Professional Documents
Culture Documents
Laporan Kasus Ketuban Pecah Dini + Drip Oksitosin
Uploaded by
Putra MahautamaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Laporan Kasus Ketuban Pecah Dini + Drip Oksitosin
Uploaded by
Putra MahautamaCopyright:
Available Formats
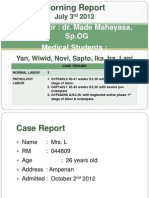
MORNING REPORT
September 14th, 2012
Supervisor : dr. Agus Rusdhy Hariawan Hamid, Sp.OG
Medical Students : Jun, Erma, Dini H, Dini F, Jatna
CASES RESUME NORMAL LABOR PATHOLOGY LABOR 1 1. G4P1A2L1 A/S/L/IU head presentation with laten phase 1st stage of labor + history CS 11 years ago + History rupture of membrane 2. G3P2A0L1 A/S/L/IU head presentation with PROM > 12 hours 3. G3P2A0H2 A/S/L/IU with PROM >12 hours
Name: Mrs.N Age: 27 yo Address: Kapu, Jenggara, Tanjung, KLU Admitted: September, 14th 2012 at 11.00 wita
TIME 14/09/ 2012 (11.00)
SUBJECTIVE Patient referred from Tanjung GH with G3P2A0L1 36-37 weaks/S/L/IU with PROM > 12 hours. Patient confessed rupture of membrane since 20.00 (13/09/2012). Abdominal pain (-). Bloody slim (-), FM (+). No history of DM, HT, asthma. LMP: forgot EDD : History of ANC: > 4 X posyandu Last ANC : 06-09-2012 Result : normal History of USG: never
OBJECTIVE General status: GC: well BP: 110/70 mmHg PR: 80 bpm RR: 20 T: 36,5OC Eye : anemis (-), icteric (-) Thorax : Cor : S1S2 single regular (murmur ), (gallop -) Pulmo : vesicular (+/+), wheezing (/-), Ronchi (-/-). Abdomen : scar (-), striae (+), linea nigra (+) Extremity : edema (-/-), warm acral (+/+) Obstetrical status: L1: breech L2: back on the left side L3: head L4: 4/5 UFH: 29 cm EFW: 2790 g UC : FHB: 11-11-11 (132 x/min) VT: 2 cm, eff 10 %, amnion (-), head palpable HI, impalpable small part / umbilical cord.
ASSESTMENT G3P2A0L1 A/S/L/IU head presentation with PROM > 12 hours
PLANNING Obs mother & fetal well being skin test ampi (-) Inj. Ampicillin 1 gr /6 hour IV DM announce to SPV pro induction with oxytocin drip if CTG reactive, advice: acc induction with drip oxytocin if CTG reactive
History of family planning : pill Next family planning : injection 3 month
Obstetrical history: I. , Premature, 2500 gram, RSU Tanjung, 12 yo II. , Aterm, 2500 gram, midwife, death 3 month III. This
TIME
SUBJECTIVE Chronology: 09.30 (14/09/2012) S: Patient referred from midwife came to Tanjung GH confessed rupture of membrane since 19.30 (13/09/2012). Bloody Slim (-). Abdominal pain (-). History of DM (-), asthma (--), HT (-) LMP: forgot EDD: O: GC: well BP: 100/70 mmHg PR: 80 bpm RR: 20 bpm T: 36,4oc L1: breech TFU : 27 cm L2: back on the left side TBJ : 2480 g L3: head L4: 4/5 23.30 (13-09-2012) UC: FHB: 12-12-11 (140 x/min) VT: 1 cm, eff 25 %, amnion (-), head palpable HI, denom unclear, impalpable small part / umbilical cord. 08.30 (14-09-2012) UC: FHB: 11-12-12 (140 bpm) VT: 1 cm, eff 25 %, amnion (-), head palpable HI, denom unclear, impalpable small part / umbilical cord. A:G3P2A0L1 36-37 weaks/S/L/IU with PROM > 12 hours. P: infuse RL 20 dpm inj. Ampicillin 1 gr (IV) 23.20 wita Obs mother & fetal well being Refer to NTB GH
OBJECTIVE PS: 5 Cervic dilatation 2 cm : 1 Cervix length 1 cm : 2 Cervix consistency moderate : 1 Cervix position posterior : 0 Station H I : 1
ASSESTMENT
PLANNING
Lab: HB: 13,1 g/dl RBC : 4,46 M/dl WBC : 6,7 K/dl PLT : 165 K/dl HbSAg: (-)
TIME 13.00 -
SUBJECTIVE
OBJECTIVE GC: well BP: 120/80 mmHg PR: 88 bpm RR: 20 T: 36,5 CTG: reactive UC: FHR: 11-12-13 (144 bpm )
ASSESTMENT G3P2A0L1 A/S/L/IU head presentation with PROM > 12 hours
PLANNING Flash I Drip oxy began 8 dpm
13.30
UC: FHR: 12-12-12 (144 bpm)
G3P2A0L1 A/S/L/IU head presentation with PROM > 12 hours
G3P2A0L1 A/S/L/IU head presentation with PROM > 12 hours G3P2A0L1 A/S/L/IU head presentation with PROM > 12 hours G3P2A0L1 A/S/L/IU head presentation with PROM > 12 hours G3P2A0L1 A/S/L/IU head presentation with PROM > 12 hours
Drip oxy 12 dpm
14.00
UC: FHR: 12-11-11 (136 bpm)
Drip oxy 16 dpm
14.30
UC: FHR: 11-11-12 (136 bpm)
Drip oxy 20 dpm
15.00
Abdominal pain came and relieved
UC: 2x/10 ~ 20 FHR: 12-12-12 (144 bpm)
Drip oxy 24 dpm
15.30
Abdominal pain came and relieved
UC: 2x/10 ~ 30 FHR: 12-11-12 (140 bpm)
Drip oxy 28 dpm
TIME 16.00
SUBJECTIVE Abdominal pain came and relieved
OBJECTIVE UC: 3x/10 ~ 30 FHR: 12-12-12 (144) VT: 3 cm, eff 25%, amnion (-), head palpable HI, impalpable small part of fetal/ umbilical cord UC : 3x/10 ~ 35 FHR : 12-12-13 (148 bpm) G3P2A0L1 A/S/L/IU head presentation latent phase 1st stage of labor with history rupture of membrane
PLANNING Drip oxy 32 dpm CTG, result: reactive
16.30
Abdominal pain came and relieved
Drip oxy 36 dpm
17.00
Abdominal pain came and relieved
UC: 3x/10 ~ 35 FHR: 12-13-13 (152 bpm)
Drip oxy 40 dpm
17.30
Abdominal pain came and relieved
UC: 4x/10 ~ 35 FHR: 12-12-12 (144 bpm) UC: 4x/10 ~ 35 FHR: 12-13-12 (148 bpm) UC: 4x/10 ~ 35 FHR: 12-11-13 (144 bpm)
Drip oxy 40 dpm
18.00
Abdominal pain came and relieved
Drip oxy 40 dpm
18.30
Abdominal pain came and relieved
Drip oxy 40 dpm
19.00
Abdominal pain came and relieved
UC: 4x/10 ~ 35 FHR: 12-12-12 (144 bpm) UC: 4x/10 ~ 35 FHR: 11-12-11 (136 bpm)
Flash II Drip oxy 40 dpm
19.30
Abdominal pain came and relieved
Drip oxy 40 dpm
TIME 20.00
SUBJECTIVE Abdominal pain came and relieved
OBJECTIVE UC: 4x/10 ~ 35 FHR: 13-12-13 (152 bpm) VT: 8 cm, effacement 75 %, amnion (-), head palpable HII denominator LOA, impalpable small part of fetal / umbilical cord G3P2A0L1 A/S/L/IU head presentation active phase 1st stage of labor with history rupture of membrane
PLANNING Drip oxy 40 dpm
20.30
Abdominal pain came and relieved Abdominal pain ++ Mother want to bearing down doran
UC: 4x/10 ~ 45 FHR: 12-12-12 (144 bpm) UC: 4x/10 ~ 45 FHR: 12-12-12 (144 bpm) Teknus perjol vulka 2nd stage of labor
Drip oxy 40 dpm
21.00
Drip oxy 40 dpm Conduct mother to bearing down Baby was born, male, AS 7-9, 2750 gram, 48 cm, Anus (+), congenital anomaly (-) Placenta was born spontaneous, complete, perineum intak bleeding 150cc
21.35
23.35
Delivery wound pain
GC: well Cons: CM BP: 120/70 HR: 84 bpm RR: 24 tpm T: 36,5 C UC: + UFH: 1 finger below umbilicus GC: well Cons: CM BP: 120/80 HR : 80 bpm RR : 20 tpm T : 36,4 C UFH : 1 finger below umbilicus UC : + Baby rooming in PR: 120 RR: 44 T: 36,7
2 day post partum
Observed mother and baby well being Suggest mother to mobilisation.
15/09/ 2012 (07.00)
Delivery wound pain
1 day post partum
Observed mother and baby well being Suggest mother to mobilisation, eat, and drink, medication.
You might also like
- Name: Mrs. N.S. Age: 20 Yo Address: Narmada Admitted: October, 29 2012 at 10.30 WitaDocument6 pagesName: Mrs. N.S. Age: 20 Yo Address: Narmada Admitted: October, 29 2012 at 10.30 WitaLaili KhairaniNo ratings yet
- MR OBGYN 14 Okt 2012 - KPD - SCDocument10 pagesMR OBGYN 14 Okt 2012 - KPD - SCPutra MahautamaNo ratings yet
- Morning Report: Supervisor: Dr. Rusdhy A.H., SP - OG Medical StudentsDocument8 pagesMorning Report: Supervisor: Dr. Rusdhy A.H., SP - OG Medical StudentsEra MoetzNo ratings yet
- MR 13agustus13 - KPD Preterm Drip MRDocument11 pagesMR 13agustus13 - KPD Preterm Drip MRIda Andalos TothaNo ratings yet
- Supervisor: Dr. Gede Made Punarbawa, SP - OG (K) Medical Students: TiaDocument10 pagesSupervisor: Dr. Gede Made Punarbawa, SP - OG (K) Medical Students: TiaRian Segal HidajatNo ratings yet
- Morning Report Obstetri 1Document7 pagesMorning Report Obstetri 1melatiigdNo ratings yet
- Morning Report Obstetri 12Document5 pagesMorning Report Obstetri 12melatiigdNo ratings yet
- KPD Drip Oxytocin-18.04.12Document6 pagesKPD Drip Oxytocin-18.04.12Vendi Cahyadi RiandikaNo ratings yet
- Supervised By: Dr. Punarbawa Spog: Morning ReportDocument19 pagesSupervised By: Dr. Punarbawa Spog: Morning ReportArja' WaasNo ratings yet
- MR Obgyn LMRDocument25 pagesMR Obgyn LMRRian Segal HidajatNo ratings yet
- 04-12-13 Letak Sugsang FinishDocument13 pages04-12-13 Letak Sugsang FinishAnonymous L3q7yHhhNo ratings yet
- Morning Report: Case Resume Normal Labor 2 Pathology LaborDocument10 pagesMorning Report: Case Resume Normal Labor 2 Pathology LabormelatiigdNo ratings yet
- Morning Report Obstetri 11Document6 pagesMorning Report Obstetri 11melatiigdNo ratings yet
- MR PEB Kl1 F Aktif Macet 26.4.12Document6 pagesMR PEB Kl1 F Aktif Macet 26.4.12Arrum Chyntia YuliyantiNo ratings yet
- Morning Report: Case Resume Normal Labor - Pathology LaborDocument9 pagesMorning Report: Case Resume Normal Labor - Pathology LabormelatiigdNo ratings yet
- Laporan Kasus PEB + Impending EklamsiaDocument9 pagesLaporan Kasus PEB + Impending EklamsiaPutra MahautamaNo ratings yet
- MR 4 Agustus 2014Document18 pagesMR 4 Agustus 2014Rian Segal HidajatNo ratings yet
- Preeklampsia BeratDocument5 pagesPreeklampsia BeratmelatiigdNo ratings yet
- MR 13Document6 pagesMR 13Vendi Cahyadi RiandikaNo ratings yet
- Kala II KasepDocument4 pagesKala II KasepSiska SiscaNo ratings yet
- Supervisor: Dr. Edy Prasetyo, Spog: Medical Student: Novi, Suwika, HeryDocument12 pagesSupervisor: Dr. Edy Prasetyo, Spog: Medical Student: Novi, Suwika, HeryAnonymous L3q7yHhhNo ratings yet
- Supervisor: Dr. Made Mahayasa, SP - OG Medical Students:: Morning ReportDocument6 pagesSupervisor: Dr. Made Mahayasa, SP - OG Medical Students:: Morning ReportNur LestaryNo ratings yet
- Morning Report August, 13 2015: Supervisor: Dr. Gede Made Punarbawa, SP - OG DM Jaga: Febri, RianDocument27 pagesMorning Report August, 13 2015: Supervisor: Dr. Gede Made Punarbawa, SP - OG DM Jaga: Febri, RianRian Segal HidajatNo ratings yet
- DM: Yoga, Ida, Brian, Fauzan, Ardian, Abrista, UlfaDocument21 pagesDM: Yoga, Ida, Brian, Fauzan, Ardian, Abrista, UlfaFaridatun HasanahNo ratings yet
- Morning Report 1 September 2014Document11 pagesMorning Report 1 September 2014Rian Segal HidajatNo ratings yet
- MR 29 Sept 2011Document10 pagesMR 29 Sept 2011Lili SurianiNo ratings yet
- KPD Minggu 9 LalaDocument7 pagesKPD Minggu 9 LalaArja' WaasNo ratings yet
- Name: Mrs. E Age: 26 Yo RM: 538866 Adress: Narmada Admitted: May, 18 2012 at 02.51 Name: Mrs. E Age: 26 Yo RM: 538866 Adress: Narmada Admitted: May, 18 2012 at 02.51Document5 pagesName: Mrs. E Age: 26 Yo RM: 538866 Adress: Narmada Admitted: May, 18 2012 at 02.51 Name: Mrs. E Age: 26 Yo RM: 538866 Adress: Narmada Admitted: May, 18 2012 at 02.51Akbar GazaliNo ratings yet
- Morning Report September, 4 2015: Supervisor: Dr. Made Putra Juliawan, Spog DM Jaga: RianDocument48 pagesMorning Report September, 4 2015: Supervisor: Dr. Made Putra Juliawan, Spog DM Jaga: RianRian Segal HidajatNo ratings yet
- SalmahDocument17 pagesSalmahRian Segal HidajatNo ratings yet
- Morning Report VK SCDocument8 pagesMorning Report VK SCmardilasariNo ratings yet
- Morning Report: Supervised By: Dr. Edi P.W. SpogDocument10 pagesMorning Report: Supervised By: Dr. Edi P.W. SpogArja' WaasNo ratings yet
- Morning Report 16-12-12 Drip SuccessDocument6 pagesMorning Report 16-12-12 Drip SuccessmelatiigdNo ratings yet
- Preeklampsia BeratDocument9 pagesPreeklampsia BeratmelatiigdNo ratings yet
- Morning Report 19-12-12 Prolonged Latent PhaseDocument6 pagesMorning Report 19-12-12 Prolonged Latent PhasemelatiigdNo ratings yet
- Fase Aktif Memanjang Drip & Kala II Lama VEDocument7 pagesFase Aktif Memanjang Drip & Kala II Lama VELaili KhairaniNo ratings yet
- MR 12 Sept 2011Document7 pagesMR 12 Sept 2011Lili SurianiNo ratings yet
- 27-10-09 PagiDocument3 pages27-10-09 PagiLaili KhairaniNo ratings yet
- Morning Report 31-8-14Document11 pagesMorning Report 31-8-14Rian Segal HidajatNo ratings yet
- Name: Mrs. S Age: 21 Years Old Address: Penimbun Admitted: January 7 2016 No. RM: 572290Document10 pagesName: Mrs. S Age: 21 Years Old Address: Penimbun Admitted: January 7 2016 No. RM: 572290Meita ReligiaNo ratings yet
- Supervisor: Dr. Edi Prasetyo W., SP - OG Medical Students:: Morning ReportDocument10 pagesSupervisor: Dr. Edi Prasetyo W., SP - OG Medical Students:: Morning ReportNetii FarhatiNo ratings yet
- First Stage Active Phase Neglected Pro SCDocument8 pagesFirst Stage Active Phase Neglected Pro SCAYu MiFtakhunNo ratings yet
- Case Report: IdentityDocument6 pagesCase Report: IdentityKelli RoseNo ratings yet
- Morning Report October 5 2011: Supervisor: Dr. Doddy, SpogDocument6 pagesMorning Report October 5 2011: Supervisor: Dr. Doddy, SpogLili SurianiNo ratings yet
- Duty Report "Example"Document9 pagesDuty Report "Example"Riyan W. PratamaNo ratings yet
- Supervisor: Dr. Agus Thoriq, Spog DM: AkbarDocument31 pagesSupervisor: Dr. Agus Thoriq, Spog DM: AkbarAkbar GazaliNo ratings yet
- Mr2 KPDP 28 May 2012Document6 pagesMr2 KPDP 28 May 2012Heri Hrisikesa WjgNo ratings yet
- Morning Report July, 21 2014: Supervisor: Dr. I Made Putra Juliawan, SP - OG DM Jaga: Zia, Yid, Santi, AyuDocument10 pagesMorning Report July, 21 2014: Supervisor: Dr. I Made Putra Juliawan, SP - OG DM Jaga: Zia, Yid, Santi, AyuRian Segal HidajatNo ratings yet
- MR 25-10-2015 DR - SNO, SP - OG-KDocument57 pagesMR 25-10-2015 DR - SNO, SP - OG-KStephanie Amelia ArgodipuroNo ratings yet
- 8 NOVEMBER 2009: Morning ReportDocument10 pages8 NOVEMBER 2009: Morning ReportArja' WaasNo ratings yet
- 11-10-12 LetliDocument5 pages11-10-12 LetliArja' WaasNo ratings yet
- Morning Report 9Document9 pagesMorning Report 9melatiigdNo ratings yet
- MR Lili Stengah Gemeli Belum JadiDocument5 pagesMR Lili Stengah Gemeli Belum JadiLili SurianiNo ratings yet
- Morning Report: Supervisor: Dr. H. Doddy Ak., Spog (K)Document10 pagesMorning Report: Supervisor: Dr. H. Doddy Ak., Spog (K)vika handayaniNo ratings yet
- Morning Report: Case Resume Normal Labor 0 Pathologies LaborDocument5 pagesMorning Report: Case Resume Normal Labor 0 Pathologies LabormelatiigdNo ratings yet
- HPPDocument15 pagesHPPArizkamhNo ratings yet
- CPD + MakrosomiaDocument6 pagesCPD + MakrosomiaLili SurianiNo ratings yet
- DMG + Macrosomnia + APBDocument9 pagesDMG + Macrosomnia + APBArja' WaasNo ratings yet
- 01 DESEMBER 2008: Morning ReportDocument20 pages01 DESEMBER 2008: Morning ReportNetii FarhatiNo ratings yet
- North Carolina Children’s Global Health Handbook: A Pediatrician’s Guide to Integrating IMCI Guidelines in Sub-Saharan AfricaFrom EverandNorth Carolina Children’s Global Health Handbook: A Pediatrician’s Guide to Integrating IMCI Guidelines in Sub-Saharan AfricaErica C. BjornstadNo ratings yet
- Stok Obat-1Document17 pagesStok Obat-1Putra MahautamaNo ratings yet
- Tumor OvariumDocument20 pagesTumor OvariumPutra MahautamaNo ratings yet
- Tumor OvariumDocument20 pagesTumor OvariumPutra MahautamaNo ratings yet
- Tumor OvariumDocument20 pagesTumor OvariumPutra MahautamaNo ratings yet
- Physiology of PregnancyDocument31 pagesPhysiology of PregnancyPutra Mahautama100% (1)
- DistosiaDocument185 pagesDistosiaPutra MahautamaNo ratings yet
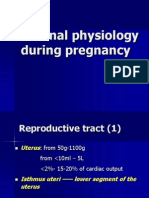
- Maternal Physiology During PregnancyDocument28 pagesMaternal Physiology During PregnancyPutra MahautamaNo ratings yet
- Fistula AbdominalisDocument19 pagesFistula AbdominalisPutra MahautamaNo ratings yet
- Lapsus 1 - Suspect Tumor BuliDocument8 pagesLapsus 1 - Suspect Tumor BuliPutra MahautamaNo ratings yet
- Lapsus 1 - Suspect Tumor BuliDocument8 pagesLapsus 1 - Suspect Tumor BuliPutra MahautamaNo ratings yet
- Lapsus 2 - Wilms TumorDocument9 pagesLapsus 2 - Wilms TumorPutra MahautamaNo ratings yet
- Pediatrics - unm.edu/divisions/neonatology/docs/MAS - PDF: Ctice/co379.pdf?dmc 1&ts 20130416T1813583992Document1 pagePediatrics - unm.edu/divisions/neonatology/docs/MAS - PDF: Ctice/co379.pdf?dmc 1&ts 20130416T1813583992Putra MahautamaNo ratings yet
- Laporan Kasus KJDRDocument7 pagesLaporan Kasus KJDRPutra MahautamaNo ratings yet
- MR OBGYN 14 Okt 2012 - Fase Aktif Kasep - SCDocument6 pagesMR OBGYN 14 Okt 2012 - Fase Aktif Kasep - SCPutra MahautamaNo ratings yet
- Laporan Kasus PEB + Impending EklamsiaDocument9 pagesLaporan Kasus PEB + Impending EklamsiaPutra MahautamaNo ratings yet
- Kuwait Pediatric GuideLinesDocument124 pagesKuwait Pediatric GuideLinesemicurudimov100% (1)
- Muscles of Mastication Saurav 2Document79 pagesMuscles of Mastication Saurav 2FourthMolar.comNo ratings yet
- Class IX - Worksheet 4 (Comprehension & Writing Skill)Document6 pagesClass IX - Worksheet 4 (Comprehension & Writing Skill)Anis FathimaNo ratings yet
- Lesson 5 Core Elements Evidenced Based Gerontological Nursing PracticeDocument38 pagesLesson 5 Core Elements Evidenced Based Gerontological Nursing PracticeSam GarciaNo ratings yet
- Escala de Apatia de StarksteinDocument6 pagesEscala de Apatia de StarksteinVanessa HernandezNo ratings yet
- Cardiology - Corrected AhmedDocument23 pagesCardiology - Corrected AhmedHanadi UmhanayNo ratings yet
- Annex I Summary of Product CharacteristicsDocument29 pagesAnnex I Summary of Product CharacteristicslisnerisNo ratings yet
- Oet Test Material: Occupational English Test Reading Sub-Test NursingDocument13 pagesOet Test Material: Occupational English Test Reading Sub-Test NursingRyu Tse33% (3)
- QB BT PDFDocument505 pagesQB BT PDFنيزو اسوNo ratings yet
- LAN Party Skate Park by Shane Jesse ChristmassDocument91 pagesLAN Party Skate Park by Shane Jesse ChristmassPatrick TrottiNo ratings yet
- Coping With CrossdressingDocument43 pagesCoping With Crossdressingjodiebritt100% (5)
- Tumor Marker Tests - CancerDocument4 pagesTumor Marker Tests - CancerMonna Medani LysabellaNo ratings yet
- GMO Pro Arguments (Gen-WPS OfficeDocument4 pagesGMO Pro Arguments (Gen-WPS OfficeFranchesca RevelloNo ratings yet
- Human Body Systems: Study GuideDocument11 pagesHuman Body Systems: Study Guideapi-242114183No ratings yet
- FlaxDocument9 pagesFlaxXeeshan Rafique MirzaNo ratings yet
- LP MAPEH 9 (Health)Document4 pagesLP MAPEH 9 (Health)Delima Ninian100% (2)
- Cage HomesDocument8 pagesCage HomesstanhopekrisNo ratings yet
- How Swab Testing of Kitchen SurfacesDocument3 pagesHow Swab Testing of Kitchen SurfacesSIGMA TESTNo ratings yet
- Is It True That GanodermaDocument2 pagesIs It True That GanodermaRohit SharmaNo ratings yet
- Program Implementation With The Health Team: Packages of Essential Services For Primary HealthcareDocument1 pageProgram Implementation With The Health Team: Packages of Essential Services For Primary Healthcare2A - Nicole Marrie HonradoNo ratings yet
- Preterm Prelabour Rupture of MembranesDocument12 pagesPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanNo ratings yet
- Adr Enaline (Epinephrine) 1mg/ml (1:1000) : Paediatric Cardiac Arrest AlgorhytmDocument13 pagesAdr Enaline (Epinephrine) 1mg/ml (1:1000) : Paediatric Cardiac Arrest AlgorhytmwawaNo ratings yet
- Electronic Physician (ISSN: 200 08-5842)Document10 pagesElectronic Physician (ISSN: 200 08-5842)Sapi KemploNo ratings yet
- The Nadi Vigyan by DR - Sharda Mishra MD (Proff. in Jabalpur Ayurved College)Document5 pagesThe Nadi Vigyan by DR - Sharda Mishra MD (Proff. in Jabalpur Ayurved College)Vivek PandeyNo ratings yet
- Long-Term Survey of Tooth Loss in 600 PtsDocument15 pagesLong-Term Survey of Tooth Loss in 600 PtsAndy HeNo ratings yet
- RUNDOWN ILMIAH TIPD 2021 29 SeptDocument8 pagesRUNDOWN ILMIAH TIPD 2021 29 SeptJessie AriniNo ratings yet
- Medical FlyerDocument2 pagesMedical FlyerThana PalNo ratings yet
- Delayed Homicides and The Proximate Cause.8Document5 pagesDelayed Homicides and The Proximate Cause.8rheanditahafsaNo ratings yet
- Measurement of CENTRAL VENOUS PRESSURE Via A TransducerDocument22 pagesMeasurement of CENTRAL VENOUS PRESSURE Via A TransducerJasleen KaurNo ratings yet
- Subjective: Diarrhea Related To Watery Short Term: IndependentDocument4 pagesSubjective: Diarrhea Related To Watery Short Term: IndependentEmma Lyn SantosNo ratings yet