the temperature increases is usually considered to be non-clinically significant. These antibodies may mask the presence of a clinically significant warm antibody. Perform a prewarmed panel (Prewarm Technique IPP 759) or autologous adsorption (Adsorption Technique IPP 703) to help detect and identify other antibodies.
Page 38 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
5. If anti-M,N, or P1is identified that reacts at the AHG phase, perform prewarm testing. 5.1 5.2 If the reactivity is eliminated upon prewarming, report the antibody as nonclinically significant. If it is positive in AHG phase after prewarming, report the antibody as being clinically significant.
6. Check for extended typings of panel cells. Some cells will have been typed for less common antigens such as Wra, Chido, etc. and a listing is provided by the manufacturer. PREVIOUSLY IDENTIFIED ANTIBODY 1. From available panels select enough cells which meet the following criteria: Cells that are antigen negative for the previously identified antibody(ies), but positive for all remaining clinically significant antigens. Any additional antibodies that are identified by this process must be confirmed using a total of 3 cells of homozygous expression for the corresponding individual antigen.
2. 3. 4.
Perform an auto control. Previously identified antibodies need not be re-identified. If the panel of selected cells is positive, test additional cells to identify the additional antibody(ies) detected.
EXCLUSIONS USING POLYETHYLENE GLYCOL (PEG) 1. If you incorporate a more sensitive technique into an antibody workup, all alloantibodies should be ruled out using that more sensitive technique. 2. Since liss is our primary potentiator for now, a full panel should be performed using liss. PEG can be used as an alternate, but do not use a combination of liss and peg to perform exclusions on the same panel. Use only one potentiator all the way through your work up. EXCEPTIONS: 3. Rh exclusions in Rh negative (d-) individual most often these people are rr: 3.1 3.2 3.3 Test two r'r cells with PEG to rule out anti-C, if r'r' cell unavailable Test two r"r cells with PEG to rule out anti-E, if r"r" cell unavailable Test one R2R2 cell with PEG to rule out anti-D
Page 39 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3.4
Other alloantibodies may be ruled out on the aforementioned cells if the antigen is in the homozygous state of expression.
4. If a homozygous cell is unavailable to rule out a certain antibody with LISS, test two heterozygous cells with PEG. This would occur most often in multiple antibody situations. 5. If, in the above two situations, an antibody is detected with PEG. Test the same cells with LISS as a comparison. If the same antibody (ies) is non-reactive with LISS, the other exclusions must be repeated using PEG. REPORTING RESULTS 1. Enter Results in Meditech RESULT ENTRY, ENTER RESULTS. At the ABID prompt there is a list of possible panel choices. Enter the results for the methods used as either POSITIVE, NEGATIVE or NP. 1.1. If the initial Antibody Screen has not been resulted and only a rule-out panel is to be performed, order the ABID in Meditech under REQUISITIONS, ENTER/EDIT&RESULT. 1.1.1. Add the Antibody Identification to the existing Type and Screen requisition by performing an <F9> lookup at the REQ # prompt and selecting the current TS order. 1.1.2. At the ORDER prompt order an ABID. 1.1.3 If a new sample is ordered to finish the antibody work up, for the 1st sample ND the antibody interpretation and add to the comment that new sample requested from the ward and add the number of the sample BX# and ND the conclusion too. Use the ABID sample 2 sample to enter the result interpretation for the antibody identification.
nd
1.1.4 2.
At the ANTIBODY INTERP (or ELUATE) prompt press <shift + right arrow key> to obtain the Antibody Interpretation Result Entry Screen. At the ANTIBODY prompt perform an <F9> lookup and select the antibody that was identified. Press ENTER to return to the regular Result Entry screen. Complete Immunohematology Report form (Appendix I) and leave it together with all screening cell antigrams, panel sheets and antigen typing form for senior review. All work will be reviewed by supervisor and pathologist prior to filing in Immunohematology binders. In Meditech, order Antigen Typing(s) and result according to Antigen Typing IPP 710. Print a new file card. For patients with previously identified antibodies: If the panel of selected cells is negative, result as No additional antibodies.
3.
4. 5. 6.
Page 40 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
7.
For patients who have received RhIg and whose selected panel is negative, result as RHIG- Passive Anti-D. Under HISTORY / EDIT BBK HISTORY, enter the date the RhIg was last given.
PROCEDURE NOTES 1. Grade reactions and record on panel sheet according to Grading of Agglutination Reactions IPP624. 2. If the specificity and identification is in some doubt, calculation of probability can be performed using Fisher's Exact Method employing a 2 x 2 table (AABB Technical Manual)
3. It is sometimes impractical to perform exclusions using cells with homozygous expressions of certain antigens. It is acceptable to exclude Anti-K using two heterozygous cells and for patient with anti-D, to exclude Anti-C and Anti-E using two heterozygous cells. Use two heterozygous cells any time a homozygous cell is not available. 4. It is acceptable not to eliminate antibodies to low frequency antigens such as Cw Kpa, V, VS, Jsa. 5. A clinically significant red cell antibody is one that shortens the survival of transfused red cells or has been associated with hemolytic disease of the newborn (HDN). Clinically significant antibodies include the Rh antibodies, anti-S, -s, -U, -Lub, -K, -k, -Kpa, -Kpb, Jsa, -Jsb, -Fya, -Fyb, -Jka, - Jkb, -Dia, -Dib, -Doa, -Coa. 6. Other antibodies may occasionally cause shortened red cell survival, such as anti-M or Yta, and therefore must be treated as clinically significant.
7.
If a new sample is required to complete an antibody workup, order it as ABID with a new BX number. Perform an ABO/Rh on the new sample; order ABO/RH on that BX number to have space to record the results in the computer. Repeat one more positive cell, screening cell or selected cells to rule out, and ensure that the 2nd cell, repeated cell, will react as the 1st cells agglutination strength. For multiple antibody workups, only one positive cell needs to be repeated.
8. Use the ABID sample 2nd sample to enter the result interpretation for the antibody identification . 9. If a new antibody is detected on a patient of Dr. Rahman or Dr. Kurdi (OBGYN), perform and result antibody titration without waiting for specific titration order. REFERENCES 1. AABB Technical Manual, 12th edition. Bethesda, MD: American Association of Blood Banks, 1996, pages 349-378. Standards for Blood Banks and Transfusion Services, 21st edition. Bethesda, MD: American Association of Blood Banks, 2002.
2.
Page 41 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3. 4. 5. 6. 7.
Blood Transfusion in Clinical Medicine, P.L. Mollison, 1993. Gamma Ficin-Panel Systems (Panel One), Package Insert. Houston, TX: Biologicals Inc., May 1996. Gamma
Panel Twenty, Package Insert. Houston, TX: Gamma Biologicals Inc., May 1996. Resolve Panel A, Package Insert. Raritan, NJ: Ortho Diagnostic Systems, May, 1989. Resolve Panel B, Package Insert. Raritan, NJ: Ortho Diagnostic Systems, July 1988.
TITLE / DESCRIPTION:
INDEX NUMBER(S):
ANTIBODY IDENTIFICATION FICIN PANEL
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
708
DEC91
REV10 / AUG02
XM
PRINCIPLE The use of ficin pretreated panel cells increases sensitivity in the identification of some blood group antibodies, most notably those of Rh, Kidd, Lewis, & Vel blood group systems as well as cold agglutinins of anti-I specificity. Ficin treated cells will not react with most samples of antia b a Fy , -Fy , -M, -N,. Xg , and Pr. Anti-S and anti-s may show loss of specificity when tested with enzyme-treated cells. For this reason the ficin panel is never used alone in identification tests. POLICY The Ficin panel may be used as an aid in the identification of antibodies, either by enhancing or inhibiting antibody reactivity, in the following circumstances: 1. 2. 3. When a pattern of weak reactions fails to indicate specificity. When the presence of an antibody is suspected but cannot be demonstrated. When the depression of a reaction may aid in the identification of antibody mixtures or may confirm the identity of an antibody.
Enzyme treated panels must always be used in parallel with the corresponding untreated panel. SPECIMEN 10mL (min 7mL) serum sample in a red top tube REAGENTS, SUPPLIES, EQUIPMENT
Page 42 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
12 mm x 75 mm test tubes Pasteur pipettes 0.9% saline O 37 C Dri bath Waterproof/permanent marker Anti-human globulin reagent IgG Sensitized red cells Ficin treated panel Ficin treated panel cells Ficin solution Enzyme control reagent
SAFETY PRECAUTIONS 1. All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual. Do not attempt to pick up broken glass with fingers. Use a dustpan or other scooping implement and dispose of glass fragments in sharps disposal container.
2.
QUALITY CONTROL 1. 2. Routine daily quality control of antisera and cells. Enzyme Control Reagent.
PROCEDURE 1. Select an indate ficin panel from Jewett refrigerator #5 with the same lot number as the untreated cell panel used. Select a copy of the panel sheet with the lot number that matches the lot number of the panel cells. Complete the essential information on the panel sheet: Date of testing Tech ID # Patient name and medical record number Phases of testing, additive and conditions: IS 37 = = Immediate Spin phase 37oC incubation phase Antihuman globulin phase Coombs Control (or Check Cells)
Page 43 of 95
2.
AHG = CC =
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Ficin = Neat = LISS =
Ficin No additive LISS additive
(Others as indicated) 3. Prepare controls: 3.1 3.2 3.3 3.4 3.5 Prepare a 3% cell suspension of washed patient cells. Place 2 drops of washed cell suspension into an appropriately labeled tube. Add 2 drops of ficin solution to the tube. Mix well and incubate for 10 minutes at 37C. Immediately wash the treated cells at least 2 times in saline and decant the last wash. Resuspend the dry cell button in 2 drops of Modified Alsevers Solution to provide a 3-4% cell suspension. Confirm the adequacy of ficin treatment by testing as follows: 3.7.1 Place 1 drop of Gamma enzyme control reagent to each of two labeled tubes, e.g. AC for Auto Control and FP for random Ficin-Panel cell. Add 1 drop of the treated auto control cells to AC tube and 1 drop of a random Ficin-Panel cell to the FP tube. Centrifuge for designated saline spin time. Resuspend the cell button and examine for agglutination.
3.6
3.7
3.7.2
3.7.3
3.8
Adequate ficin treatment of the auto control is indicated by agglutination of 2-3+ in both tubes. If the ficin treatment is satisfactory, the remaining drop of ficin treated cells may be used to the auto control tube on the panel.
3.9
4. 5. 6. 7. 8. 9.
Label 12 tubes with patient identification. Label the first eleven tubes with numbers 1-11 for panel cells and the twelfth tube with AC for the patient auto control. Place 2 drops of patient's serum in each of the 12 tubes. Gently mix the panel cells well. Add 1 drop of cell #1 to tube #1, 1 drop of cell #2 to tube #2 and so forth through cell #11. Mix well. Add 1 drop of the ficin treated patient cell suspension to the tube labeled AC, mix well. Incubate the tubes for 15 minutes at 37C. Incubation may be extended to 60 minutes. Centrifuge all tubes in a properly calibrated centrifuge (saline spin time is designated on specific Serofuge or cell washer).
Page 44 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
10.
Examine for hemolysis and record if present. Gently resuspend the cell button and examine for agglutination macroscopically. Record results in the 37C column on the panel sheet. Wash 4 times with saline. After last wash decant completely. Add 2 drops of anti-human globulin reagent and mix. Centrifuge as in #9 above. Gently resuspend the cell button and carefully examine for agglutination macroscopically. Do not read microscopically. Immediately record results on the panel sheet. To all negative tests, add 1 drop of IgG sensitized red cells, mix. Centrifuge as above. Examine for agglutination. Immediately record results in CC column on panel sheet. If no agglutination is present, test(s) must be repeated.
11. 12. 13.
14.
Interpretation: 1. Interpret positive and negative results according to the following table: Test Result: Definition: Indication: Positive Result Agglutination or hemolysis in immediate spin or incubation phase, or agglutination in antiglobulin phase. Presence of one or more antibodies directed at antigens present on the particular cells. Negative Result Absence of hemolysis or agglutination. Absence of detectable antibodies to antigens present on the cells.
Grade reactions and record on panel sheet according to Grading of Agglutination Reactions - IPP624. 2. Antibodies that show increased reactions with ficin treated cells are anti-Rh, -Jk and Jkb, -Lea and -Leb. Anti-I will also show increased reactions. If a serum sample gives positive (or negative) results on a specific cell on the untreated panel and stronger (or positive) results on the same cell on the ficin treated panel it may indicate the presence of one of these antibodies. Antibodies that show negative or diminished reactions with ficin treated cells are anti-M, N, -Fya and -Fyb. Anti-S and -s may show diminished reactions or loss of specificity with ficin treated cells. If a serum sample gives positive results on a specific cell on the untreated panel but negative results on the same cell on the ficin treated panel, it may indicate the presence of one of these antibodies. Enter results under Antibody ID in BLOOD BANK RESULT ENTRY. 4.1 Under the FICIN column, enter or select a result from the list of options.
a
3.
4.
REPORTING RESULTS 1. Report results according to Antibody Identification - Basic Panel (707). On the panel sheet(s) label ficin results clearly to differentiate from untreated cell results.
Page 45 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
PROCEDURE NOTES 1. Do not read results microscopically because the use of enzyme treated cells enhances non-specific reactivity. A positive result in auto control tube indicates the presence of a warm or cold autoantibody and should be referred to Senior Technologist for evaluation.
2.
LIMITATIONS OF PROCEDURE 1. Warm or cold auto agglutination may be enhanced in tests performed with ficin treated cells. Excess ficin or over treatment of cells may cause nonspecific agglutination. The reactivity of the ficin treated red cells may diminish over the dating period.
2. 3.
REFERENCES 1. AABB Technical Manual, 13th Edition. Bethesda, MD: American Association of Blood Banks, 1999. Package Insert, Gamma Biologicals, Reagent Red Blood Cells (Ficin Treated), May 1996. Cerner HNA Millenium Integrated Clinical Information System PathNet User Training st Manual, 1 Edition, King Faisal Specialist Hospital and Research Center, July 2002.
2.
3.
Page 46 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
ANTIGEN TYPINGS
Technologist: ______________ Date: _____________ MR # and Date of Last Transfusion:_____________________
DETAILS Rosette Test Sickle Test Anti-C Anti-E Anti-c Anti-e AntiAntiAntiAntiAnti Computer Entry MT LL
Lot Number Expiry Date POS - Lot No. - Expiry - Cell No. - Result NEG - Lot No. - Expiry -Cell No. - Result
Page 47 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
PAGE No. ______________ REVIEWED BY: _____________________ DATE: ____________________ NOTE: [! ] in same column, indicates negative AHG result confirmed with coombs control cells and found to give acceptable 2+ reaction ICIS DOWNTIME: Entered into ICIS By:________________________ Date___________________
Page 48 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
TITLE/DESCRIPTION:
INDEX NUMBER(S):
ANTIGEN TYPING
EFFECTIVE DATE: REVISION DATE/NUMBER: DISSEMINATION:
710
DEC91
REV10 / AUG02
XM
PRINCIPLE Antigen typing is performed to provide red cell products without the corresponding antigen for patients with clinically significant red blood cell antibodies. Once a clinically significant alloantibody has been identified in a patients serum it is advisable to test the patient red cells for the corresponding antigen as a confirmatory test.
POLICY In accordance with AABB Standards 5.14.3, when clinically significant unexpected red cell antibodies are found or the recipient has a history of such antibodies, whole blood or red blood cell components shall be prepared for transfusion that do not contain the corresponding antigen, and are crossmatch compatible. Exceptions may be made, only when approved by the Medical Director, when clinical circumstances warrant deviation. The following antibodies are considered clinically insignificant: P1, M, N, Le , Le , Sd , Bg , o and A1, and antigen typed units are not required if the antibodies are not reactive at 37 C or AHG. All units must be crossmatch compatible by the method deemed appropriate for the antibody and the phase at which it is reactive. Patients who have one or more Rh antibodies will have their full Rh phenotype determined. Patients with other clinically significant antibodies will have both alleles of the corresponding antigen phenotyped. Patient phenotyping may be performed to aid in identifying and/or excluding antibodies, but should not be done on patients with a recent transfusion history. Red cell phenotypes may be ordered by physicians after consultation with the Blood Bank Director.
a b a a
SPECIMEN 10mL (min. 7mL) clotted whole blood - test as soon as possible, store at 2-8C if testing is delayed.
Page 49 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
REAGENTS, SUPPLIES, EQUIPMENT Commercial blood grouping antisera Antisera directions for use (Package inserts) Isotonic saline Anti-Human globulin reagent Coombs control cells 12 x 75 mm test tubes 37C Dri bath Centrifuge Disposable pipettes Waterproof/Permanent Marker Cell Washer Antigen Typing form (Appendix I)
SAFETY PRECAUTIONS All blood and blood products must be treated as potentially infectious. precautions detailed in the Laboratory Safety Manual. Follow universal
QUALITY CONTROL 1. Test each antisera each day of use with the following: 1.1 Positive Control: a cell with heterozygous (if possible) expression of the antigen it is directed against. Negative Control: a cell negative for the antigen. If appropriate controls cannot be found among the indate screening cells, use outdated panel cells.
1.2
PROCEDURE Refer to package inserts for instructions.
REPORTING RESULTS 1. Record all tests performed, including controls, on the Antigen Typing form (Appendix I) as each test is read. Record the lot number and cell number of all control cells. For patients, record the MR # and Date of the last transfusion. Grade reactions according to Grading of Agglutination Reactions - IPP624. 2. Control all negative tests read in the antiglobulin phase with Coombs Control Cells. Record a tick () in the same column to indicate validation of these results.
Page 50 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3. Interpret antigen type only when positive and negative control cells react with antisera as expected. The positive control should give a minimum reaction reading of 2+ or greater, as defined in IPP 624 Grading of Agglutination Reactions. 4. If the positive control gives a grading of < 2+, it must be repeated with either fresh control cells or another vial or lot number of antisera. Refer the discrepancy to the Senior Technologist, if it can not be resolved. 5. Antisera controls must be performed each day of use. If controls have already been done and recorded on a different antigen typing sheet, record the lot number and expiry of the reagent on the current antigen typing sheet. In place of the control results, record that controls were already performed. 6. Order Antigen Typing(s) in DEPARTMENT ORDER ENTRY under the sample accession number. BMT PHENOs will be ordered by the wards. 7. To result antigen typings select BLOOD BANK RESULT ENTRY. 8. Complete the New Worksheet Dialogue box, select the accession number format for a patient or product number and press OK. 9. Enter the accession number associated with the Antigen Type procedure to be resulted or enter the product number. The Insert Phases/Cells/Interp window will be displayed. 10. Select AG TYPE from the Phase list by using the drop-box and PATIENT or PRODUCT depending on which you are performing, from the Cell list. 11. For BMT Phenotype (Antigen Types), select BMT PHENO from the phase list and also BMT PHENO from the cells list. For BMT Pheno, if all the cells are not going to be required they must be deleted before result verification. 12. The system retrieves order information and reference data for use in the worksheet. When this data has been displayed, you can enter additional accession numbers. 13. Click on, or use the arrow key to move to the first cell to be resulted, represented a white cell in the worksheet. 13.1.1 Enter the antigen that you have tested in the Ag Tested column using free text. Enter or select a result from the drop down list for the R.T, AHG and AHG CC columns. To enter a result, type the first letter or number associated with the result (e.g. 1 for 1+, NP for Not Performed) or click the down-arrow key to display the list of options. by
13.2
13.3
13.4 Press ENTER to move to the next result cell. 14. Enter or select from the list the Antigen Type Interpretation, taking care to select the correct interpretation.
Page 51 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
The Result Entry spreadsheet does not show all the fields to be resulted on the screen in a single view. When you get to the Ag Interp field you will not be able to see the Ag tested box which makes it difficult to follow. To view the Ag tested once you have got to the Ag interp field use the left/right arrow keys to move between fields. 15. Click PERFORM or VERIFY to save the results. 16. The system will then prompt Do you wish to complete the Ag Type 16.1 17. Click YES to complete the antigen type entry.
Enter donor antigen results in Lifeline computer according to Antigen/Sickledex Result Entry In Lifeline IPP 723. Write antigen results on red cell donor unit on upper left hand corner of the label.
18.
PROCEDURE NOTES 1. Read and follow the manufacturers instructions with each lot number of antisera, as the procedure can vary from manufacturer to manufacturer and from lot to lot. Every time a new vial of antisera is opened, sign and date the vial. Label the package insert with the reagent lot number and expiration date and place it in the package insert binder. Remove the previous package insert. A binder of current package inserts is available and is updated monthly. When screening donor units, take antigenic frequency into account. If the antigen is relatively low frequency, negative units will be easily found, e.g. if a patient has anti-K, only a few units will need to be typed as 91% of donors are K negative. If a patient has multiple antibodies, type for the higher frequency antigen first, e.g. if patient has anti-c and anti-E, type for c antigen first since 80% will be unsuitable, then type c negative units for E. Frequency tables for each blood group can be found in the AABB Technical Manual. This should be used only as a guide, as it is not based on Arabian populations.
2.
3. 4.
5.
Page 52 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
LIMITATIONS OF PROCEDURE 1. If a patient is to be antigen typed, samples should be tested prior to transfusion therapy. Patients who have been transfused may have surviving donor cells that can cause mixed field agglutination or false positive or negative reactions. 1.1 1.2 Do not antigen type patients who have been transfused within the previous 30 days. If patient has been transfused within the previous 3 months, interpret the antigen type with caution. Do not do BMT Phenotype if patient has been transfused in the previous 3 months. Cancel BMT Phenotype under DEPARTMENT ORDER ENTRY with cancellation comment of BMT PHENOTYPE NOT DONE; TRANSFUSED WITHIN 90 DAYS
1.3
2.
If a patient has a positive direct antiglobulin test, their cells will give a false positive result when the indirect antiglobulin test is required for antigen typing. Take into account the characteristics of the antigens when antigen typing patients or donor units. The strength of P1 antigen reactivity differs markedly among different cell samples and reactivity declines during storage, thus use of fresh control cells is desirable. Some antigens are not fully expressed on the red cells of infants and young children, these include P1, Lewis and Lutheran antigens.
3.
4.
5.
REFERENCES
1. Manufacturers inserts for each antisera. 2. Issitt, PD. Applied Blood Group Serology, 3rd Edition. Miami, Florida: Montgomery Scientific Publications, 1989. 3. Technical Manual, 13th ed., Bethesda, MD: 1999. American Association of Blood Banks,
4. Standards for Blood Banks and Transfusion Services, 21st Edition. Bethesda, MD: American Association of Blood Banks, 2002. 5. Cerner HNA Millenium Integrated Clinical Information System PathNet User Training st Manual, 1 Edition, King Faisal Specialist Hospital and Research Center, July 2002.
Page 53 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
BLOOD BANK INTERNAL PROCEDURE / POLICY
TITLE / DESCRIPTION: INDEX NUMBER(S):
DIRECT ANTIGLOBULIN TEST (DAT)
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
728
JAN92
REV9 / AUG02
XM
PRINCIPLE The direct antiglobulin test (DAT) demonstrates the presence of antibody bound to red cells in vivo. It is of value in detecting cases of HDN (hemolytic disease of the newborn), auto-immune hemolytic anemia, transfusion reaction and other clinical conditions.
POLICY A direct antiglobulin test (DAT) will be performed on all cord samples and will be provided as a diagnostic tool at the physicians request. All post transfusion samples submitted for transfusion reaction investigation will have a direct antiglobulin test performed on them in accordance with AABB Standards 7.3.3.1.4. A direct antiglobulin test will be performed if the autocontrol performed with an antibody investigation panel is positive.
SPECIMEN Whole blood from patient in lavender top (EDTA) tube, 5 mL
REAGENTS, SUPPLIES AND EQUIPMENT 12 mm x 75 mm disposable glass tubes Normal saline Disposable pipettes Polyspecific Anti-human globulin reagent Monospecific (IgG and C3d) Anti-Human globulin reagents Automatic cell washer or Serofuge IgG sensitized cells (Coombs Control Cells) Microscope Complement Coombs Control Cells Antigen Typings form (Appendix I)
SAFETY PRECAUTIONS
Page 54 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
1.
All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual. Do not attempt to pick up broken glass with fingers. Use a dustpan or other scooping implement and dispose of glass fragments in sharps disposal container.
2.
QUALITY CONTROL 1. 2. Test and record anti-IgG results according to Reagent Quality Control IPP 760. Record polyspecific control results of antihuman globulin and anti-C3d monospecific antihuman globulin on Antigen Typings form (Appendix I) each day of use.
PROCEDURE 1. 2. 3. 4. Make a 3-5% suspension of patient cells in saline. Add one drop of cell suspension to each of three tubes labeled for polyspecific AHG, IgG and C3d. Wash the cells four times using the automatic cell washer. Polyspecific Direct Antiglobulin Testing 4.1 To the dry cell button, add 2 drops of polyspecific antihuman globulin reagent to the appropriately labeled tube. Mix well and centrifuge at calibrated AHG spin time. Immediately resuspend the red blood cells by gentle agitation and examine macroscopically for agglutination. Examine any apparent negative tests microscopically. Record results. If negative, incubate tube at room temperature for 5-10 minutes after the initial reading. Centrifuge and read microscopically, record results. To each negative test, add one drop of Coombs Control Cells and centrifuge for calibrated spin time, then examine microscopically immediately for agglutination. Repeat any negative tests. If a positive result is found with polyspecific AHG, perform monospecific direct antiglobulin testing to determine whether the positive test is due to IgG or complement components bound to the cell.
4.2 4.3
4.4 4.5
4.6
4.7
5.
Monospecific Direct Antiglobulin Testing 5.1 Add two drops of anti-IgG monospecific anti-human globulin reagent into the appropriately labeled tube. Add 2 drops of anti-C3d monospecific anti-human globulin reagent into the appropriately labeled tube.
Page 55 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
5.2 5.3 5.4 5.5
Mix well and centrifuge at AHG calibrated spin time. Resuspend the cell button gently and examine macroscopically for agglutination. Examine any apparent negative tests microscopically. If the DAT is positive with anti-IgG, anti-c3d and polyspecific antihuman globulin, a 6% albumin control must be performed and recorded to rule out the presence of spontaneous agglutination. If anti-C3d is negative, incubate 5-10 minutes at room temperature, spin, read microscopically, record results. To any negative IgG tests, add 1 drop of Coombs Control Cells, centrifuge at calibrated AHG spin time and examine macroscopically for agglutination. Repeat any negative tests. To any negative C3d tests add 1 drop of Complement Control Cells, incubate at room temperature for 5 minutes, spin and examine macroscopically for agglutination. Repeat any negative tests. Enter DAT results under BLOOD BANK RESULT ENTRY.
5.6
5.7
5.8
5.9
REPORTING RESULTS 1. Presence of agglutination, either macroscopically or microscopically, is interpreted as a positive result. Absence of agglutination is interpreted as a negative result. Refer to procedure on Grading of Agglutination Reactions - IPP624. A patient who develops a positive DAT subsequent to recent transfusion may be undergoing a delayed hemolytic transfusion reaction. This possibility must always be considered and if indicated a full transfusion reaction work-up should be performed. Consult the Senior, Supervisor (weekdays) and / or Blood Bank Director (evenings, nights, weekends). In this case, the DAT result is a critical value and the recipient physician should be notified via the Medical Director of the Blood Bank. Refer to Cord Blood Testing - IPP724 for the reporting format for neonate samples.
2.
3.
PROCEDURAL NOTES
1. If anti-IgG gives a positive result, perform an eluate on the cells. (See #4 below for guidelines.
2.
If IgG is negative and only C3d and polyspecific AHG are positive, there is no need to perform an eluate. Polyspecific anti-human globulin testing requires both an immediate spin reading and a room temperature incubation for 5-10 minutes and reading again. A negative reaction will sometimes become positive after this time. This is particularly useful in detecting C3d or IgA sensitization. Positive reactions due to IgG sensitization will often become weaker following this procedure so that reading after 5-10 minutes incubation in antiglobulin serum must never be substituted for the immediate reading.
3.
Page 56 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
4.
If a DAT is positive with anti-IgG, anti-C3d, and polyspecific AHG, a 6% albumin control must be performed and recorded in order to rule out the presence of spontaneous agglutination due to immunoglobulin coating. Some patients with autoimmune disease process have routine DATs requested in order to monitor treatment. If the DAT is positive perform an eluate on first presentation. Following the initial elution, perform an eluate only if: 5.1 5.2 5.3 The DAT or elution has not been done for 6 months. The DAT strength increases significantly (2 or greater agglutination gradings). The patient has been transfused within the past month.
5.
6.
If a DAT is ordered and there is no history of ABO/Rh results in the patients medical record data in computer, order the test ABO/RH on the same accession number, perform ABO/Rh, and enter the results under the same accession number in the BLOOD BANK RESULT ENTRY application.
LIMITATIONS OF PROCEDURE Cells from clotted specimens stored at 4 - 6C temperature may absorb complement which will be detected by the anti-C3d component of polyspecific AHG and by monospecific Anti-C3d. Any positive DAT performed on a clotted specimen must be confirmed on an EDTA specimen.
REFERENCES 1. 2. Technical Manual, 13th Edition, Bethesda, MD: American Association of Blood Banks, 1999. Standards for Blood Banks and Transfusion Services, 21st Edition. Bethesda, MD: American Association of Blood Banks, 2002.
Page 57 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
BLOOD BANK INTERNAL PROCEDURE / POLICY
TITLE / DESCRIPTION: INDEX NUMBER(S):
ELUTION - ACID (Elu-kit)
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
704
DEC91
REV8 / AUG02
XM
PRINCIPLE Elution using the commercial Elu-kit is a procedure for the recovery of antibody from coated red blood cells. 1. Red blood cells coated with antibody are first thoroughly washed in a buffered wash solution to remove all traces of unbound protein. The washed red cells, with antibody still attached, are then suspended in a low pH glycine buffer. After centrifugation, the supernatant containing any dissociated antibody is separated from the red cells. Restoration to near normal ionic strength and pH is achieved by adding a concentrated tris buffer.
2. 3.
POLICY An acid elution will be performed on patient cell samples with positive DAT due to IgG if six months have passed since last elution. Patients with a diagnosis of autoimmune disease and a positive DAT must have an eluate performed on first presentation then every six months thereafter. As well, an eluate must be performed if the DAT strength increases significantly (equal to or greater than 2 agglutination readings), or if the patient has been transfused in the past three months.
SPECIMEN 5mL (minimum 3mL) whole blood in a Lavender Top tube
REAGENTS, SUPPLIES, EQUIPMENT centrifuge normal saline distilled water 12 x 75 mm disposable glass test tubes Pasteur pipettes timer Elu-kit Concentrated Wash Solution: Prepare working wash solution by adding one volume of concentrated wash solution to nine volumes of distilled water. Mix thoroughly before use. Store at 20 - 80C in a stoppered glass or plastic container; good until turbid. Eluting Solution: Low pH glycine buffer
Page 58 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Buffering Solution:
Tris-aminomethane solution to neutralize acidity of eluting solution.
SAFETY PRECAUTIONS 1. All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual. Do not attempt to pick up broken glass with fingers. Use a dustpan or other scooping implement and dispose of glass fragments in sharps disposal container.
2.
QUALITY CONTROL
The purpose of this control test is to assure that antibody present in the eluate has been derived from the bound state on the original cells and is not unbound antibody remaining as the result of inadequate washing.
1. Retain a small sample of working wash solution from the last wash of the coated red cells to test for antibody activity in parallel with eluate. Test the last wash against cells homozygous for antigens of clinical significance. Routine reagent screening cells are adequate for testing last wash. If antibody activity is present in the last wash, repeat the elution procedure after more thorough washing of the cells.
2.
3.
PROCEDURE
Preparing the Eluate
1.1. 1.2. Centrifuge the specimen and remove all excess plasma or serum. Wash the coated red cells once with saline. Wash the cells an additional four times with working wash solution. For each wash, mix well after each addition of working wash solution, centrifuge for one minute, remove supernatant carefully without losing any red cells. Reserve a small aliquot of solution from the last wash to serve as a control (see Quality Control). Place 1 mL (20 drops) of washed red cells in a clean 12 x 75 mm test tube. Add 1 mL (20 drops) of eluting solution and mix gently by inversion four times. Immediately Serofuge for 45-60 seconds. Note: If fewer than 20 drops available, add an equal number of drops of eluting solution. Add the same number of drops of buffering solution. Immediately transfer the supernatant eluate to a clean test tube and discard red cells. Add 1 mL (20 drops) of buffering solution to supernatant and mix well. The eluate should turn light blue. Continue adding additional buffer, one drop at a time with mixing, until it turns blue. Mix well. Centrifuge for one minute to remove any precipitate of cellular debris, then transfer the eluate to a clean and properly labeled test tube.
1.3.
1.4.
1.5.
1.6.
Page 59 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
1.7. 2.
The eluate is now ready for testing to detect or identify antibodies.
Testing the Eluate 2.1. Place 1 drop of a 3-5% suspension of each cell to be tested in a clean, labeled test tube. Add a small volume of physiologic saline (5-10 drops). Centrifuge for 30 seconds at 3,400 rpm (RCF 900 to 1,000), decant the saline and blot the tubes dry. Test A and B cells with the eluate if the patient has received ABO incompatible plasma products or if the patient received an ABO incompatible bone marrow transplant. Add 2 drops of eluate to the dry cell button. Do not add potentiators such as LlSS or albumin. Mix gently to resuspend the cells and incubate for 15 minutes in a 37 C Dribath. After appropriate incubation, add 5-10 drops of working wash solution to the tube and mix. Centrifuge for 30 seconds at 3,400 rpm (RCF 900-1,000). Decant the working wash solution and blot the tubes dry. Without further washing add 2 drops of anti-human globulin and shake to mix. Immediately centrifuge in Serofuge for 15 seconds. Resuspend the cells by gentle shaking, read for agglutination and record test results. To all tubes with negative reactions, add one drop IgG sensitized cells. Centrifuge and read. Record results. If negative, repeat testing starting from step 2.1.
2.2.
2.3.
2.4. 2.5.
2.6. 2.7. 2.8. 2.9. 2.10.
2.11.
3.
Interpretation 3.1. An agglutination reaction, occurring when the eluate is tested against red blood cells of appropriate phenotypes, indicates that an antibody has been recovered from the original cells, subject to satisfactory control tests. The absence of agglutination indicates that no antibody has been recovered from the cells. If the antibody activity is present in the wash saline, or if the wash saline hemolyzes test cells, repeat the elution procedure after more thorough washing of the cells.
3.2.
3.3.
REPORTING RESULTS
1.
2. 3.
Record graded reactions on panel sheet. Record that it is an eluate being tested and type of eluate. Record specific phase of test reactions, e.g. IgG.
If serum panels are included on the same sheet, clearly label results as serum. Record results of control (last wash) on panel sheet. Page 60 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
4.
5. 6.
7. 8. 9. 10.
Order an ELUATE, ACID and enter results under BLOOD BANK RESULT ENTRY by entering the sample accession number and selecting PATIENT under CELL in the dialogue box that appears. Click on, or use the arrow key to move to the first cell to be resulted, represented by a white cell in the worksheet. Enter or select a result from the list. To enter a result, type the first letter associated with the result (e.g. N for negative, NP for Not Performed) or click the down arrow key to display the list of options. Press ENTER to move to the next result cell. Enter or select the overall interpretation of the Eluate panel. All eluate interpretations begin with Eluate eg. Eluate-Fyb. Click PERFORM or VERIFY to save the results. Submit panel sheet(s) to the senior technologist for review.
PROCEDURE NOTES
1.
Prolonged immersion of red cells in the elution solution causes hemolysis. The consequent release of hemoglobin into the eluate alters the pH and may affect the performance of the eluate in serological testing.
Do not add potentiators such as bovine albumin or a low ionic strength additive solution, as the eluate is already a low ionic substrate. Polyethylene glycol (PEG) may be used to increase to sensitivity of the eluate as it will not affect the ionic strength. For greater test sensitivity if the direct antiglobulin test on the original red cell was weak (w to 1+), the sensitivity of the antibody detection test may be enhanced by increasing the number of drops of eluate per test and/or by extending the incubation time (e.g. 3-4 drops of eluate may be used for the test instead of 2 drops, and/or incubation at 37 C may be extended to 20 minutes). Not washing the panel cells with saline before adding anti-human globulin improves the sensitivity of the test by minimizing dissociation of antibody bound to the test cells during incubation.
2.
3.
4.
LIMITATIONS OF PROCEDURE
The yield of antibody obtained upon elution from coated red blood cells is dependent on the following variable factors:
1. The amount of antibody bound to the cells. Where elution is being attempted from red blood cells which have been incubated with serum in vitro, this is related to the serum: cell ratio in the incubating mixture, to the mean binding constant of the particular antibody, to the number, type and accessibility of the red cell receptor sites and whether or not the reaction has been allowed to reach equilibrium. These factors are partially under the control of the serologist, who is able to vary proportions of serum to cells and incubation conditions accordingly. The degree of dissociation of antibody that occurs during the washing in cold 4 C working wash solution. More dissociation of antibody will occur if the working wash solution is warm, giving false negative results. The degree of recombination of antibody that occurs before the eluate is separated from the cells. This is minimal with the acid elution procedure, as separation of the eluate from the cells occurs at pH that is unfavorable for antibody association. The degree to which immunoglobulin is denatured by the low pH during dissociation. This is minimal if the procedure is carried out as recommended.
2.
3.
4.
Page 61 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
5.
Other factors to be considered are: 5.1. Red blood cells which have a positive direct antiglobulin test due to bound complement alone will normally yield an eluate showing no antibody activity. Incorrect restoration of pH in the eluate may cause hemolysis of red blood cells in subsequent testing. Cells from blood samples stored for longer than 72 hours may yield less potent eluates than those from freshly drawn samples. An alternative elution procedure may be preferable for the preparation of eluates from stored cells. A false negative test may occur if the test red cells suspension is not washed sufficiently free of human protein before incubation with eluate, or if the test system becomes contaminated in any way with human protein other than antibody dissociated during the elution phase. A negative Coombs control test indicates this source of error.
5.2.
5.3.
5.4.
REFERENCES 1. 2. Elukit, Package Insert. Houston, TX: Gamma Biologicals, August 1995. Technical Manual, 13th edition. Bethesda, MD: American Association of Blood Banks, 1999.
3.
Cerner HNA Millenium Integrated Clinical Information System PathNet User Training Manual, 1st Edition, King Faisal Specialist Hospital and Research Center, July 2002.
Page 62 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
BLOOD BANK INTERNAL PROCEDURE / POLICY
TITLE/DESCRIPTION: INDEX NUMBER(S):
ELUTION - LUI FREEZE
EFFECTIVE DATE: REVISION DATE/NUMBER: DISSEMINATION:
748
FEB92
REV9 / AUG02
XM
PRINCIPLE Elution is the removal of antibody that has been adsorbed onto the surfaces of red cells. If an ABO antibody is suspected, as commonly occurs in neonates whose blood type is ABO incompatible with maternal blood, the method of choice is Lui freeze elution. After the eluate is prepared, it should be tested with A and B cells, as well as with a 3-cell panel of O red cells of known antigenic make up (antibody screening cells).
POLICY A Lui freeze eluate will be prepared from cord samples of suspected ABO hemolytic disease of the newborn cases. The eluate will be tested against A1, B and O cells using antiglobulin technique. SPECIMEN Antibody coated red cells from group A, B or A,B cord blood sample which has tested DAT positive.
REAGENTS, SUPPLIES AND EQUIPMENT Saline Stoppered Test Tube -20C to -70C Freezer Running Tap Water Centrifuge (Calibrated) Page 63 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Reverse grouping cells Antibody screening cells Cellwasher IgG Sensitized Cells Anti-human globulin reagent 12 x 75 mm test tubes Marking pen Disposable pipettes 37C Dri Bath
SAFETY PRECAUTIONS All blood and blood products must be treated as potentially infectious. Follow safety precautions detailed in the Laboratory Safety Manual.
QUALITY CONTROL The purpose of this control test is to assure that antibody present in the eluate has been derived from the bound state on the original cells, and is not unbound antibody remaining as the result of inadequate washing. 1. Retain a sample of saline from the last wash of the coated red cells to test for antibody activity against A and B cells. If antibody activity is present in the last wash, repeat the elution procedure after more thorough washing of the cells.
2.
PROCEDURE 1. Wash cells to be eluted with large volumes of saline at least 6 times. Mix well after each addition of saline and centrifuge for one minute. Remove supernatant carefully without losing any red cells. Retain the last wash. Test as specified in Quality Control (above). Add 3 drops of 0.9% saline to 10 drops of the well washed packed red blood cells. Stopper the tube and mix well. Coat the sides of the tube with red cells by rotating the tube. Rapidly freeze the red cell layer by placing the tube horizontally in a -20C to -70C freezer for 10 minutes. Thaw rapidly under warm running tap water. Centrifuge the hemolysed cells at high speed for 2 minutes. appropriately labeled test tube. Remove the hemolysate to an
2. 3. 4. 5. 6.
7. 8.
9.
Test the hemolysate (2 drops) against A and B cells (1 drop) and screening cells I, II and III (1 drop) by antiglobulin technique. Test last wash against A and B cells. 9.1. 9.2. Do not add LISS. Incubate for 15 minutes at 37C. Page 64 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
9.3. 9.4. 9.5.
Wash 4 times in the cell washer. Add 2 drops of AHG. Centrifuge and read. To all negative tubes, add 1 drop IgG sensitized cells. Centrifuge and read. Record results.
REPORTING RESULTS 1. 2. 3. Record serological results on panel sheets. Order Eluate ,Lui under the DEPARTMENT ORDER ENTRY application. Enter results in the BLOOD BANK RESULT ENTRY application.
3.2 Agglutination of A cells with a negative antibody screen demonstrates presence of anti-A.
3.3 3.4 Agglutination of B cells with a negative antibody screen demonstrates presence of anti-B. Agglutination of A and B cells with a negative antibody screen demonstrates presence of anti-A,B.
5.
If agglutination is present in the screening cells, perform the Elukit elution. See IPP 704 - Elution - Acid (Elukit). Append comment under mothers medical record number, e.g., Cord # (baby MRN) B POS, DAT POS; ANTI-B ELUTED, date and accession #, using the appropriate comment template. Print a hard copy of LUI Eluate results and attach to panel sheets. Submit to senior technologist for review.
6.
7.
PROCEDURE NOTES 1. This elution is only used for confirming ABO HDN. Do not utilize to identify other antibodies. If positive DAT is suspected to be other than ABO, utilize Elukit elution. See IPP 704.
LIMITATIONS OF PROCEDURE 1. 2. This is a poor elution technique for antibodies other than ABO. The markedly hemoglobin stained eluate causes difficulty in reading tests prior to antiglobulin stage.
REFERENCES 1. Basic Blood Grouping Techniques and Procedures, 2nd Edition. Victorian Immuno-haematology Discussion Group. 1992. Technical Manual, 13th edition. Bethesda, MD: American Association of Blood Banks, 1999.
2.
Page 65 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
BLOOD BANK INTERNAL PROCEDURE / POLICY
TITLE / DESCRIPTION: INDEX NUMBER(S):
EMERGENCY TRANSFUSION
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
730
FEB92
REV8 / SEP02
XM
PRINCIPLE Emergency issue of blood for transfusion, i.e. issue of blood prior to completion of pretransfusion testing, must be requested by the patient's physician. That physician must take responsibility for the transfusion of uncrossmatched blood and its attendant risks.
POLICY When a delay in transfusion could be detrimental to the patient, blood products will be released prior to completion of pre-transfusion testing in accordance with AABB Standard 5.17.4 Urgent Requirement for Blood. These products will be prepared and dispensed in accordance with AABB Standards 5.11 to 5.17
REAGENTS, SUPPLIES, EQUIPMENT Emergency Transfusion Form (Appendix I) "NOT CROSSMATCHED" unit tags (Appendix II)
Page 66 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
SAFETY PRECAUTIONS Follow safety precautions listed in referenced IPPs.
PROCEDURE Candidates for emergency dispense of blood for transfusion fall into two categories depending on the availability of a specimen for pre-transfusion testing, but in both scenarios, the units will be dispensed in the same manner: 1. Patients with no type and screen in the past 72 hours - specimen accompanies request for emergency transfusion. 1.1 1.2 Locate previous patient records, if available, either in computer or card file. Perform ABO/Rh on the blood specimen according to ABO/Rh and Weak D Typing IPP 701. 1.2.1 If blood group matches previous records, select type specific units from available blood inventory. If blood group does not match previous records, select O negative units and request that a repeat specimen be drawn for pre-transfusion testing and patient's ID be rechecked. Proceed with procedure step 2 as if no specimen were available.
1.2.2
1.3
Save segments in labeled tubes from each unit to be issued. If time allows, perform immediate spin crossmatches on units to be emergency issued. Attach "NOT CROSSMATCHED" tags (Appendix II) to units to be issued. Go to the DISPENSE AND ASSIGN application. Select the DISPENSE mode under TASK. Enter the patients medical record number. Barcode the unit into the Worksheet. If the unit group does not match the patients group, an exception box will open. Ensure the unit group is compatible with the recipients group, then select YES to override.
1.4 1.5 1.6 1.7 1.8 1.9
1.10 Select EMERGENCY as the reason. 1.11 Click the Save icon. A Save box will open. 1.12 Enter the ordering physicians name in the Physician box. 1.13 Select EMERGENCY in the Reason box. 1.14 List OK in the Visual Inspection box.
Page 67 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
1.15 Enter the messengers ID number in the courier box. 1.16 Enter the ward in the Location box. 1.17 Press OK at the bottom of the box. 1.18 The print box will open. Select the appropriate printer to print the Emergency Transfusion Form (Appendix I). 1.19 Attach the Emergency Transfusion Form (Appendix I) to the unit. 1.20 Go the GENERATE TAGS AND LABELS application. 1.21 Click on Option Reprint. 1.22 Click on Emergency Tag under Tag/Label box. 1.23 Select 2 copies. 1.24 Enter the patients MRN number and the product number in the appropriate fields. 1.25 Click the printer icon. 1.26 Place one Emergency Transfusion Request form (Appendix I) with the unit and give to the messenger. Note: Ideally a signed request form should accompany the specimen but the form can be sent with blood products and be signed and returned to the Blood Bank at a later time. 1.27 Place the other on the Seniors desk for follow up. 1.28 Complete the type and screen according to ABO/Rh and Weak D Typing IPP 701 and Antibody Screen IPP 706. Perform the crossmatch according to Crossmatch IPP 722. 1.28.1 If the antibody screen is negative, perform immediate spin crossmatches using segments saved from units already issued. 1.28.2 Before entering the crossmatch results in the computer, the unit has to be given a transfused status. 1.28.3 Go to the FINAL DISPOSITION application. 1.28.4 Select the Transfuse mode under Task. 1.28.5 Enter the product number and click on the SAVE icon. 1.28.6 A crossmatch may have to be ordered under Accession Add On in the DEPARTMENT ORDER ENTRY
Page 68 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
application, if not entered by the floor with the Type and Screen. 1.28.7 Go to the RESULT ENTRY application to enter the crossmatch results under the accession number. 1.28.8 A message box will appear stating that the unit is not in a valid state for crossmatch because it has bee dispensed and transfused already. 1.28.9 Click on YES after the Do you wish to continue? question. 1.28.10 Enter the crossmatch results and interpretation and click on PERFORM or VERIFY. 1.28.11 A message box will appear stating that the product is transfused, the crossmatch procedure results will be saved, but product will not be set to crossmatched. Click OK.
1.28.12 Another message box will appear asking if you want to complete the crossmatch for that accession number. Click on YES and the crossmatch is completed. . 1.8.2 If antibody screen is positive, inform patients physician and the Blood Bank Supervisor immediately. Complete full AHG crossmatch to determine if units issued are compatible. Identify the antibody and antigen type the units according to Antibody Identification - Basic Panel IPP 707 and Antigen Typing IPP 710.
2.
Patient with no type and screen in past 72 hours - no specimen available. 2.1 2.2 2.3 Notify the requesting location that a sample for crossmatch must be collected Stat. Select O negative units from available blood inventory. Save segment in labeled tubes from each unit to be issued. Use segments for crossmatching when the specimen is received. If time allows, group check the units prior to issue. Attach "NOT CROSSMATCHED" tags (Appendix II) to units to be issued. Dispense the units according to steps 1.5 1.27. Note: Ideally a signed request form should accompany the specimen but the form can be sent with blood products and be signed and returned to the Blood Bank at a later time. 2.6 2.7 When specimen is drawn and received, perform the type and screen. If antibody screen is negative, perform immediate spin crossmatches using segments saved from units already issued.
Page 69 of 95
2.4 2.5
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
2.8
Before entering the crossmatch results in the computer, the unit has to be given a transfused status. 2.8.1 2.8.2 2.8.3 2.8.4 Go to the FINAL DISPOSITION application. Select the Transfuse mode under Task. Enter the product number and click on the SAVE icon. A crossmatch may have to be ordered under Accession Add On in the DEPARTMENT ORDER ENTRY application, if not entered by the floor with the Type and Screen. Go to the RESULT ENTRY application to enter the crossmatch results under the accession number. A message box will appear stating that the unit is not in a valid state for crossmatch because it has bee dispensed and transfused already. Click on YES after the Do you wish to continue? question. Enter the crossmatch results and interpretation and click on PERFORM or VERIFY. A message box will appear stating that the product is transfused, the crossmatch procedure results will be saved, but product will not be set to crossmatched. Click OK.
2.8.5
2.8.6
2.8.7
2.8.8
2.8.9
2.8.10 Another message box will appear asking if you want to complete the crossmatch for that accession number. Click on YES and the crossmatch is completed. 2.8.2 If antibody screen is positive, inform patients physician and the Blood Bank Supervisor immediately. Complete full AHG crossmatch, antibody identification and antigen typing to determine if units issued are compatible.
REPORTING RESULTS 1. Complete the ABO/Rh, antibody screen and crossmatch STAT and record in the computer. If incompatible crossmatches are found, notify the physician to stop transfusion immediately and have all issued blood returned to Blood Bank. Notify the Blood Bank Medical Director immediately. A copy of the Emergency Transfusion Form must be returned to the Laboratory within 24 hours, complete with the signature of the charge nurse and attending physician. The
Page 70 of 95
2.
3.
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
original should go into the patients chart. Give form to senior for review. Senior will file forms in the Emergency Transfusion file in the issue bench area.
PROCEDURE NOTES 1. Should any patient with a request for emergency transfusion prove to have a previously identified clinically significant antibody, units negative for that antigen(s) must be given and blood should not be issued by emergency issue. Units should be typed STAT for the antigens in question and a specimen can be obtained in the meantime. Contact the on-call blood bank pathologist if this is not acceptable with the requesting physician. Each unit dispensed should have a NOT CROSSMATCHED tag attached to it with a tach-it. An Emergency Transfusion Form is unique for each unit dispensed. There should be one attached to the unit itself and one that accompanies the unit. A sample for crossmatch must be collected at the earliest opportunity in the transfusion sequence.
2.
3.
3.
LIMITATIONS OF PROCEDURE If the patient has alloantibody and compatible units are not available, refer to the Medical Director of Blood Bank. The decision may be made to issue incompatible units.
REFERENCES 1. Technical Manual, 13 Edition, Bethesda, MD: American Association of Blood Banks, 1999. Standards for Blood Banks and Transfusion Services, 21st Edition. American Association of Blood Banks, 2002. Bethesda, MD:
th
2.
Page 71 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
BLOOD BANK INTERNAL PROCEDURE / POLICY
TITLE / DESCRIPTION: INDEX NUMBER(S):
TRANSFUSION REACTION INVESTIGATIONS
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
778
DEC91
REV7 / AUG02
XM
PRINCIPLE Any transfused blood product can cause an adverse effect which may be due to incompatibility of donor red cells and recipient plasma, bacterial contamination of blood product, transfusiontransmitted infection, allergy, white cell antibodies or other miscellaneous causes. The most common signs and symptoms of an adverse reaction due to transfusion of blood or blood products are: fever (increase of equal to or greater than 1 C or 2 F), with or without chills chills (rigors), with or without fever skin symptoms - hives (urticaria) or itching
Page 72 of 95
o o
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
chest pain and/or dyspnea acute hypotension or acute hypertension nausea, vomiting flushing bleeding hematuria hemoglobinuria anaphylaxis
POLICY Inaccordance with AABB Standards 7.3 The blood bank or transfusion service shall have a process for the detection, reporting, and evaluation of suspected complications of transfusion. An adverse event experienced by a patient in association with a transfusion shall be regarded as a suspected transfusion complication, and followed up accordingly.
SPECIMEN 10mL (min. 7mL) red top tube 5mL (min. 3mL) lavender top tube Bag from transfused product (if available)
REAGENT, SUPPLIES, EQUIPMENT Anti-A Anti-B Anti-D Anti-human globulin Coombs control cells 12 x 75 mL disposable tubes Automatic cell washer or Serofuge Disposable pipettes Transfusion Reaction Form (Appendix I) Transfusion Reaction Worksheet (Appendix II) used only during ICIS downtime 0.9% Saline
SAFETY PRECAUTIONS 1. All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual. Do not attempt to pick up broken glass with fingers. Use a dustpan or other scooping implement and dispose of glass fragments in sharps disposal container.
2.
PROCEDURE
Page 73 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Nursing Procedure (Read this section to nurses if they dont know what to do) 1. 2. 3. Stop the infusion immediately; keep the line open with a slow infusion of saline. Notify the physician immediately. Notify the Blood Bank (extension 38270, 38220, 35841, or 35842) immediately. Notify the Blood Bank of the unit number(s) of the blood products implicated in the reaction. Reconfirm the identification of the patient and the identification of the blood infused. Complete a Transfusion Reaction Form with the required information. One copy of the form must accompany the samples to the Blood Bank because there is no mechanism to note the clinical information in the ICIS. Retain a copy of the Transfusion Reaction Form in the patients chart. Order a Transfusion Reaction Careset in the computer which includes a DAT for Blood Bank, Urinalysis for Microbiology. Labels will print for the specimens. (One lavender and one Red top) labels will also print for a Urinalysis. Ensure samples are drawn STAT for the workup. Samples must be drawn carefully to minimize mechanical hemolysis and must be properly labeled. Send blood samples, Crossmatch / Component Transfusion Form, the Transfusion Reaction Form and the blood bag with infusion set and tag attached to the Blood Bank, STAT. Send a properly labeled urine sample (when available) to Microbiology for urinalysis. Do not transfuse the patient until the reaction investigation is completed. If transfusion is indicated prior to completion of the investigation, the physician must consult with the Blood Bank Director.
4. 5.
6. 7.
6.
7.
8.
9. 10.
Blood Bank Procedure NOTE: If a severe reaction such as hemolytic, anaphylactic, bacterial contamination or any other reaction that may be life threatening is suspected at any stage in the investigation, immediately notify the Blood Bank Medical Director or Consultant and the Supervisor. Red Cell Products Immediate Workup: 11. Transfusion reaction investigations are STAT procedures and must be completed as soon as possible. If possible, a different technologist other than the one who crossmatched the blood must perform the investigation. Login the samples when they are received.
12.
Page 74 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
13.
Check that all the required clinical information is completed on the Transfusion Reaction Form. Enter transfusion reaction work up results under RESULT ENTRY. Perform clerical check: 15.1 Check the patient's name, medical record number, blood type, donor unit number and donor blood type on all patient specimens, components involved, paper and computer records. 15.2 Record findings in the computer in the Clerical Check cell, either clerical check OK, or clerical error noted. 15.3 If any discrepancy is noted in clerical check, proceed as follows: 15.3.1 If there is evidence of a transfusion error, notify the Blood Bank consultant, patient's physician and supervisor immediately. 15.3.2 If there is indication of a mix-up of patient samples, misdraw of patient, or mix-up of donor units, check other patient records over the same time period as there may be another patient at risk.
14. 15.
16.
Perform visual inspection of sample: 16.1 Compare pre and post transfusion specimens. Check for hemolysis and jaundice (yellow or brownish coloring). Record findings in the computer in the PRE and POST Hemolysis and PRE and POST Icteric cells, either YES or NO. 16.2 If hemolysis or jaundice is observed in post transfusion sample but not in the pretransfusion sample, refer to Extended Workup below.
17.
Perform direct antiglobulin test (DAT): 17.1 Perform a DAT on post transfusion specimen. Record results at the DAT cells. 17.2 If the DAT is positive on the post transfusion sample, Add on a DAT to the pretransfusion TS. If a DAT was already performed on the pre-transfusion sample enter the repeated result as a comment. 17.2.1. If the DAT on the pre transfusion sample is the same strength as the post reaction sample, this indicates the DAT is not caused by the transfusion. 17.2.1.1. If this is the first time that a DAT was performed on the pre transfusion sample, perform an eluate on the pre-transfusion (or post-transfusion) sample. 17.2.2. If the DAT on the pre transfusion sample is negative, or is weaker than the post reaction sample, refer to Extended Workup.
18.
Check for temperature increase:
Page 75 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
18.1 If there has been a rise in temperature of at least 1C enter a result of Y in the TEMPERATURE INC cell otherwise enter N. 18.2 Send blood bag for culture if the temperature increase is 1C or greater. 18.3 Register the unit so tests can be ordered. Go to the DEPARTMENT ORDER ENTRY application. Click in the medical record number box and press ENTER. An Encounter Search box will appear, click on ADD PERSON. Select KFSHRC Riyadh as the Client and Facility name and the Registration window will open. In the FIRST NAME box, enter Crossmatch. In the MIDDLE NAME box, enter Transfusion Reaction . In the LAST NAME box, enter the product number i.e GM12345. Enter the birth date as the order date for ease of tracking. Enter Dr. Roberts for the admitting and the attending physican. In the MEDICAL SERVICE box, select LAB- BLOOD BANK. In the BUILDING box, select MAIN BUILDING. In the AMBULATORY box, select LAB-MAIN-R. At the bottom of the box, select OK.. A new medical record number will be assigned. In the ORDERABLE box, select Blood Culture and the collection detail box will open. Ensure the print label box is checked off and that the information is correct and click ADD under ORDERS. Enter Blood Bank PRBC under the Body Site. Enter none under Antibiotics. Click on the SUBMIT ORDERS icon and note the accession numbers that are assigned. Retrieve labels from the designated printer and affix to the unit. The culture specimen must be submitted to Microbiology as soon as possible. A delay in receipt of the specimen can disrupt Microbiologys blood culture numbering sequence and cause possible further delays.
18.4 18.5 18.6 18.7 18.8 18.9 18.10 18.11 18.12 18.13 18.14 18.15 18.16 18.17 18.18
18.19 18.20 18.21 18.22 18.23
Page 76 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
18.24 19.
Enter either YES or NO under Bag Sent for Culture.
If there is no immediate indication of an acute hemolytic transfusion reaction, enter a result of N at the HEMOLYTIC cell. After completing result entry, click Perform / Verfy. Go to the ORDER RESULT VIEWER application and print the Transfusion Workup Results. Look up and record blood culture and urinalysis accession numbers on the print out, if applicable. Give Report to Senior for review who will then forward it to the Blood Bank consultant for evaluation and interpretation. Save the blood product bag(s) in Jewett refrigerator for one week. If the bag is sent to Microbiology, they will retain it for one week.
20. 21.
22.
21.
Extended Workup: NOTE: If Clerical Check, Visual Inspection or DAT give positive results, further workup must be done immediately to confirm or rule out an acute hemolytic transfusion reaction. 22. Add on a TS and Crossmatch to the transfusion reaction accession number. Perform ABO and Rh testing on the patients post-transfusion sample and enter the results in Cerner. Perform an antibody screen with the post-transfusion sample and enter the results in Cerner. If a previously undetected antibody is detected, perform antibody identification to identify the antibody. Test the segment from the transfused donor unit for the corresponding antigen. Order and enter the antigen types on the unit according to IPP710 Antigen Typing. Perform a crossmatch with the post- transfusion sample using an attached segment or on blood remaining in the blood bag. Perform full AHG crossmatch even if the pretransfusion crossmatch was only immediate spin. Perform ABO and Rh testing on the patients pretransfusion sample and on blood from the unit or an attached segment. 25.1 Enter the specimen number of the pre-transfusion TS or enter the product number and the number of the unit that is being retyped. 25.2 Enter repeat results performed on the pre-transfusion sample or unit segment in the form of a result comment after the initial verified results. For example: 4+ Pretransfusion sample repeat. or Unit retype repeat. 26. Perform an antibody screen on the pre-transfusion sample. Enter results as outlined above. If a previously undetected antibody is detected, perform antibody identification to identify the antibody. Test the segment from the transfused donor unit for the corresponding antigen. Order and enter the antigen types on the unit according to IPP710 Antigen Typing.
23.
24.
25.
Page 77 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
27.
Perform a crossmatch with the pre-transfusion sample using an attached segment or on blood remaining in the blood bag. Enter the results in Cerner as outlined above. Perform a full AHG crossmatch even if the pretransfusion crossmatch was only immediate spin. If DAT is positive, add on an eluate. Perform an eluate on the post transfusion sample. Consult with the Blood Bank Medical Director or consultant to determine whether further testing is needed, such as baseline and 6 hours post transfusion levels of: Haptoglobin Plasma hemoglobin Total Bilirubin Serum creatinine Urea Refer to Technical Manual for additional serological techniques which may be useful.
28. 29.
30.
Delayed Hemolytic Transfusion Reaction Workup: 31. Suspected Delayed Hemolytic Transfusion: 31.1 If DHTR is suspected by floor, request them to order a Transfusion Reaction and send it to Crossmatch. Perform a Transfusion Reaction investigation as outlined above in Immediate Workup. 31.2 If DHTR is suspected in Crossmatch due to a positive DAT with antibody eluted, order a Transfusion Reaction or, if appropriate, add on a Transfusion Reaction to the existing TS requisition. Enter a comment Transfusion reaction on unit xxxxx. 31.3 Result the transfusion reaction as outlined above in Immediate Workup. 32. In the RESULT ENTRY application, enter the results of ABO/Rh, Antibody Screen, DAT and ELUATE. Attach panel and elution results. In computer, print out: 33.1 Patients transfusion history in the PATIENT PRODUCT INQUIRY application. 33.2 Patients laboratory tests in the ORDER RESULT VIEWER CBCs since last transfusion (to track Hct) Bilirubins pretransfusion and since last transfusion 34. Attach all results printouts. Look up and record blood culture accession number on Transfusion Reaction results, if applicable. Give to Senior for review who will then forward it to the Blood Bank consultant for evaluation and interpretation. The Blood Bank consultants will enter interpretions in the ICIS.
33.
35.
Non-Red Cell Products Acute Hemolytic Transfusion Reactions are not likely to occur with non-red cell products. Therefore a limited workup is adequate (as follows):
Page 78 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
36. 37.
Login the samples when they are received. Check that all the required clinical information is completed on the Transfusion Reaction Form. Enter transfusion reaction work up results under RESULT ENTRY. Perform clerical check: 39.1 Check the patient's name, medical record number, blood type, donor unit number and donor blood type on all patient specimens, components involved and paper and computer records. 39.2 Record findings in the computer in the Clerical Check cell, either clerical check OK, or clerical error noted.
38. 39.
40.
If any discrepancy is noted in clerical check, proceed as follows: 40.1 If there is evidence of a transfusion error, notify the Blood Bank consultant, patient's physician and supervisor immediately. 40.2 If there is indication of a mix-up of patient samples, misdraw of patient, or mix-up of donor units, check other patients records over the same time period as there may be another patient at risk.
41.
Check patient MR comments for previous transfusion reactions and record the date and classification of each on the Transfusion Reaction Form Perform visual inspection of sample: 42.1 Compare pre and post transfusion specimens. Check for hemolysis and jaundice (yellow or brownish coloring). Record findings in the computer in the PRE and POST Hemolysis and PRE and POST Icteric cells, either YES or NO. 42.2 If hemolysis or jaundice is observed in post transfusion sample but not in the pretransfusion sample, refer to Extended Workup.
42.
43.
Check for temperature increase: 43.1 A rise in temperature of at least 1C enter a result of Y in the TEMPERATURE INC cell otherwise enter N. Send component bag for culture if the temperature increase is 1C or greater. Register the unit so tests can be ordered. Go to the DEPARTMENT ORDER ENTRY application. Click in the medical record number box and press ENTER. An Encounter Search box will appear, click on ADD PERSON.
Page 79 of 95
43.2
43.3
43.4 43.5
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
43.6
Select KFSHRC Riyadh as the Client and Facility name and the Registration window will open. In the FIRST NAME box, enter Crossmatch. In the MIDDLE NAME box, enter Transfusion Reaction . In the LAST NAME box, enter the product number i.e GM12345. Enter the birth date as the order date for ease of tracking. Enter Dr. Roberts for the admitting and the attending physican. In the MEDICAL SERVICE box, select LAB- BLOOD BANK. In the BUILDING box, select MAIN BUILDING. In the AMBULATORY box, select LAB-MAIN-R. At the bottom of the box, select OK. A new medical record number will be assigned. In the ORDERABLE box, select Blood Culture and the collection detail box will open. Ensure the print label box is checked off and that the information is correct and click ADD under ORDERS. Enter Blood Bank Platelets, FPP, or Cryo under the Body Site. Enter none under Antibiotics. Click on the SUBMIT ORDERS icon and note the accession numbers that are assigned. Retrieve labels from the designated printer and affix to the unit. The culture specimen must be submitted to Microbiology as soon as possible. A delay in receipt of the specimen can disrupt Microbiologys blood culture numbering sequence and cause possible further delays. Enter either YES or NO under Bag Sent for Culture.
43.7 43.8 43.9 43.10 43.11 43.12 43.13 43.14 43.15 43.16 43.17
43.18
43.19 43.20 43.21
43.22 43.23
43.24 44.
If there is no immediate indication of an acute hemolytic transfusion reaction, enter a result of N at the HEMOLYTIC cell Enter NP at the DAT result prompts. After completing result entry, click Perform / Verfy.
45. 46.
Page 80 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
47.
Go to the ORDER RESULT VIEWER application and print the Transfusion Workup Results. Look up and record blood culture and urinalysis accession numbers on the print out, if applicable. Give Report to Senior for review who will then forward it to the Blood Bank consultant for evaluation and interpretation. Save the blood product bag(s) in Jewett refrigerator for one week. If the bag is sent to Microbiology, they will retain it for one week.
48.
49.
REPORTING RESULTS 1. If Microbiology reports a positive blood culture, notify the Blood Bank Director or Consultant immediately. If bacterial contamination is suspected, the pathologist will notify the patients physician immediately. If any results are indicative of an acute hemolytic transfusion reaction, notify the Blood Bank Director or Consultant and the Supervisor immediately. If an acute hemolytic reaction is suspected, the pathologist will notify the patients physician immediately. If there is indication there may be further workup needed to rule out a reaction, leave the HEMOLYTIC cell result pending, to be resulted when the workup is completed. Attach the Transfusion Reactin Form received from the Ward to the completed transfusion reaction result print out and submit to the Senior Technologist for review and forwarding to the Blood Bank Director or Consultant. The pathologist will review these results as soon as possible for interpretation and may recommend further testing. The Blood Bank Director or consultant will return the completed report to the Crossmatch Senior Technologist. The Senior Technologist will enter the relevant information into the patients Medical Record Data for future reference and then file the Transfusion Reaction Forms in the Transfusion Reaction binder. If there is any real or potential adverse reaction caused by blood or components received from another facility (King Fahad National Guard Hospital or Aramco Hospital in Dhahran), the Blood Bank Supervisor will notify the facility. Complete a Variance Report with the details of the problem and document date, time, and contact person at the other facility who received the information.
2.
4.
5.
6.
7.
PROCEDURE NOTES 1. Delayed hemolytic transfusion reactions may not be apparent for several days following transfusion. The most common signs are fever, unexpected fall or less than expected rise in hemoglobin, and jaundice. The DAT may be positive. Patients who experience repeated febrile reactions which are possibly due to white blood cell antibodies may be transfused with blood that is leukocyte reduced by filtration. Approval by the Medical Director is required before placing a patient on this protocol permanently.
2.
Page 81 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3.
All reactions should be handled initially as possible hemolytic reactions. The most dangerous reactions which can occur are acute hemolytic, septic shock, and anaphylactic shock. Most acute hemolytic transfusion reaction occur as a result of misidentification or clerical errors in the procedures for blood drawing, requesting blood, pretransfusion testing, issuing of blood and administration of blood. Therefore, procedures must be adhered to strictly. Most acute hemolytic transfusion reactions, transfusion of bacterial contaminated blood products and anaphylactic reactions will be apparent after the first few mL. of blood has been infused. Therefore, the infusion should be started slowly and the patient observed closely for symptoms during the first 15 minutes of infusion. If there is any report or mention of possible disease transmission in response to transfusion, record the patients name, medical record number, physician name, then report this information to the Medical Director who will decide if there is indication for followup. In the event of a computer downtime, the transfusion reaction work up may be ordered on the Blood Bank Downtime Orders Form that will be accompanied with the Transfusion Reaction Form. The workup and investigation will be documented on the Transfusion Reaction Worksheet. The urinalysis and blood culture will have to be ordered on a separate form, Laboratory Miscellaneous Orders Form.
4.
5.
6.
REFERENCES 1. Technical Manual, 13 Edition, Bethesda, MD: American Association of Blood Banks, 1999, Pages 543-562. Standards for Blood Banks and Transfusion Services, 21st Edition. American Association of Blood Banks, 2002. Bethesda, MD:
th
2.
TRANSFUSION REACTION WORKSHEET COMPUTER DOWNTIME
MRN_________________________ Name__________________________ Accession Number________/______/____ Unit Number________________________
Donor
CLERICAL CHECK Re-check of identity of patient, Donor unit(s) records and find no discrepancy OK Tech: Recipient OK Yes / No Yes / No
Tech:
Page 82 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
VISUAL INSPECTION OF PATIENTS SERUM Haemolysis Pre Transfusion Yes Sample number ____/_____/_____ Post Transfusion Yes Sample number ____/_____/_____ Bag sent for culture Yes / No Results of culture Blood in first voided urine Yes / No / No Yes / No AHG. CC INTERP. / No Yes / No Icteric
Direct Antiglobulin Test
AHG CC INTERP.
Accession number if yes ___/___/____ CONFIRMATION OF ABO AND RH TYPE Serum A Pre Transfusion Recipient Donor Donor Segment DAT AHG Post Transfusion Segment CC INTERP. Cells B D CON A B INTERP.
RECONFIRMATION OF CROSSMATCH Recipient Serum Pre Transfusion Post Transfusion Donor RBC Segment Donor RBC Segment IS 37 C AHG CC Compatible
Technologist : Conclusions: Pathologist:
Date:
Date:
Entered in ICIS By:_______________ Date:___________ Reviewed By: ____________ Date: _______
King Faisal Specialist Hospital and Research Centre Pathology and Laboratory Medicine - Blood Bank Riyadh, Saudi Arabia
TRANSFUSION REACTION FORM
Page 83 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Ordering Doctor________________ Pager Number ________________ Date Requested ____/____/____ Patient Location_____________ Type of Product: Time Requested ______________ Ward Phone Ext. _____________ Unit Number(s):
Time and Date Transfusion Began:
Time and Date Transfusion Stopped:
Time apparent reaction began:
Amount remaining in bag ML
Symptoms
Time and Date reported to Blood Bank:
Clerical check performed by 2 SN Is or one SN I and one SN II OK Y / N
Meds Given for adverse reaction:
ID ___________/____________
PLEASE NOTIFY BLOOD BANK IMMEDIATELY IF CLERICAL CHECK DOES NOT MATCH
Before transfusion Temperature Pulse Blood Pressure Staff Nurse Signature ______________________________________________________
Refer to Nursing Policy Blood Transfusion : Adverse Reactions Send yellow copy with blood bag, tubing, samples and all transfusion documentation AFTER completing Transfusion Reaction order in the computer. During ICIS downtime send this form with Blood Bank Orders Form. Retain white copy in patients chart. If blueplate not available then the following information is required: MRN, Full Name, DOB, Sex__________________
At time of suspected transfusion reaction
BLOOD BANK INTERNAL PROCEDURE / POLICY
TITLE / DESCRIPTION: INDEX NUMBER(S):
W.A.R.M. (Warm Autoantibody Removal Medium)
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
781
OCT93
REV4 / SEP99
(Reviewed MAR02)
XM
Page 84 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
PRINCIPLE The red cells from a patient with a positive DAT and free serum autoantibody are treated with W.A.R.M. This treatment removes IgG autoantibody, thereby reducing the strength of the positive DAT and freeing antigen sites for adsorption. Concomitantly, the enzyme premodifies the red cells. The red cells, thus prepared, are combined with autologous serum and the mixture is incubated at 37oC. The warm-reactive autoantibody is attached to the antigen present on the patient's red cells. This antigen-antibody interaction is enhanced by the enzyme treatment of the cells. Following incubation, the mixture is centrifuged and the adsorbed serum is harvested and tested. By comparing the results of W.A.R.M.-adsorbed serum with those obtained with the unadsorbed serum, it is usually possible to confirm the presence of the warm-reactive autoantibody, and detect or identify any additional alloantibody(ies) that may be present.
POLICY W.A.R.M. procedure will be performed prior to any other autoadsorption technique to remove a warm reactive auto antibody from patient serum. Red cells from recently transfused patients (within past 3 months) should not be used for autoadsorption because transfused red cells in the circulation are likely to adsorb alloantibodies.
SPECIMEN 5mL (min. mL) whole blood in a Lavender Top tube. 10mL (min. 7mL) whole blood in a Red Top tube. REAGENTS, SUPPLIES AND EQUIPMENT
W.A.R.M.
(Reconstitute with deionized water prior to use; see label for volume and directions. Store reconstituted W.A.R.M. at 2-8oC for no more than 5 days after reconstitution. Do not freeze.) Isotonic saline Test tubes and test tube racks Transfer pipettes Serological centrifuge 37C dry bath or waterbath
SAFETY PRECAUTIONS 1. All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual. Do not attempt to pick up broken glass with fingers. Use a dustpan or other scooping implement and dispose of glass fragments in sharps disposal container.
2.
PROCEDURE 1. 2. 3. 4. Appropriately label a test tube. Add 1 ml of packed patient red cells that have been washed with 0.9% saline. Add 2 volumes of reconstituted W.A.R.M. to the tube (1 mL RBC: 2 mL W.A.R.M.). Mix well and incubate at 37C for 30 minutes. Page 85 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
5.
Wash the W.A.R.M.-treated cells with saline a minimum of three (3) times, being careful to remove as much supernatant as possible after each wash. Hard pack the W.A.R.M. treated red cells after the last saline wash. Add an equal volume of patient serum to the W.A.R.M.-treated, packed red cells. Mix well and incubate for 30-60 minutes at 37C. Centrifuge for two (2) minutes or until red cells are well-packed. Harvest the adsorbed serum (plasma) using a transfer pipette. Test an aliquot of the adsorbed specimen at 37C and the antiglobulin phase to determine if warm-reactive autoantibody has been removed. (See Interpretation). If results indicate that adsorption was insufficient, repeat steps 1-9 using a new aliquot of patient red cells. If adsorption is complete, the adsorbed specimen is ready for use in antibody detection and identification.
6. 7. 8. 9. 10.
Interpretation: 1. Complete Adsorption Complete adsorption of warm-reactive autoantibody has been achieved when the adsorbed serum no longer reacts where previously detected with: 1.1 1.2 The patient's own W.A.R.M. treated red cells; Those reagent red cells that lack antigens toward which additional alloantibodies are directed.
2.
Incomplete Adsorption If warm-reactive autoantibody has not been sufficiently removed, or the autoantibody cannot be adsorbed by W.A.R.M.-treated cells, agglutination will be detected when the serum is tested as in "1.1" or "1.2" above. NOTE: Complete adsorption of warm-reactive autoantibodies may not always be possible. However, in some instances, only partial adsorption of the autoantibody may be sufficient to reveal underlying alloantibody(ies) that might also be present.
REPORTING RESULTS Record reactions on panel sheet in parallel with unadsorbed serum results. Label columns clearly to designate which column is unadsorbed serum results and which is adsorbed serum results. Record the number of autoadsorptions performed.
LIMITATIONS OF THE PROCEDURE 1. Not all red cells will become DAT negative upon W.A.R.M. treatment. Some examples may only show a reduction in strength. It is possible that certain red cells will not be demonstrably affected. This does not obviate their use in an autoadsorption procedure. W.A.R.M. treatment and adsorption cannot be evaluated quantitatively. The number of adsorptions necessary as well as their effectiveness is dependent on a variety of factors and may differ from patient to patient.
2.
Page 86 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3.
Some autoantibodies have specificity within the Kell blood group system or other systems whose antigens are enzyme sensitive (Xga). Since W.A.R.M. treatment would destroy these antigens, autoadsorption using W.A.R.M.-treated cells would not be expected to be effective. The use of W.A.R.M.-treated red cells for antigen typing is not recommended since commercial antisera may or may not be specific when tested in this manner. On occasion, it is possible that a warm-reactive autoantibody will not be completely adsorbed by W.A.R.M.treated red cells. As a result, it may not be possible to assign a definitive specificity to those reactions obtained following adsorption. Further, complete adsorption of warm-reactive autoantibodies does not assure that those antibodies remaining in the adsorbed serum can be readily identified. Crossmatches performed on a warm autoadsorbed serum cannot be considered "compatible", since the antibodies removed by warm autoadsorption procedures are active at 37C. The warm autoadsorption procedure serves only as an aid in the detection and identification of underlying alloantibodies potentially masked by a warm-reactive autoantibody. Because the potential exists for adsorption of significant alloantibodies onto transfused donor red cells, autoadsorption procedures should not be performed on samples from recently transfused patients. Due to the fragility of certain red cells, some hemolysis may be observed upon treatment. The treatment of the red cells with W.A.R.M., should be no more than, but not less than thirty (30) minutes.
4.
5.
6.
7.
8. 9.
REFERENCE 1. Warm Autoantibody Removal Medium, Package Insert. Durham, NC: Organon Teknika, 1992.
BLOOD BANK INTERNAL PROCEDURE / POLICY
TITLE / DESCRIPTION: INDEX NUMBER(S):
ADSORPTION TECHNIQUE
EFFECTIVE DATE: REVISION NUMBER / DATE: DISSEMINATION:
703
Page 87 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
DEC91
REV4 / AUG97
(Reviewed MAR02)
XM
PRINCIPLE Antibody can be removed from the serum with red cells of the appropriate phenotype. The antibody forms a complex with the membrane-bound antigen; when the serum and cells are separated, the antibody remains attached to the cells. Adsorption techniques may be useful in the following situations: 1. 2. Removing autoantibody activity to permit detection of co-existing alloantibodies. Removing unwanted antibody from a serum that contains an antibody suitable for reagent use. Separating multiple antibodies present in serum or eluate to aid in antibody identification. Confirming the presence of an antigen on red cells through their ability to remove specific antibody from serum. Confirming antibody specificity.
3. 4.
5.
POLICY Autoadsorption for removal of autoantibodies should be used in untransfused patients whenever an autoantibody is present which may mask the presence of underlying clinically significant alloantibodies. Do not perform autoadsorption on a patient who has been transfused in the past three months, because transfused RBCs may adsorb alloantibody from the patients serum.
SPECIMEN 10mL (min. 7mL) red top tube 5mL Lavender top tube
REAGENTS, SUPPLIES, EQUIPMENT 0.9% saline 10mL test tube o ice or 37 C waterbath centrifuge
Page 88 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
SAFETY PRECAUTIONS All blood and blood products must be treated as potentially infectious. precautions detailed in the Laboratory Safety Manual. Follow safety
QUALITY CONTROL 1. Test the adsorbed serum against screening cells to determine if the procedure has removed the antibody. 1.1 Use the temperature and phase previously demonstrated to be optimal for antibody activity. A negative reaction indicates that adsorption is sufficient. A positive reaction indicates that further adsorption is necessary.
1.2 1.3
PROCEDURE 1. Wash the selected cells at least three times with saline. After the last wash centrifuge the cells for five minutes to pack them. Remove all the supernatant. Mix appropriate volumes of serum and cells, and incubate at the desired temperature for 30-60 minutes. 2.1 The serum to cell ratio used depends upon the strength of the antibody that is to be removed. The usual ratio is one volume of washed red cells to one volume of serum. The incubation temperature used should be that optimal for the activity of the antibody: 2.2.1 For cold reacting antibodies place the tube inside a plastic bag filled with crushed ice, seal, and mix on mechanical specimen rotator. For warm reacting antibodies place the tube in the 37 C waterbath and mix frequently.
o
2.
2.2
2.2.2
2.3
Use a large tube to increase area of contact between serum and cells, and mix tube every 5-10 minutes during incubation. Label
3.
Centrifuge and remove serum promptly to avoid antigen-antibody dissociation. serum as adsorbed serum.
4. 5.
Determine if all the antibody has been removed from the serum (see Quality Control). If eluate is to be performed, save cells.
LIMITATIONS OF PROCEDURE
Page 89 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Autoadsorption should not be performed on red cells from recently transfused patients because the circulating transfused red cells may adsorb the alloantibodies that are being sought.
PROCEDURE NOTES 1. In separating mixtures of antibodies, selecting the proper cells for adsorption is extremely important. The cells must be of an appropriate phenotype. The specificity of at least one of the antibodies must be known (or suspected) in order to choose cells positive for one antigen and negative for another. Pretreating red cells with a proteolytic enzyme may enhance antibody uptake, reducing the adsorptions required for complete removal of the antibody. Since some antigens are destroyed by proteases, antibodies directed against these antigens may not be removed by enzyme-treated cells. In the presence of warm reacting auto antibodies circulating autologous red cells are already coated with autoantibody which must be removed prior to performing an adsorption. Refer to W.A.R.M. (Warm Autoantibody Removal Medium) IPP781.
2.
3.
REFERENCES 1. Technical Manual, 13 Banks, 1999.
th
Edition, Bethesda, MD:
American Association of Blood
2.
W.A.R.M. Package Insert, West Chester, PA: BCA Division of Biopool International, 1999.
BLOOD BANK INTERNAL PROCEDURE / POLICY
TITLE/DESCRIPTION: INDEX NUMBER(S):
ANTIBODY TITRATION
EFFECTIVE DATE: REVISION DATE/NUMBER: DISSEMINATION:
709
JAN92
REV9 / AUG02
XM
Page 90 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
PRINCIPLE Titration is a semi-quantitative technique for measuring the amount of antibody. It is most frequently performed in the following situations: 1. Prenatal Studies - the mother's serum is tested at one-month or longer intervals during pregnancy; each clinically significant antibody is titered. ABO mismatched Bone Marrow Transplant may be requested prior to transplant and again approximately one year post transplant. Perform saline phase titration of anti-A and/or anti-B. Antibody identification - mixtures of antibodies may be identified by titration. DTT treatment can also be used to abolish IgM antibody activity to permit detection of coexisting IgG antibodies. DTT (Dithiothreitol, or Clelands reagent) treatment of the patients serum will split IgM antibodies, eliminating their agglutination ability, thus differentiating between IgG and IgM antibodies. Immunodeficiency workup - perform saline phase titration of anti-A and / or anti-B.
2.
3.
4.
POLICY Antibody titers will be performed when requested by the physician, when a new antibody is detected on a patient of the high risk OB/GYN physicians or at the discretion of the Blood Bank Director. Prenatal titers will not be performed once invasive monitoring has begun unless request is approved by Blood Bank Medical Director. Only clinically significant antibodies will be titered. Cells with homozygous expression of the corresponding antigen will be used for testing whenever practical. IgG titers using DTT are performed to aid in antibody identification.
SPECIMEN
10ml (min.7ml) clotted whole blood Frozen aliquot of previous serum sample containing the antibody to be titered. (stored in Revco Freezer #3)
REAGENTS, SUPPLIES, EQUIPMENT
12 mm x 75 mm test tubes Calibrated automatic pipette 100 L Disposable pipette tips Serological centrifuge and/or cell washer Saline 0.9% 6% Albumin Anti-human globulin Coombs Control cells Red blood cells appropriate for titration (see Procedure)
Page 91 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Antibody Titration worksheet (Appendix I) IgG Titration Using DTT worksheet (Appendix II)
For DTT titration only:
0.01M DTT in saline. Prepare in a chemical fume hood. 1. Place 0.077g DTT in flask (a Mettler scale is located in Flow Cytometry) and mix to a volume of 50 mL with isotonic saline. 2. Adjust pH to 8.0 by adding .5M NaOH (obtain in Chemistry). One-two small drops may be adequate. (pH meters are found in Immunology, Chemistry and Hematology) 3. Solution is stable for 3 months at 4C.
SAFETY PRECAUTIONS 1. All blood and blood products must be treated as potentially infectious. Follow universal precautions detailed in the Laboratory Safety Manual. Handle DTT and NaOH in a chemical fume hood, wearing gloves. DTT is harmful if inhaled and is irritating to eyes. NaOH causes eye and skin burns and causes digestive and respiratory tract burns.
2.
QUALITY CONTROL 1. The previous sample will be tested in parallel and the titer obtained from it will be compared to the previous reported titer prior to reporting results. The current sample is frozen for titrating in parallel with subsequent sample.
2.
PROCEDURE 1. Prenatal titration: 1.1 Locate previous sample, if available, in Revco #3. Record previous results on Antibody Titration Worksheet (Appendix I).
1.2 Perform ABO/Rh on current sample according to IPP701 ABO/Rh and Weak D Typing. 1.2.1 Perform an antibody screen (IPP706 Antibody Screen) if one hasnt been done previously. Perform antibody identification (IPP707 Antibody Identification) if antibody has not been previously identified. If an antibody has been previously identified, ensure no additional antibodies have been formed. Run at least one cell positive for the antigen corresponding to each previously identified
Page 92 of 95
1.2.2
1.2.3
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
antibody in order to get an indication of the expected titration and to ensure the antibody is still reactive. 1.3 Titre each clinically significant antibody identified. 1.4 Label 2 sets of test tubes, one set for current sample; one set for the previous sample. The first tube is 1:1 (undiluted), then 1:2, 1:4, etc. through 1:1024. 1.5 To both sets of tubes, add 100 L of 6% albumin to all tubes except the first. 1.6 Add 100 L of serum to tube #1 and tube #2. 1.7 Using a clean pipette tip, mix the contents of tube #2 several times. Transfer 100 uL to the next tube. 1.8 Continue with the same technique through all dilutions. From the last tube, remove 100 L of the diluted serum and save for use in further dilutions ineeded. 1.9 Prepare the red cell suspension. See Procedure Notes for selection of red cells. Wash the red cells and decant the saline completely. Resuspend to approximately 2-5% concentration with 6% albumin. 1.10 1.11 1.12 Add 100 L of the appropriate red cell suspension to each tube. Mix well and incubate at 37C for 30 minutes. After incubation, wash cells four (4) times and proceed with the antiglobulin phase. Beginning with final dilution, gently re-suspend the cell button and observe each tube macroscopically for agglutination until undiluted sample is read. Record the results on the Antibody Titration Worksheet (Appendix I). Grade reactions according to IPP624 Grading of Agglutination Reactions. Report the results. Store the remainder of the serum in freezer #3 according to Procedure Note 3.
1.13
1.14
1.15
2.
ABO Iso Titration: 2.1. Locate previous sample, if available, in Revco #3. Record previous results on Antibody Titration Worksheet (Appendix I). Perform ABO/Rh on current sample according to IPP701 ABO/Rh and Weak D Typing. Titer against A1 and/or B reagent red cells, as appropriate.
Page 93 of 95
2.2.
2.3.
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
2.4.
Label 2 sets of test tubes, one set for current sample; one set for the previous sample. The first tube is 1:1 (undiluted), then 1:2, 1:4, etc. through 1:1024. To both sets of tubes add 100L of saline to all tubes except the first tube. Add 100 L of serum to tube #1 and to tube #2. Using a clean pipette tip, mix the contents of tube #2 several times. Transfer 100 L to the next tube. Continue with the same technique through all dilutions. From the last tube, remove 100 L of the diluted serum and save for use in further dilutions if needed. Prepare the red cell suspension. Wash the red cells and decant the saline completely. Resuspend to approximately 2-5% concentration with saline. Add 100 L of the appropriate red cell suspension to each tube. Mix well and incubate at room temperature for 30 minutes. Centrifuge for time indicated on centrifuge. Beginning with final dilution, gently resuspend the cell button and observe each tube macroscopically for agglutination until undiluted sample is read. Record the results on the Antibody Titration Worksheet (Appendix I). Grade reactions according to IPP624 Grading of Agglutination Reactions. Report the results. Store the remainder of the serum in freezer #3 according to Procedure Note 3.
2.5.
2.6. 2.7.
2.8.
2.9.
2.10. 2.11. 2.12. 2.13.
2.14.
2.15.
3.
DTT Titration: 3.1. Treatment of Serum: 3.1.1. Mix 0.3 mL of serum and 0.3 mL of 0.01M DTT in a labeled tube. 3.1.2. In another tube (control), mix 0.3 mL of serum and 0.3 mL of saline. 3.1.3. Incubate at 37C for 15 minutes. 3.2. Titration:
Page 94 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3.2.1. Label 2 sets of tubes, one set for the DTT treated serum and one set for the saline / serum control. The first tube is a 1:2 dilution, then 1:4, 1:8, 1:16, etc. through 1:512. 3.2.2. To both sets of tubes add 100 L of 6% albumin to all tubes except the first. 3.2.3. To the appropriate set of tubes, add 0.1 mL of the DTT or saline treated serum to the first and the second tubes of each titration. 3.2.4. Using a clean pipette tip, mix the contents of tube #2 several times. Transfer 100 L to the next tube. 3.2.5. Continue the same technique through all dilutions. From the last tube remove 100 L of the diluted serum and save for use if further dilutions are needed. 3.2.6. Prepare the red cell suspension. See Procedure Notes for selection of red cells. Wash the red cells and decant the saline completely. Resuspend to approximately 2-5% concentration with 6% albumin. 3.2.7. Add 100 L of the appropriate red cell suspension to each tube. 3.2.8. Mix well and incubate at 37C for 30 minutes. 3.2.9. After incubation, wash cells four (4) times and proceed with the antiglobulin phase. 3.2.10. Beginning with final dilution, gently resuspend the cell button and observe each tube macroscopically for agglutination until undiluted sample is read. 3.2.11. Record the results on the IgG Titers Using DTT worksheet (Appendix II). Grade reactions according to IPP624 Grading of Agglutination Reactions. 3.2.12. Report the results. Store the remainder of the serum in freezer #3 according to Procedure Note 3.
CALCULATIONS Assign each agglutination a score and total all score values for each sample.
REPORTING RESULTS
Page 95 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Report the highest dilution that produces 1+ macroscopic agglutination. Do not report weak or microscopic reactions. Report results as the reciprocal of the highest dilution that shows 1+ macroscopic agglutination. (Report titer as 32; not 1:32). If 1:1024 dilution is positive report as Greater than 1024. Reporting Antibody Titre Results in Cerner Antibody titre results will be entered into Cerner using textual result entry under BLOOD BANK RESULT ENTRY. 3.1 Complete the New Worksheet Dialogue box, select the accession number format and press OK.
3.2 Enter the accession number associated with the antibody titration to be resulted. 3.3 The system retrieves order information and reference data for use in the worksheet. Click on, or use the arrow key to move to the cell to be resulted, represented by a white cell in the worksheet.
3.4
3.5 Press the SPACE BAR to open text editor window and press F2 to open the Select Template Dialogue box. 3.6 In the Activity Type box, select BLOOD BANK. 3.6.1 If the name of the template is known, type it in the Name box and press FIND. If not, a search can be performed by: Entering the first letter of the template and clicking FIND or ENTER. Pressing the SPACE BAR and clicking FIND or ENTER. This will bring up all Blood bank templates. 3.7 Select the Antibody Titre template and press OK. 3.8 Press F3 to move from one underscore (_) to the next. 3.9 Click OK to close the text editor window and Click PERFORM or VERIFY to save the results. 3.10 4. Add a comment, DTT used for titration. if applicable.
A two tube change in titer or a score difference of 10 is considered significant.
5. If previous titer is greater than 1024, do not repeat. Enter a comment as above "Not Indicated; previous titer on (date) was greater than 1024. Reporting ABO ISO Titer Results:
Page 96 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
6.1.
Report current results of previous sample at the Previous Titer prompt. This can be done using the same titer and score templates as described in AB Titer result entry above. (Do not report the result that was previously reported). If these results are significantly different (greater than 1 tube) from the previous reported results discuss with senior technologist prior to reporting results.
6.3 Add result comment, DTT used for titration if applicable.
DTT Interpretation: 7.1 Identical titers and strength of agglutination in both the test (DTT) and control is (saline) tubes denotes that neutralization has not taken place and that the antibody is IgG. 7.2 Inhibition of agglutination in the test (DTT) sample but not the control (saline) sample denotes that neutralization has occurred, and that the antibody is IgM. 7.3 Mixtures of IgG and IgM will show partial neutralization.
PROCEDURE NOTES 1. Select cells which will react strongest with the antibody being titrated; i.e., cells which are homozygous for the corresponding antigen. If a single antibody is present, select cell according to the following chart: Antibody anti-D, anti-c, anti-E anti-C, anti-e anti-K anti-A anti-B Cell Phenotype R2R2 R1R1 Kk A1 B
If multiple antibodies are present, select cells positive for antigens of the antibody to be titrated and negative for antigens of the other antibodies present. Select a cell with heterozygous expression when titrating anti-K, since it is usually not possible to select a cell with homozygous expression of the Kell antigen. This will ensure consistency from one anti-Kell titration to the next. 2. If an IgM antibody, other than Anti-A or Anti-B, is to be titered; 0.9% Saline is the preferable diluent. Incubate at room temperature for 30 minutes. Specimen storage:
Page 97 of 95
3.
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
3.1
Place frozen sample in freezer #3 in Antibody Titer Box #2; place sample in row corresponding to last digit of medical record number. Write sample information in Frozen Specimen Log. Cross out specimen when removing from box for subsequent testing or for discard. Retain frozen samples for one year.
3.2
3.3
LIMITATIONS OF PROCEDURES Technical factors will affect the results. To reduce these variables to a minimum: 1. 2. Meticulous pipetting is essential. Change tips between tubes. Optimum incubation time, temperature and dilution medium should be determined and used consistently. The age, phenotype and concentration of the test RBCs may affect the results. When the titers of several different examples of an antibody are to be compared, all sera should be tested against a pool of reagent RBCs from donors of the same phenotype
3.
4. Completely reproducible results are virtually impossible to achieve. Comparisons are only valid when specimens are tested concurrently. In prenatal testing, when sequential serum samples are tested for changing antibody titer, samples should be frozen for comparison with subsequent specimens. Each new sample should be tested in parallel with the immediate preceding sample.
REFERENCES 1. AABB Technical Manual, 13th edition. Bethesda, MD: American Association of Blood Banks, 1999. 2. Cerner HNA Millenium Integrated Clinical Information System PathNet User Training st Manual, 1 Edition, King Faisal Specialist Hospital and Research Center, July 2002.
Page 98 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
Page 99 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
ANTIBODY TITRATION
PATIENT NAME ANTIBODY (IES) IDENTIFIED: PATIENT MR#
DILUENT:
CURRENT TITRATION RED CELL USED:
PREVIOUS TITRATION DATE DONE:
INCUBATION TEMPERATURE:
INCUBATION TIME:
RESULTS:
USE A NEW SHEET FOR EACH ANTIBODY TITERED CURRENT SPECIMEN SPECIMEN DATE: ANTIBODY BEING TITERED: GRADE CCC SCORE PREVIOUS SPECIMEN SPECIMEN DATE: ANTIBODY BEING TITERED: GRADE CCC SCORE
DILUTION 1:1 1:2 1:4 1:8 1:16 1:32 1:64 1:128 1:256 1:512 1:1024
TITER:
TOTAL SCORE
TITER:
TOTAL SCORE
AGGLUTINATION SCORE: ALIQUOT FROZEN? YES / NO
4+ = 12
3+ =10
2+ = 8
1+ = 5
Performed By____________________________
Date_______________
Page 100 of 95
King Faisal Specialist Hospital and Research Center
Blood Bank Internal Policy / Procedure
IgG TITRATION USING DTT
PATIENT NAME ANTIBODY:
PATIENT MR#
DILUENT:
CURRENT TITRATION RED CELL USED:
PREVIOUS TITRATION DATE DONE:
INCUBATION TEMPERATURE:
INCUBATION TIME:
RESULTS:
USE A NEW SHEET FOR EACH ANTIBODY TITERED
DTT TREATED SERUM
CURRENT SAMPLE DILUTION GRADE CCC PREVIOUS SAMPLE GRADE CCC
SALINE TREATED SERUM
(CONTROL)
CURRENT SAMPLE GRADE CCC PREVIOUS SAMPLE GRADE CCC
1:1 1:2 1:4 1:8 1:16 1:32 1:64 1:128 1:256 1:512
ND
ND
ND
ND
ND
ND
ND
ND
TITRE:
TITRE:
TITRE:
TITRE:
ALIQUOT FROZEN? Y / N Interpretation (IgG and/or IgM) : _______________________________________
Performed By____________________________
Date_______________
Page 101 of 95
You might also like
- Essentials of ABO -Rh Grouping and Compatibility Testing: Theoretical Aspects and Practical ApplicationFrom EverandEssentials of ABO -Rh Grouping and Compatibility Testing: Theoretical Aspects and Practical ApplicationRating: 5 out of 5 stars5/5 (1)
- Clinical Chemistry, Immunology and Laboratory Quality Control: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeFrom EverandClinical Chemistry, Immunology and Laboratory Quality Control: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeRating: 5 out of 5 stars5/5 (1)
- Transfusion Medicine for Pathologists: A Comprehensive Review for Board Preparation, Certification, and Clinical PracticeFrom EverandTransfusion Medicine for Pathologists: A Comprehensive Review for Board Preparation, Certification, and Clinical PracticeRating: 3 out of 5 stars3/5 (1)
- Hematology and Coagulation: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeFrom EverandHematology and Coagulation: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeRating: 5 out of 5 stars5/5 (2)
- Blood Bank Harmening Chapter 10Document14 pagesBlood Bank Harmening Chapter 10ichummy19100% (3)
- Urinalysis and Body Fluids for Cls & MltFrom EverandUrinalysis and Body Fluids for Cls & MltNo ratings yet
- Other Blood Group SystemsDocument2 pagesOther Blood Group SystemsRachel ManaloNo ratings yet
- Blood Bank ProceduresDocument33 pagesBlood Bank Proceduresninadroy2844100% (19)
- Self-assessment Q&A in Clinical Laboratory Science, IIIFrom EverandSelf-assessment Q&A in Clinical Laboratory Science, IIIRating: 3 out of 5 stars3/5 (1)
- Blood Bank 2Document21 pagesBlood Bank 2moonfire2009No ratings yet
- Blood Bank PracticalDocument24 pagesBlood Bank Practicalmoonfire2009No ratings yet
- Blood Banking and Transfusion Medicine 2 PDFDocument891 pagesBlood Banking and Transfusion Medicine 2 PDFAaron Wallace100% (15)
- Blood Bank Review 2019 PDFDocument613 pagesBlood Bank Review 2019 PDFCuddles Pingoy100% (1)
- Blood Bank 3Document20 pagesBlood Bank 3moonfire2009100% (2)
- WHO Blood Bank SOPsDocument116 pagesWHO Blood Bank SOPsambitiousamit83% (12)
- Blood Banking ReviewDocument442 pagesBlood Banking ReviewMayra Flor100% (2)
- Accurate Results in the Clinical Laboratory: A Guide to Error Detection and CorrectionFrom EverandAccurate Results in the Clinical Laboratory: A Guide to Error Detection and CorrectionRating: 5 out of 5 stars5/5 (1)
- Aabb Antibody Id ApproachDocument127 pagesAabb Antibody Id ApproachRounak Dubey29% (7)
- Laboratory Total Quality Management for Practitioners and Students of Medical Laboratory ScienceFrom EverandLaboratory Total Quality Management for Practitioners and Students of Medical Laboratory ScienceRating: 5 out of 5 stars5/5 (3)
- Pre Transfusion TestingDocument57 pagesPre Transfusion TestingDominic Bernardo100% (4)
- Antibody IdentificationDocument74 pagesAntibody IdentificationNilver Zenteno100% (3)
- Transfusion Medicine and Hemostasis: Clinical and Laboratory AspectsFrom EverandTransfusion Medicine and Hemostasis: Clinical and Laboratory AspectsRating: 4 out of 5 stars4/5 (9)
- Blood Bank Practical Panel CasesDocument23 pagesBlood Bank Practical Panel CasesMiguel Vasquez0% (1)
- Blood Bank Case StudyDocument17 pagesBlood Bank Case StudyMelissa Harding33% (3)
- Medical Laboratory Technician: Passbooks Study GuideFrom EverandMedical Laboratory Technician: Passbooks Study GuideNo ratings yet
- Other Blood Group System AssignmentDocument5 pagesOther Blood Group System AssignmentMary ChristelleNo ratings yet
- Quick guide to Laboratory Medicine: a student's overviewFrom EverandQuick guide to Laboratory Medicine: a student's overviewNo ratings yet
- Blood Banking by BMTDocument126 pagesBlood Banking by BMTRachel Marie M. Gania100% (2)
- AABB Primer of Blood AdministrationDocument112 pagesAABB Primer of Blood AdministrationMohamed ElmasryNo ratings yet
- 24, Standards For Blood Banks and Blood Transfusion ServicesDocument111 pages24, Standards For Blood Banks and Blood Transfusion ServicesShiv Shankar Tiwari67% (3)
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4From EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4No ratings yet
- Medical Laboratory Sample QuestionsDocument6 pagesMedical Laboratory Sample Questionszopito100% (1)
- ImmunohematologyDocument11 pagesImmunohematologydtimtimanNo ratings yet
- Handbook of Transfusion MedicineFrom EverandHandbook of Transfusion MedicineChristopher HillyerRating: 4 out of 5 stars4/5 (4)
- Quality Assurance in The Blood BankDocument41 pagesQuality Assurance in The Blood Bankgauravmahajan4480% (5)
- DNA Replication, Genetics, Immunology, Blood GroupsDocument8 pagesDNA Replication, Genetics, Immunology, Blood Groupsadagay100% (1)
- Transfusion MedicineDocument396 pagesTransfusion Medicinemjtjdomingo85% (26)
- IMMUNOHEMATOLOGY AND BLOOD BANKING: Passbooks Study GuideFrom EverandIMMUNOHEMATOLOGY AND BLOOD BANKING: Passbooks Study GuideRating: 1 out of 5 stars1/5 (1)
- Transfusion TherapyDocument14 pagesTransfusion TherapyCMLNo ratings yet
- AABB Technical Manual 15TH PDFDocument931 pagesAABB Technical Manual 15TH PDFnanaNo ratings yet
- Clinical Chemistry NotesDocument24 pagesClinical Chemistry Notesclower112100% (3)
- Introduction to Medical Laboratory TechnologyFrom EverandIntroduction to Medical Laboratory TechnologyRating: 2.5 out of 5 stars2.5/5 (7)
- Antibody Screening and IdentificationDocument13 pagesAntibody Screening and IdentificationAnonymouscatNo ratings yet
- ImmunoassayFrom EverandImmunoassayEleftherios P. DiamandisRating: 5 out of 5 stars5/5 (1)
- Strasinger Q&A BLANKDocument68 pagesStrasinger Q&A BLANKJayniel MollenoNo ratings yet
- Abo Typing Discrepancies: Rene Jesus Alfredo R. Dinglasan, RMTDocument14 pagesAbo Typing Discrepancies: Rene Jesus Alfredo R. Dinglasan, RMTdirenjan100% (1)
- Important new certification infoDocument28 pagesImportant new certification infoMuhammad umarNo ratings yet
- SUCCESS in Clinical Laboratory Science PDFDocument1 pageSUCCESS in Clinical Laboratory Science PDFDaryl Langamon Uy Cruz67% (3)
- BloodbankDocument433 pagesBloodbankFait Hee95% (22)
- Study Stack - M (ASCP) EXAM Table Review PDFDocument9 pagesStudy Stack - M (ASCP) EXAM Table Review PDF장주연100% (2)
- Tarif B Tahun 2020 RLSDocument55 pagesTarif B Tahun 2020 RLSLaboratory SHBTNo ratings yet
- Association of Veterinary Hematology and Transfusion Medicine (AVHTM) Transfusion Reaction Small Animal Consensus Statement (TRACS) Part 2 - Prevention and MonitoringDocument22 pagesAssociation of Veterinary Hematology and Transfusion Medicine (AVHTM) Transfusion Reaction Small Animal Consensus Statement (TRACS) Part 2 - Prevention and MonitoringLaboratório de Patologia ClínicaNo ratings yet
- Table of Blood Group SystemsDocument3 pagesTable of Blood Group SystemsElizabeth MedinaNo ratings yet
- SL ReportDocument2 pagesSL Reportakshay kachwayaNo ratings yet
- 10 - Ag PhenotypeDocument6 pages10 - Ag PhenotypeBromance H.No ratings yet
- Blood TranfusionDocument18 pagesBlood TranfusionVishnu PriyaNo ratings yet
- Massive Haemorrhage: P Donnelly B FergusonDocument18 pagesMassive Haemorrhage: P Donnelly B FergusonRizqiNo ratings yet
- Icd 10Document5 pagesIcd 10Andriyan KardhaniNo ratings yet
- Referat Thalasemia MajorDocument21 pagesReferat Thalasemia Majoreryprayudi13No ratings yet
- The Composition of Blood: Fact Sheet: Blood PlasmaDocument1 pageThe Composition of Blood: Fact Sheet: Blood PlasmaKoshkaNo ratings yet
- BLOOD-BANK - Blood ComponentsDocument27 pagesBLOOD-BANK - Blood ComponentsShannie MacatuggalNo ratings yet
- Tiruneh 2020Document5 pagesTiruneh 2020Shafici CqadirNo ratings yet
- ImmunohematologyDocument67 pagesImmunohematologyRainbow SherbetNo ratings yet
- Medtecg Sir Judecribd NiDocument11 pagesMedtecg Sir Judecribd NiSUPPLY OFFICERNo ratings yet
- I Need To Know About Fresh Frozen Plasma: BloodDocument1 pageI Need To Know About Fresh Frozen Plasma: BloodHumberto OmaresNo ratings yet
- Blood Bank ManualDocument29 pagesBlood Bank ManualMarice Ferrufino SchmidtNo ratings yet
- BLOOD PRODUCT TRANSFUSIONS DEFINITIONS AND TRANSFUSION REACTIONSDocument1 pageBLOOD PRODUCT TRANSFUSIONS DEFINITIONS AND TRANSFUSION REACTIONSjuan ramon milanes grageraNo ratings yet
- Biological Referance Interval: Negative 11.0Document2 pagesBiological Referance Interval: Negative 11.0Huzaiful ReyazNo ratings yet
- Elution and Adsorption TechniquesDocument23 pagesElution and Adsorption TechniquesBromance H.No ratings yet
- Lecture10 - Blood Groups and TransfusionDocument28 pagesLecture10 - Blood Groups and Transfusionmohapatrarashmi050No ratings yet
- Coomb's Test GuideDocument26 pagesCoomb's Test Guidelubna aloshibiNo ratings yet
- Miner Blood Group SystemDocument44 pagesMiner Blood Group SystemArshad RazaqNo ratings yet
- Shalamar Hospital Laboratory: Blood BankDocument2 pagesShalamar Hospital Laboratory: Blood BankSuleman RasheedNo ratings yet
- Lab Ex. 1 5Document5 pagesLab Ex. 1 5LUZVIMINDA GORDONo ratings yet
- NTA - GPAT 2022 Examination: Subject: Pharmaceutical Chemistry SET 02Document48 pagesNTA - GPAT 2022 Examination: Subject: Pharmaceutical Chemistry SET 02BvayNo ratings yet
- 4th (Regional Administrative Order)Document12 pages4th (Regional Administrative Order)Naruto UzumakiNo ratings yet
- Blood Bank ProposalDocument31 pagesBlood Bank Proposalzfnef608No ratings yet
- Characteristics of Blood Group Antibodies Immunoglobulin Classes and In Vitro PropertiesDocument1 pageCharacteristics of Blood Group Antibodies Immunoglobulin Classes and In Vitro PropertiesyepNo ratings yet
- An Audit of Blood Bank Services: Journal of Education and Health Promotion February 2014Document4 pagesAn Audit of Blood Bank Services: Journal of Education and Health Promotion February 2014surigao doctors'No ratings yet
- Immunohematology QuizletDocument28 pagesImmunohematology QuizletReizel GaasNo ratings yet