Professional Documents
Culture Documents
Assessment of Vital Signs&GCS
Uploaded by
Nicole JacksonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessment of Vital Signs&GCS
Uploaded by
Nicole JacksonCopyright:
Available Formats
Assessment of Vital Signs
Vital signs provide important, basic information about a persons’ physiological state.
These relate primarily to cardiac and respiratory function and include pulse, blood
pressure, temperature and respiratory rate.
Pulse
The following should be considered when observing the pulse,
- the rate of the pulse
- rhythm
- radiofemoral pulse
Rate - In healthy adults the resting heart rate should be between 60 and 100 beats per
minute. (bpm)
A heart rate of less than 60 pbm is known as Bradycardia
A heart rate of more than 100 pbm is known as Tachycardia
Rhythm – The heart contracts (beats) and pumps blood with a regular rhythm, for
example, at a rate of 60 beats per minute there is a beat every second. The heart may beat
faster or slower with a shorter or longer interval between beats, but at any one rate the
interval between beats is constant. This regular rhythm occurs as a result of regular
electrical discharges (currents) that travel through the heart and cause the muscle of the
heart to contract. In an irregular heart beat, the electrical discharges are irregular and
rapid and, as a result, the heart beats irregularly and, usually, rapidly.
(Some extra notes….
Aortic regurgitation, or anaemia (red blood cell count/hemoglobin count is less than
normal) for example are causes of a large stroke volume and typically produce a
bounding pulse with a wide amplitude.
Aortic stenosis (an abnormal narrowing of the aortic valve) impedes ventricular emptying
and may cause a slow rising, weak and delayed pulse)
Radiofemoral pulse – this is assessed by measuring the radial pulse (felt just medial to the
radius the forefinger and middle finger pulps of hand) and the femoral pulse (found one
third of the way up from the pubic tubercle, situated below the inguinal ligament). The
delay between the two can be reflective of what is happening at the deeper level where
the ductus arteriosus (A key arterial shunt) joins the descending aorta.
Blood Pressure (BP)
In healthy adults,
the Systolic BP falls between 90 & 120mm Hg
the Diastolic BP falls between 60 & 80mm Hg
The blood pressure is measured using a sphygmomanometer and uses a 12.5cm wide cuff
which wraps over the brachial artery (The artery that runs from the shoulder down to the
elbow). For an approximate estimation of the systolic blood pressure the cuff is fully
inflated and then deflated slowly (3-4mmHg per second) until the radial pulse returns.
The pressure at which the sound is first heard is the systolic blood pressure, and the
pressure at which the sound finally disappears is the diastolic blood pressure.
Pressure may vary in the arms and the legs.
Temperature
In healthy adults, the normal temperature ranges between 36.6 C and 37.2 C (98F and
99F). It should be noted that in very hot weather the temperature may rise by 0.5 C. There
is also diurnal variation where the body temperature is lowest in the morning and reaches
its peak between 1800hours and 2000hours. This is relevant as ‘fever-pattern’ (febrile
pattern) of most diseases follows this diurnal variation. The three main areas where
temperature recording are often made are mouth, axilla (the cavity beneath the junction of
the arm and the body) and the rectum. The normal, average temperature of these 3 areas
differs, 36.8 C, 36.4 C and 37.3 C respectively, with an increase of 0.5 C considered to be
an indicator of a fever.
Respiratory Rate
The number of breaths per minute or, more formally, the number of movements
indicative of inspiration and expiration per unit time. In practice, the respiratory rate is
usually determined by counting the number of times the chest rises or falls per minute.
By whatever means, the aim is to determine if the respirations are normal, abnormally
fast (tachypnea), abnormally slow (bradypnea), or nonexistent (apnea)
Glasgow Coma Scale
The assessment of conscious level is an essential part of the neurological examination.
The patients level of arousal and response to stimuli can be graded on the ‘Glasgow
Coma Scale’ (GCS) using a numerical scale which allows for comparison and may
provide prognostic information. The GCS is divided in to 3 categories, and are as
follows.
Eye Opening (E)
- Spontaneous 4
- To speech 3
- To pain 2
- Nil 1
Best Motor Response (M)
- Obeys 6
- Localises 5
- Withdraws 4
- Abnormal flexion 3
- Extensor response 2
- Nil 1
Verbal Response (V)
-Orientated 5
- Confused conversation 4
- Inappropriate words 3
- Incomprehensible sounds 2
- Nil 1
Scores are tallied by the equation
Coma Scale = E + M + V
A score of 15 equates to full consciousness, 12-14 the person may be awake but ‘cloudy’,
scores of 8 or under equate to the person in a coma state. In terms of prognosis, scores of
4 or less generally have a very poor prognosis, and scores of 11 or more have a good
prognosis for recovery.
REVIEW OF FIRST AID ASSESSMENT
(This is all courtesy of the Australian Red Cross)
Basic Life Support Flow Chart
D Check for Danger/Safety (of yourself/victim)
R Check Response to voice/touch/check for signs of life (If no, call 000/112)
A Clear and open the Airway (in position they are in or move to recover position if
more suitable
B Give 2 Breaths if not breathing normally (watch for the chest to rise and fall)
Recheck for signs of life
C Give 30 chest Compressions (compressions made on the sternum using 2 hands –
find the notch where the ribs meet in the centre and compress 1/3 of chest depth)
compressions given at rate of 100 per minute, followed by 2 more breaths
D Defibrillate – attach AED as soon as available
The role of a ‘first-aider’ is to continue with CPR until qualified personnel arrive or signs
of life return. In this context, ‘no signs of life’ is defined as no response (unconscious),
not breathing normally, not moving.
Care is needed when given resuscitation to a child aged between one and eight years and
only hand should be used to give compressions, being aware not to compress to high or
too low. Special care is needed when giving CPR to babies under 1 year of age. Only 2
fingers should be used to give compressions, and the breaths given should be ‘puffs’. The
same steps and principals apply to adults, children and babies, and the same 2/30 ratio
applies to all.
*Pregnant women in their last weeks of pregnancy should have padding put under their
right buttock to tilt her hips left (Left Lateral Tilt) as this allows free movement of blood
back to the heart. When in this position CPR may begin.
You might also like
- High Blood Pressure: Safe alternatives without drugsFrom EverandHigh Blood Pressure: Safe alternatives without drugsRating: 5 out of 5 stars5/5 (2)
- Clinical Procedures For Medical AssistantDocument40 pagesClinical Procedures For Medical AssistantStudent1010No ratings yet
- M.Heldi Riyanda 19334059 B InggrisDocument3 pagesM.Heldi Riyanda 19334059 B InggrisBintan NajihanNo ratings yet
- Vital Sign Na (1) by ZWBDocument52 pagesVital Sign Na (1) by ZWBAshraf Ali100% (1)
- Vital SignDocument100 pagesVital SignIbnu FuqonNo ratings yet
- Vital SignsDocument5 pagesVital SignsFrances Kaye Sta. CruzNo ratings yet
- NSTP1 Vital SignsDocument31 pagesNSTP1 Vital SignsCarmie CasañasNo ratings yet
- Vital Signs (BHW Training) 2Document31 pagesVital Signs (BHW Training) 2Yathziel Meow100% (4)
- Vital SignsDocument10 pagesVital SignsEdelou Alegria JumawanNo ratings yet
- Aristotle C. Castronuevo BSN 1-1Document16 pagesAristotle C. Castronuevo BSN 1-1Aristotle Calayan CastronuevoNo ratings yet
- Blood and Pulse Measaurment Topic 1Document17 pagesBlood and Pulse Measaurment Topic 1Amro AzrakNo ratings yet
- PHYSICAL EXAMINATION GeneralitatiDocument12 pagesPHYSICAL EXAMINATION GeneralitatiMarianNo ratings yet
- Vital Signs Examination - Kuliah SMT 2 2008Document54 pagesVital Signs Examination - Kuliah SMT 2 2008VilasineeAriHaraKumarNo ratings yet
- Basic Clinical SkillsDocument4 pagesBasic Clinical Skillsbijuiyer5557No ratings yet
- 1 - Vital SignsDocument27 pages1 - Vital Signshawdeng xalitNo ratings yet
- LRI1.1 Identify Vital Information of The ClientDocument6 pagesLRI1.1 Identify Vital Information of The ClientHannah May Abigail CortadoNo ratings yet
- Course: Emergency Procedures and Patient Care Lecture-6Document38 pagesCourse: Emergency Procedures and Patient Care Lecture-6saba ramzanNo ratings yet
- Vital SignDocument100 pagesVital SignZubda ButtNo ratings yet
- Vital SignsDocument10 pagesVital SignsMuhammad FahmyNo ratings yet
- Vital SignDocument100 pagesVital SignMj EncinaNo ratings yet
- Cned Handbook Single Page1 1Document40 pagesCned Handbook Single Page1 1api-300218860No ratings yet
- Group 5 Vital SignsDocument27 pagesGroup 5 Vital SignsGelique AnterolaNo ratings yet
- Vital Signs/'Document30 pagesVital Signs/'Monika MinhasNo ratings yet
- Resume Vital Sign ExaminationDocument6 pagesResume Vital Sign ExaminationRedmy LasmanaNo ratings yet
- HILOT WELLNESS MASSAGE NC II 2nd TopicDocument17 pagesHILOT WELLNESS MASSAGE NC II 2nd TopicClydie Joy100% (2)
- Objectives:: Exercise PersonDocument11 pagesObjectives:: Exercise PersonArchie CabacheteNo ratings yet
- NSTP12 FinalDocument16 pagesNSTP12 FinalJhonny pingolNo ratings yet
- General Survey AssessmentDocument56 pagesGeneral Survey Assessmentdanny_ng080% (1)
- First Aid and Water SafetyDocument14 pagesFirst Aid and Water SafetyASHLEY JOY ARZADON (SCJE)No ratings yet
- Fakultas Kedokteran UnisbaDocument28 pagesFakultas Kedokteran UnisbadeasyahNo ratings yet
- Kmedical Definition of Respiratory RateDocument65 pagesKmedical Definition of Respiratory RateKebede KassuNo ratings yet
- Vital SignsDocument4 pagesVital SignsPatricia MendozaNo ratings yet
- CBR Report - Vital SignsDocument6 pagesCBR Report - Vital Signsteddy_tudsNo ratings yet
- Vital Signs (Body Temperature, Pulse Rate, Respiration Rate, Blood Pressure)Document21 pagesVital Signs (Body Temperature, Pulse Rate, Respiration Rate, Blood Pressure)Ira Nur HumairaNo ratings yet
- Cardiovascular AssessmentDocument73 pagesCardiovascular AssessmentmatthewsarfrazbhattiNo ratings yet
- Vital Signs: DiaphragmDocument18 pagesVital Signs: DiaphragmLenjoy CabatbatNo ratings yet
- Vital SignsDocument38 pagesVital SignsSanjna Kumari (SNSR Senior Tutor/Lecturer)100% (1)
- Vitalsigns 180617200506Document34 pagesVitalsigns 180617200506Maricris Tac-an Calising-PallarNo ratings yet
- Equipment Used in Exercise Physiology and Its UsesDocument55 pagesEquipment Used in Exercise Physiology and Its UsesAkshayNo ratings yet
- Vital Signs and Their Clinical SignificanceDocument30 pagesVital Signs and Their Clinical Significanceabineupane11No ratings yet
- Vital SignsDocument5 pagesVital SignsazazelrallosNo ratings yet
- Measuring Vital Signs: How To Take Blood PressureDocument5 pagesMeasuring Vital Signs: How To Take Blood PressureErin BarnesNo ratings yet
- Assessing Radial PulseDocument18 pagesAssessing Radial PulseJoisy AloorNo ratings yet
- Vital Signs SabansiDocument116 pagesVital Signs SabansiTariku olanaNo ratings yet
- RBI-Vital-Signs-Wellness MassageDocument36 pagesRBI-Vital-Signs-Wellness Massagema.fatima ravalo rabulanNo ratings yet
- Basic Health Care Skills: How To Measure Vital Signs Vital SignsDocument8 pagesBasic Health Care Skills: How To Measure Vital Signs Vital SignsJoan BarcenasNo ratings yet
- Baseline Vital Kefah 1BDocument38 pagesBaseline Vital Kefah 1BShahd Abu SnenehNo ratings yet
- Physical DiagnosisDocument42 pagesPhysical DiagnosisKhim Yalong100% (1)
- Health AssessmentDocument4 pagesHealth Assessmentoshiz2000No ratings yet
- Physical Exam Final Written Exam Study Guide 2Document51 pagesPhysical Exam Final Written Exam Study Guide 2pelly3190100% (2)
- Assessing Apical PulseDocument5 pagesAssessing Apical PulseMatthew Ryan100% (1)
- Vital Sign 1Document34 pagesVital Sign 1wowila6489No ratings yet
- Cardiovascular Assessment (1) - StudentsDocument70 pagesCardiovascular Assessment (1) - Studentsraima ayazNo ratings yet
- Vital-Signs (Quiz Nalang Kulang)Document51 pagesVital-Signs (Quiz Nalang Kulang)Hannah TollenoNo ratings yet
- FundaDocument5 pagesFundaGreggy Francisco LaraNo ratings yet
- PulseDocument13 pagesPulseArdi EroNo ratings yet
- Blood Pressure and The PulseDocument4 pagesBlood Pressure and The PulseGeorge OstNo ratings yet
- Pengukuran Tekanan Darah Dan NadiDocument22 pagesPengukuran Tekanan Darah Dan NadiBellaNo ratings yet
- Blood Pressure: Step By Step Guide And Proven Recipes To Lower Your Blood Pressure Without Any MedicationFrom EverandBlood Pressure: Step By Step Guide And Proven Recipes To Lower Your Blood Pressure Without Any MedicationNo ratings yet
- IndexDocument3 pagesIndexBrunaJ.MellerNo ratings yet
- DaybreaksDocument14 pagesDaybreaksKYLE FRANCIS EVANo ratings yet
- Code of Conduct of Dabur Company - 1Document5 pagesCode of Conduct of Dabur Company - 1Disha KothariNo ratings yet
- Who Di 31-4 Atc-DddDocument6 pagesWho Di 31-4 Atc-DddHenderika Lado MauNo ratings yet
- NIA Foundation PLI Proposal Template (Repaired)Document23 pagesNIA Foundation PLI Proposal Template (Repaired)lama dasuNo ratings yet
- ShakespeareDocument12 pagesShakespeareapi-510189551No ratings yet
- HRM848 Training Techniques and Practices Summer 2021Document39 pagesHRM848 Training Techniques and Practices Summer 2021Dhruvi RajNo ratings yet
- Victorian AOD Intake Tool Turning Point AuditDocument8 pagesVictorian AOD Intake Tool Turning Point AuditHarjotBrarNo ratings yet
- Wulandari - Solihin (2016)Document8 pagesWulandari - Solihin (2016)kelvinprd9No ratings yet
- Bottoms y Sparks - Legitimacy - and - Imprisonment - Revisited PDFDocument29 pagesBottoms y Sparks - Legitimacy - and - Imprisonment - Revisited PDFrossana gaunaNo ratings yet
- Muzakarah Jawatankuasa Fatwa Majlis Kebangsaan Bagi Hal Ehwal Ugama Islam Malaysia Kali KeDocument7 pagesMuzakarah Jawatankuasa Fatwa Majlis Kebangsaan Bagi Hal Ehwal Ugama Islam Malaysia Kali KeSiti Zubaidah ZulkhairieNo ratings yet
- Creativity and AestheticDocument17 pagesCreativity and AestheticSyahirah Erahzs100% (1)
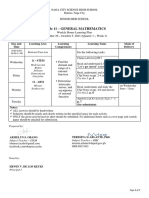
- General Mathematics - Module #3Document7 pagesGeneral Mathematics - Module #3Archie Artemis NoblezaNo ratings yet
- SG Insert SpecificationDocument16 pagesSG Insert SpecificationRaamkriss Raja100% (2)
- Ebook Fulfilling Destiny As Demanded by GodDocument94 pagesEbook Fulfilling Destiny As Demanded by GodIfeanyi OmeiheakuNo ratings yet
- Lecture - 4 - 28june2023Document18 pagesLecture - 4 - 28june2023vanshikaNo ratings yet
- Renal CalculiDocument12 pagesRenal CalculiArieNo ratings yet
- CA IPCC Accounting Guideline Answers May 2015Document24 pagesCA IPCC Accounting Guideline Answers May 2015Prashant PandeyNo ratings yet
- ABS Parametric RollDocument2 pagesABS Parametric RollAdvan Zuidplas100% (1)
- Birth and Growth of Semiotics: November 2020Document9 pagesBirth and Growth of Semiotics: November 2020Maria del Carmen Alvarado AcevedoNo ratings yet
- SCHEEL, Bernd - Egyptian Metalworking and ToolsDocument36 pagesSCHEEL, Bernd - Egyptian Metalworking and ToolsSamara Dyva86% (7)
- Thompson VarelaDocument18 pagesThompson VarelaGiannis NinosNo ratings yet
- The Utopia of The Zero-OptionDocument25 pagesThe Utopia of The Zero-Optiontamarapro50% (2)
- Adeyinka Wulemat Olarinmoye - The Images of Women in Yoruban Folktales PDFDocument12 pagesAdeyinka Wulemat Olarinmoye - The Images of Women in Yoruban Folktales PDFAngel SánchezNo ratings yet
- Liquid Holdup in Large-Diameter Horizontal Multiphase PipelinesDocument8 pagesLiquid Holdup in Large-Diameter Horizontal Multiphase PipelinessaifoaNo ratings yet
- Creative LeadershipDocument6 pagesCreative LeadershipRaffy Lacsina BerinaNo ratings yet
- Evolution of Corporate Social Responsibility in IndiaDocument12 pagesEvolution of Corporate Social Responsibility in IndiaVinay VinuNo ratings yet
- Bhagavad Gita Ch.1 Shlok 4++Document1 pageBhagavad Gita Ch.1 Shlok 4++goldenlion1No ratings yet
- SSPC - Guia 12Document6 pagesSSPC - Guia 12José Alvaro Herrera Ramos50% (2)
- HDLSS Numerical Assignments - DOC FormatDocument3 pagesHDLSS Numerical Assignments - DOC FormatNikhil UpadhyayNo ratings yet