Professional Documents
Culture Documents
Antipsychotics
Uploaded by
Jandz MNCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antipsychotics
Uploaded by
Jandz MNCopyright:
Available Formats
Antipsychotics
Typical/ First Generation/ Novel Antipsychotics *(Side Effects, Adverse Reactions, Special Precautions & Nursing Responsibilities)
I.
Side Effects & Adverse Reactions
A. Extrapyramidal Symptoms (EPS) o Serious Neurologic symptoms which are the major side effects of antipsychotics. Due to the blockage of D2 receptors in the midbrain.
a. Manifestations: i. Acute Dystonia
ii. Pseudoparkinsonism iii. Akathisia
i.
Dystonia o Acute muscular rigidity and cramping, stiff or thick tongue with difficulty in swallowing and laryngospasm and respiratory difficulties.
a.
Symptoms:
Muscular rigidity and cramping Stiff or thick tongue with difficulty in swallowing
In severe cases: Laryngospasm Respiratory difficulty
b.
Risk factors: i. ii. iii. First week of treatment Younger than 40 years old Males
iv. Receiving high potency drugs: Haloperidol, Thiothixene
ii.
Pseudoparkinsonism o o Drug- induced parkinsonism Symptoms similar to Parkinsons disease
a. Symptoms stiff- stooped posture mask- like facies decreased am swing shuffling, festinating gait cogwheel rigidity iii. Akathisia o Reported by the client as an intense need to move about.
drooling tremor bradycardia
pill- rolling movement of fingers at rest
a. Symptoms: restlessness anxiety b. Management o o Decreasing dosage of antipsychotic medication Changing of antipsychotic medication agitation rigid posture & gait
o Adding oral anticholinergic medication (amantadine) to treatment o Administering a beta-blocker or benzodiazepine
B. Neuroleptic Malignant Syndrome (NMS) o Potentially fatal idiosyncratic reaction to an antipsychotic medication (neuroleptic).
a. Symptoms: rigidity high fever confusion & delirium elevated CPK levels changing LOC
autonomic instability
i. unstable blood pressure ii. pallor iii. Diaphoresis
b. Risk factors: i. ii. First 2 weeks of treatment Dehydration
iii. Poor nutrition iv. Concurrent medical condition
c. Management & Treatment o o Immediate discontinuation of all antipsychotic medications Supportive treatment for dehydration and hyperthermia
Note: After NMS, the decision to treat the client with other antipsychotic drug requires full discussion between the client/folk and the physician to weigh the relative risks against the potential benefits of therapy.
C. Tardive Dyskinesia (TD) o o o o Syndrome of permanent involuntary movement. Pathophysiology remains unclear. No effective treatment for general use. Antipsychotic medication can mask beginning symptoms
a. Symptoms: Involuntary movement of: i. tongue ii. facial muscles iii. neck muscles iv. uper & lower extremities
v. truncal musculature
tongue thrusting & protruding lip smacking blinking grimacing
excessive unescessary facial movement b. Management o o After it has developed, TD is irreversible Decreasing or discontinuing antipsychotic medication can arrest progression
o o o o
Prevention is the best mode of action Keeping maintenance medications at lowest level possible dose Changing antipsychotic medications Periodic monitoring of patient
D. Anticholinergic Side Effects o o Often occur with the use of antipsychotics Taking anticholinergic medications for EPS may cause increased problems
a. Symptoms: orthostatic hypotension dry mouth constipation urinary hesitancy or retention
blurred vision dry eyes photophobia nasal congestion decreased memory
b. Management o o Supportive treatment for presenting symptoms Use of calorie- free beverages or hard candy to alleviate dry mouth Inclusion fruits and grains in the diet prevents constipation
E. Other side effects i. Elevated Prolactin levels a. Symptoms: breast enlargement & tenderness diminished libido erectile & orgasmic dysfnction menstrual irregularities increased risk for breast cancer contributes to weight gains
ii. Cardiovascular Irregularities a. Symptoms: postural hypotension palpitation tachycardia lengthened QT interval dysrhythmia
Client Teaching Inform the client and folk to watch out the possible side effects of the antipsychotic medication being taken and prompt referral to the physician/psychiatrist. Teach client and folks of managing or avoiding unpleasant side effects or adverse reactions and maintaining the medication regimen. Teach patient and folks to monitor patients sleepiness and drowsiness and to limit or avoid physical activities if level of consciousness is decreased. Teach the patient and folk that if medication is missed, he or she can take the missed dose if it is only 3-4 hours late. If the dose is more than 4 hours overdue or the next dose is due, the client may omit the forgotten dose. Encourage compliance to medication by utilizing charts or pillboxes which can be prefilled with accurate doses for the day of the week.
JMNbsnIIIc
You might also like
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- lIVER AbscessDocument2 pageslIVER AbscessJandz MNNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- ACCN Assignment #2Document9 pagesACCN Assignment #2Jandz MNNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- ACCN Assignment #2Document9 pagesACCN Assignment #2Jandz MNNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- ACCN Assignment #2Document9 pagesACCN Assignment #2Jandz MNNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- 24 Hour Fluid MonitoringDocument2 pages24 Hour Fluid MonitoringJandz MNNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Textbook DiscussionDocument3 pagesTextbook DiscussionJandz MNNo ratings yet
- Heart DevelopmentDocument24 pagesHeart DevelopmentJandz MNNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Patient Assignment-1Document1 pagePatient Assignment-1Jandz MNNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Tof Schematic DiagramDocument3 pagesTof Schematic DiagramJandz MNNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Metronidazole generic dosage indications reactionsDocument1 pageMetronidazole generic dosage indications reactionsiluvmunicamuchNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Evaluation Sheet: Registration Process (Generally)Document1 pageEvaluation Sheet: Registration Process (Generally)Jandz MNNo ratings yet
- P Francis. Ign Feastday. For PrintDocument6 pagesP Francis. Ign Feastday. For PrintJandz MNNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Self Assessment Tool NAMSSDocument5 pagesSelf Assessment Tool NAMSSJandz MNNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Gastroenteritis GuidelineDocument15 pagesGastroenteritis GuidelineJandz MNNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Cover PageDocument1 pageCover PageJandz MNNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- ReferencesDocument5 pagesReferencesJandz MNNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Table of ContentsDocument1 pageTable of ContentsJandz MNNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- World CivilizationDocument15 pagesWorld CivilizationJandz MNNo ratings yet
- ICU Case Pre - Labs DRFTDocument9 pagesICU Case Pre - Labs DRFTJandz MNNo ratings yet
- Schem DiDocument3 pagesSchem DiJandz MNNo ratings yet
- Evaluation Sheet: Registration Process (Generally)Document1 pageEvaluation Sheet: Registration Process (Generally)Jandz MNNo ratings yet
- Results Normal Values Significance Blood Gas Values Hco Tco Bevv O Sat Temporary Corrected Values Ph-Paco PaoDocument1 pageResults Normal Values Significance Blood Gas Values Hco Tco Bevv O Sat Temporary Corrected Values Ph-Paco PaoJandz MNNo ratings yet
- Management of Acute Asthma in Adults in The EmergencyDocument14 pagesManagement of Acute Asthma in Adults in The EmergencyJandz MNNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- ICU Case Pre - Labs DRFTDocument9 pagesICU Case Pre - Labs DRFTJandz MNNo ratings yet
- Schematic Diagram MyomaDocument2 pagesSchematic Diagram MyomaJandz MN100% (2)
- Sports BeatDocument34 pagesSports BeatJandz MNNo ratings yet
- Schematic Diagram Intramural MyomaDocument3 pagesSchematic Diagram Intramural MyomaJandz MNNo ratings yet
- Monopolistic CompetitionDocument29 pagesMonopolistic CompetitionJandz MNNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- TOF Schem DiDocument3 pagesTOF Schem DiJandz MNNo ratings yet
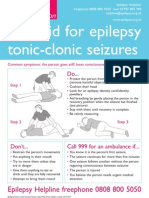
- Epilepsyaction FirstaidpostersDocument2 pagesEpilepsyaction FirstaidpostersKheliwiNo ratings yet
- Clinical Neurosurgical Vignettes For The Oral Board and Recertification Examinations First 2 Chapters PDFDocument27 pagesClinical Neurosurgical Vignettes For The Oral Board and Recertification Examinations First 2 Chapters PDFece142100% (2)
- Anatomy and Physiology of Blood VesselDocument3 pagesAnatomy and Physiology of Blood Vesselneleh grayNo ratings yet
- Neurology Notes Syrian StudentDocument5 pagesNeurology Notes Syrian StudentLiridon SopajNo ratings yet
- Tigrinya Medical LSKDocument120 pagesTigrinya Medical LSKTesfa Wele100% (1)
- Neurological AssessmentDocument64 pagesNeurological AssessmentNEuRoLoGisT CoFFeeCuP95% (20)
- Unti 4-6 StudyDocument1 pageUnti 4-6 StudyJennifer Schulze AyscueNo ratings yet
- Chiari MalformationDocument15 pagesChiari Malformationapi-388981686No ratings yet
- Doh - Mental Health Gap Action ProgramDocument4 pagesDoh - Mental Health Gap Action ProgramCassey AnneNo ratings yet
- Final Case Study JindalDocument39 pagesFinal Case Study JindalSahil SinglaNo ratings yet
- Manual de Neuropatía Periférica (2005)Document727 pagesManual de Neuropatía Periférica (2005)histoginoNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Neurotransmitter ChartDocument1 pageNeurotransmitter ChartEduardo LauandeNo ratings yet
- GCSDocument76 pagesGCSJane PalafoxNo ratings yet
- 4 5866212804146498341Document36 pages4 5866212804146498341Faris FirasNo ratings yet
- Clinical Aspects of UMN LMNDocument24 pagesClinical Aspects of UMN LMNKelly YeowNo ratings yet
- Nervous System Chapter EssentialsDocument19 pagesNervous System Chapter EssentialsAeren RhosenNo ratings yet
- Certificaiton of Rachel Alintoff - RevisedDocument11 pagesCertificaiton of Rachel Alintoff - Revisedmikekvolpe100% (1)
- Frequent Headaches: Evaluation and Management: Patients WithDocument10 pagesFrequent Headaches: Evaluation and Management: Patients WithRami ElnakatNo ratings yet
- Multiple SclerosisDocument96 pagesMultiple SclerosisDrGasnasNo ratings yet
- 1 - 2 - Module 1 (Neuroanatomy) - Part 1 - Learning Objectives and Overview of Neuroanatomy (27-46)Document14 pages1 - 2 - Module 1 (Neuroanatomy) - Part 1 - Learning Objectives and Overview of Neuroanatomy (27-46)Rodrigo Eberhart Musaio SommaNo ratings yet
- Sensing the environment: Sight 視覺Document3 pagesSensing the environment: Sight 視覺Winnie ChanNo ratings yet
- Convulsion Neo Flujograma 11 NicusDocument8 pagesConvulsion Neo Flujograma 11 NicusYolanda RodriguezNo ratings yet
- Audiogram InterpretationDocument5 pagesAudiogram InterpretationSusan JackmanNo ratings yet
- III. Mcqs NeuroDocument19 pagesIII. Mcqs NeuroMhmd Iraky100% (1)
- Cns PathologyDocument18 pagesCns Pathologysunnyorange8No ratings yet
- Multiple Sclerosis Concept MapDocument1 pageMultiple Sclerosis Concept MapKyle Santos50% (2)
- Non-Convulsive Status EpilepticusDocument17 pagesNon-Convulsive Status EpilepticusjossNo ratings yet
- Dissertationen Online Uni Bonn MedizinDocument8 pagesDissertationen Online Uni Bonn MedizinHelpWithWritingAPaperUK100% (1)
- PG Prospectus 2021Document41 pagesPG Prospectus 2021Amy LalringhluaniNo ratings yet
- Electroencephalography (Eeg)Document13 pagesElectroencephalography (Eeg)Shelten GeorgeNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)