Professional Documents
Culture Documents
Periodonsi
Uploaded by
AndykaYayanSetiawanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Periodonsi
Uploaded by
AndykaYayanSetiawanCopyright:
Available Formats
Dental Sciences
Chhokra Mehak et al. / JPBMS, 2012, 20 (19)
Available online at www.jpbms.info
Review article JPBMS
ISSN NO- 2230 7885 CODEN JPBSCT NLM Title: J Pharm Biomed Sci.
JOURNAL OF PHARMACEUTICAL AND BIOMEDICAL SCIENCES
Magic Bullet to treat Periodontitis: A targeted approach
Vidya Dodwad1, Shubra Vaish2, *Mehak Chhokra3, Aakriti Mahajan3.
1MDS,
Professor and HOD,2 MDS,Reader,3 MDS, final year students ,Department of Periodontology, ITS-CDSR, Ghaziabad, India.
Abstract:
Periodontitis is a disease attributable to multiple infectious agents and interconnected with cellular and humoral host responses. It results from extension of the inflammatory process initiated in the gingiva to the supporting periodontal tissues. Periodontal pockets provide natural reservoir bathed by gingival crevicular fluid that is easily accessible for the insertion of a delivery device. Controlled release delivery of antimicrobials is a therapeutic intervention directly into periodontal pockets and is available in various forms like gels, monolithic devices, irrigation systems, chips, films, strips, microspheres, fibres etc. It is an effective monotherapy that has evoked a great interest and appears to hold a sound promising result in periodontal treatment. It does not substitute the local instrumentation but acts as an adjunct to it. These local agents bypass the adverse effects of systemically administered antimicrobial agents, as well stabilize the attachment apparatus and reduce the probing depth thereby allowing better control and management of periodontal disease.
Keywords: Gingivitis, Periodontitis, Local drug delivery, Periodontal Pocket
Introduction:
Gingival and Periodontal disease is affecting the mankind since decades and in now looked upon as a principle health problem. Periodontitis is a complex multi factorial disease mainly caused due to gram negative microbes and host response to their colonization leading to destruction of periodontal apparatus. Henceforth, periodontal pocket acts as a source of continuous localized infection which acts as a niche of various potential periodontopathogens including Actinobacillus actinomycetemcomitans, Porphyromonas gingivalis, Prevotella intermedia, Bacteroides forsythus, Peptostreptococcus micros, Campylobacter rectus, Eikenella corrodens, Fusobacterium nucleatum, Eubacterium spp., Treponema denticola, Selenomonas spp., beta-hemolytic streptococci, a variety of enteric rods and pseudomonas, enterococci, staphylococci and possibly yeasts[1]. Elimination or adequate suppression of putative periodontopathic microorganisms in the subgingival microbiota is necessary for periodontal healing. The clinical improvement following conventional mechanical root debridement is directly related to the degree to which pathogenic subgingival microbial plaques are reduced or completely eradicated[2]. Poor oral hygiene leads to reestablishment of subgingival microflora within 2 months of single debridement session and 120-140 days despite of multiple sessions of subgingival and supragingival instrumentation [3,4]. This temporary effect of root planing and its inability to eradicate all periodontal pathogens can also be attributed to the unfavourable anatomy of tooth or dimension of periodontal pockets, which jeopardize the mechanical instrumentation, the incomplete removal of plaque and calculus, the existence of an intraoral microbial translocation and/or the escapement of the pathogens
1
during debridement into the adjacent the periodontal tissues [5,6]. The microbial aetiology of human periodontitis further suggests the treatment with antimicrobial agents.1 Various antimicrobial agents may gain access into deep periodontal pockets through systemic or local route of administration. Systemic agents come into action through their intestinal absorption, leading passage from bloodstream entering into oral tissues. On contrary, local administration involves direct delivery of agent into subgingival site, minimizing the adverse reactions on non oral sites.
Comparison of systemic and local administration of drug
Systemic administration of drug via oral or parenteral routes is done with higher concentration of drug to attain a particular plasma level prior to entering the gingival tissues. It leads to distribution of drug into various body compartments irrespective of the requirement, reaching widely distributed microorganisms better. This mode of drug delivery follows the first order kinetics therefore requires regular loading of dosage. Prime clinical limitations include systemic adverse effects, development of antibiotic resistance and patient compliance [7]. Whereas, locally delivered antimicrobial acts at a specific site with lower drug dosage, it intends to follow zero order kinetics. It has also been shown to penetrate and act better on biofilm associated bacteria [7]. Fewer number of side effects are observed with local administration due to its minimal distribution to different body compartments and with maximum concentration at delivered sites lowering the frequency of administration[8]. Problems associated can be re- infection from the treated sites and identification of type of lesion and pathogen.
Journal of Pharmaceutical and Biomedical Sciences (JPBMS), Vol. 20, Issue 20
Dental Sciences
Chhokra Mehak et al. / JPBMS, 2012, 20(19)
Systemic and local delivery of drugs can be used in conjunction with scaling and root planing and are effectively able to reduce the need for periodontal surgery [9]. However, the efficacy of locally applied antimicrobial agents in periodontitis therapy depends on obtaining adequate subgingival delivery of the agent, attaining sufficient contact time between the antimicrobial agent and the target microorganisms, and achieving effective concentrations of the antimicrobial agent [10].
Duration of action of the drug is dependent upon the mechanism by which the antimicrobial agent inhibits or destroys target bacteria, bacteriocidal or bacteriostatic pathway[17]. So an adequate drug-microbial contact time must be attained for an antimicrobial agent to act against targeted microorganisms. 4. Substantivity: Substantivity refers to property of a substance to bind to soft and/or hard tissue of the pocket, thereby establishing a drug reservoir[18]. Based on, an assumed pocket volume of 0.5ml and a gingival fluid flow rate of 20l /hr, it was estimated that half time of a non binding drug placed into a pocket is about a minute[19]. Therefore incorporation of drug into various vehicles or devices, prior to placement into periodontal pocket enhances substantivity.
Ideal requisites of Locally Delivery System[ 10, 11, 12]
Device must deliver drug to the base of the pocket. Must deliver drug at microbiologically efficacious concentration. 3. Must sustain the concentration of drug in the pocket for sufficient length of time and in sufficient concentration to be clinically effective. 4. Ease of placement. 5. Retention after placement. 6. Biodegradable. 7. No emergence of bacterial resistance. 8. Safe with minimal side effects. 9. Should be effective only against periodontal pathogens and not on commensal microflora. Before recommending any antimicrobial agent for periodontal therapy a number of basic requirements should be fulfilled [13]. 1. Drug must show in vitro activity against the organisms considered most important in the etiology. 2. It should be demonstrated that a dose sufficient to kill the target organism can be reached within the subgingival environment. 3. At that dose the drug should not have major local or systemic adverse effects. 4. Organisms should not be resistant to the antimicrobial agents. 5. Antibiotic should be specific for periodontal pathogens and not in general use for treatment of other diseases and should be inexpensive. 1. 2.
Indications of local drug delivery[8]
1. Isolated periodontal pockets (>5mm),with successful phase 1 therapy(scaling and root planing) Medically compromised patients where surgical therapy is contraindicated or not suggested As an adjunct to mechanical debridement In patients suffering from recurrent or refractory periodontitis As an adjunct to periodontal regenerative procedures Where periodontal surgery is to be avoided or the patient is on supportive periodontal treatment.
2. 3. 4. 5. 6.
Contraindications [8, 13]
Patients with known hypersensitivity reaction to any of the antimicrobials used as local drug, Delivery of antimicrobials using ultrasonic devices is contraindicated in asthamatics, infective conditions such as AIDS, tuberculosis and those with cardiac pacemakers.
Pharmacokinetic parameters criteria for local application [14, 17]
1. Site of action Local drug delivery targets bacteria in periodontal pocket, soft tissue wall of the pocket, exposed cementum or radicular dentin but presence of subgingival calculus impedes the delivery of these agents to intended sites of action. Reaching the entire periodontal pocket is also difficult because of its very small entrance (150 mm for a 4- mm deep pocket).[22] Thus local drug delivery should be done as an adjunct to SRP. Moreover, Anatomic anomalies, deep pockets and furcation lesions may also impart physical difficulty in placing drug at intended site, thereby further impeding the drug efficacy at site. 2. Adequate Concentration Biofilm experiments have indicated that the minimum inhibitory concentrations of antimicrobial agents are at least 50 times (or even 210,000 times) higher than for bacteria growing under planktonic conditions [15,16]. Ensuring the adequate drug concentration and enhancing its efficacy at local site of action. 3. Sufficient duration
2
Advantages [7, 10, 20]
Provides drug in an effective concentration that can be maintained there long enough for the desired effect to be accomplished without causing any side effect. It can attain upto 100 fold higher concentration of an antimicrobial agent in subgingival site compared with a systemic therapy. Broad spectrum antibiotics which cannot be employed systemically because of many sideeffects can be safely employed locally with minimum side effects. Superinfection and drug resistance are rare. It also reduces the risk of developing drug resistant microbial populations at non oral body sites. The potentials of daily drug placement into periodontal pockets as a part of home self care procedure can be performed by a compliant patient. This route may employ antimicrobial agents not suitable for systemic administration such as various broad spectrum antiseptics solutions. e.g. chlorhexidine.
Journal of Pharmaceutical and Biomedical Sciences (JPBMS), Vol. 20, Issue 20
Dental Sciences
Chhokra Mehak et al. / JPBMS, 2012, 20 (19)
It also reduces potential problems with patient compliance. Disadvantages [20 , 21] Inaccessible and deeper pocket areas, furcations cannot be completely dealt with antimicrobial agents. Time consuming and laborious, if many sites are involved. Nonsustained local delivery is limited by a only brief exposure of targeted microorganisms to applied antimicrobial agent. Connective tissue associated plaque and extrapocket oral surfaces dont get affected by local drug delivery which may be responsible for recurrence of disease in treated areas. Difficulty in placing therapeutic concentration of antimicrobial agent into deeper parts of periodontal pockets and furcations lesions. Personal application of antimicrobial agents by patients as a part of their home self-care procedure is frequently compromised by the patients lack of adequate manual dexterity, limited understanding of periodontal anatomy and poor compliance and performance with recommended procedures.
Sustained (or continuous) release of a drug involves polymers that release the drug at a controlled rate due to diffusion out of the polymer or by degradation of the polymer over time. Pulsatile release is often the preferred method of drug delivery, as it closely mimics the way by which the body naturally produces hormones such as insulin[25]. It is achieved by using the polymers that respond to specific environment or stimuli. Fibers: Fibers are thread like devices placed in periodontal pocket and secured with periodontal dressing, ensuring sustained release of drug at the site. Fibers used in periodontal disease are of two types hollow and monolithic fibers. Hollow fibers contains a reservoir of drug, which is released by simple diffusion through reservoir walls.26 Whereas , to decrease the speed of release of drug, monolithic fibers were developed by impregnating drug into the molten polymers, spinning it on high temperature followed by quick coolig [27]. Goodson studied the efficacy of both types of tetracycline fibers by placing them subgingivally to fill pockets to their probable depth and covered with a periodontal dressing which was maintained for 10 days. At these sites, total counts, spirochetes, motile rods and non motile rods were significantly reduced immediately following treatment. In comparison, scaling produced much smaller alterations of darkfield counts which were not statistically significant. The average intrasulcular tetracycline concentration measured at the end of the 10-day period was 643 mg/ml with initial concentration to be 650 mg/ml.He further stated that hollow fiber system was an imperfect local delivery device, delivering drug from the cut ends and was exhausted within 1 day. In contrast, the monolithic ethylene vinyl acetate device functioned as a true controlled delivery system over the period tested[28]. Several polymers such as poly(e-caprolactone) (PCL), polyurethane, polypropylene, cellulose acetate propionate and ethyl vinyl acetate (EVA), nordihydroguaiaretic acid (NDGA) have been used to manufacture the fibers. Films: Films are implantable devices with encapsulation of drug, in a manner that it is distributed throughout the polymer with control release occurring through diffusion, dissolution or erosion. The release action depends on type of polymer used to manufacture the chip. Ease of insertion with minimal pain, control on dosage, dimension and shape of the films makes it an ideal device to be used in periodontal pocket. Thickness of film should not exceed 400 m as well as have sufficient adhesiveness to ensure no interference in maintaining oral hygiene habits. Soskolne et al. examined the adjunctive use of Chlorhexidine chip for routine periodontal maintenance therapy over 2 years and found it to be clinically safe and effective treatment option for long term management of chronic periodontitis[29]. In an in vitro study by Perugini et al. the composite micro matricial films, made of three layers of polymers (chitosan/ PLGA /chitosan) , as compared to the monolayer films, represent a suitable dosage form to prolong ipriflavone release for 20 days[30] Jeffcoat et al showed significant change in probing depth and clinical attachment levels after the placement of a
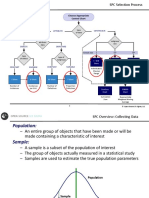
Classification of local delivery system
Based on type of therapy [10] A) Personally applied (patient home care) 1. Non Sustained (Oral irrigation) 2. Sustained (not developed till now) B) Professionally applied (in dental office) 1. Non Sustained (Supra and subgingival irrigation) 2. Sustained (Controlled release device) Based on degradability of the device [23] A) Biodegradable B) Non- Biodegradable Based on duration of action [18] A) Sustained released devices - These are delivery systems whose action lasts less than 24 hours therefore require multiple applications. It follows the first order kinetics. B) Controlled delivery devices These are the devices which follows zero order kinetics and whose actions last longer than 24 hours , thereby decreasing the number applications.
Various delivery devices
The mode by which a drug is delivered to a specific site of action has a significant role on its efficacy. The efficacy of drug delivery systems is mainly affected by the biological environment and the properties of the polymer and the drug[24]. A multidisciplinary approach to the delivery of therapeutics to target tissues is needed for precise control of pharmacokinetics and pharmacodynamics of the drug to ensure adequate concentration at the targeted site. Potential release mechanisms involved for controlled drug release can be: (i) desorption of surface-bound /adsorbed drugs; (ii) diffusion through the carrier matrix; (iii) diffusion (in the case of nanocapsules) through the carrier wall; (iv) carrier matrix erosion; and (v) a combined erosion /diffusion process[25]. The mode of delivery primarily controls drugs success and failure, as the choice of a drug is often influenced by the way it is administered.
3
Journal of Pharmaceutical and Biomedical Sciences (JPBMS), Vol. 20, Issue 20
Dental Sciences
Chhokra Mehak et al. / JPBMS, 2012, 20(19)
biodegradable chlorhexidine gelatin chip in the treatment of adult periodontitis[31]. Natural polymer like gelatine, chitosan, atelcollagen and synthetic polymers like polyvenyl alchol (PVA), poly (d,llactide-co-glycolide) (PLGA) are commonly used to synthesize films. Another biodegradable polymer poly (ortho esters) is still under trial to be used for local drug device. Gels: Gels are injectable semi solid devices containing adequate concentration of drug and delivered at specific site. They are easy to prepare and administer. They further possess a property of bioadhevisity that enhances the retention time in periodontal pocket. Salvi et al. demonstrated significant reduction in clinical and microbiological parameters after using elyzol ( metranidazole gel) and atridox (doxycycline gel)[32]. Abdaly further showed decrease in subgingival microbiological count after application of atridox (10% doxycycline gel)[33]. The gels composed of cellulose derivatives such as hydroxypropylmethyl cellulose and hydroxyethyl cellulose do not appear to have sustained release properties. Although various biogedradable polymers like xanthum gel, chitosan demonstrate better mucoadhesive property. The semisolid system based on water-free mixtures of lipids, such as glycerol monooleate (monoglyceride) and sesame oil (triglyceride) can also be used as they become semisolid on contact with gingival fluid in the periodontal pocket ensuring longevity of the drug. Microparticulate system: This system consists of encapsulation of drug into a polymer, which dissolves gradually releasing the drug at the target site. It is highly stable system for delivering a optimum concentration in the pocket. Nakahara et al demonstated regeneration of periodontal tissues in 4 weeks by using a sandwich membrane composed of a collagen sponge scaffold and gelatin microspheres containing basic fibroblast growth factor (bFGF) in situ.[35] Renvert et al. treated perimplantits patients with arestin (minocycline microspheres) with sustainance of improved results for 12 months.[36]. Biodegradable poly alpha hydroxy acids such as poly lactide (PLA) or poly (lactide co-glycolide) PLGA containing drug dosages can be used to treat periodontal disease. Nanoparticulate system: Nanosizing of drugs can lead to a dramatic increase in their absorption and subsequently bioavailability leading to a subsequent reduction in drug dose [34]. Owing to its small size, it acquires high dispersibility in an aqueous medium and controlled release rate. The polymer-based nanoparticles were prepared via micellar polymerisation, resulting in powder material with particle size in the range of 50180 nm[24]. This is the most stable system with reduced frequency of administration.
further trial for their administration as local drug into the periodontal pocket. Prudent administration of antimicrobial agents following judicious pharmacologic principles will preclude the abuse of chemotherapeutic agents and reduce the potential of developing or selecting drug resistant bacterial strains. Local drug delivery system with controlled release properties have the potential to be used as a therapeutic component in the management of periodontal diseases. It aims to minimize drug degradation and loss, prevent harmful side-effects and increase drug bioavailability and the fraction of the drug accumulated in the required zone. Various drug delivery and drug targeting systems are currently under development to obtain increased dissolution velocity, increased saturation solubility, improved bioadhesivity and versatility in surface modification so that better and effective administration of desired and newer drug can be done through the best possible system.
References
1. Slots J, Rams TE. Microbiology of periodontal disease. In: Slots J, Taubman MA, ed. Contemporary oral microbiology and immunology. St. Louis: CV Mosby Co., 1992:425-43. 2. Harper DS, Robinson PJ. Correlation of histometric, microbial, and clinical indicators of periodontal disease status before and after root planing. J Clin Periodontol 1987;14: 190-96. 3. Mousque`s T, Listgarten MA, Phillips RW. Effect of scaling and root planing on the composition of the human subgingival microbial flora. J Periodontal Res 1980; 15: 14451. 4. Magnusson I, Lindhe J, Yoneyama T, Liljenberg B. Recolonization of a subgingival microbiota following scaling in deep pockets. J Clin Periodontol 1984; 11: 193-207. 5. Rabbani GM, Ash MM Jr, Caffesse RG. The effectiveness of subgingival scaling and root planing in calculus removal. J Periodontol 1981; 52: 11923. 6. Waerhaug J. Healing of the dento-epithelial junction following subgingival plaque control. II. As observed on extracted teeth. J Periodontol 1978;49: 11934. 7. Lindhe J, Karring T, Lang NP. Clinical periodontology and Implant dentistry.4th edi.Blackwell Munksgaard Oxford: 479-81. 8. Dentino A. Overview of locally delivered controlled release antimicrobials: Adjuncts to periodontal therapy. Practical hygiene 1998;4:55-61. 9. Loesche W, Giordano J, Soehren S, Hutchinson R, Rau CF, et al.Nonsurgical treatment of patients with periodontal disease. Oral Surg Oral Med Oral Pathol 1996;81: 533 -43. 10. Slots J, Rams TE. Local delivery of antimicrobial agents in the periodontal pocket. Periodontol 2000 1996; Vol. 10: 139-59. 11. Goodson JM, Hogan PE, Dunham SL. Clinical responses following periodontal treatment by local drug delivery. J Periodontol; 1985 Special Issue: 81 - 87. 12. Greenstein G. The Role of Local Drug Delivery in the Management of Periodontal Diseases: A Comprehensive Review. J Periodontol 1998; 69: 507-20. 13. Manas D, Sirinivas SR, Jithendra KD. Role of antibiotics in periodontal therapy. Bang J med science 2009;8(4):91-101.
Conclusion
There are several drugs such as metronidazole, tetracycline, doxycycline, azithromycin, minocycline ,chlorhexidine as well as herbal products like neem, pomegranate, propolis that are used and are also under
4
Journal of Pharmaceutical and Biomedical Sciences (JPBMS), Vol. 20, Issue 20
Dental Sciences
Chhokra Mehak et al. / JPBMS, 2012, 20 (19)
14. American Academy of Periodontology Statement on Local Delivery of Sustained or Controlled Release Antimicrobials as Adjunctive Therapy in the Treatment of Periodontitis. J Periodontol 2006;77(8):1458-58. 15. Brown M, Gilbert P. Sensitivity of biofilms to antimicrobial agents. J Appl Bacteriol 1993: 74: 87S 97S. 16. Cargill KL, Pyle BH, Sauer RL, McFeters GA. Effects of culture conditions and biofilm formation on the iodine susceptibility of Legionella pneumophila. Can J Microbiol 1992: 38: 42329. 17. Quirynen M, Teughels W, Soete MD,Steenberghe DV. Topical antiseptics and antibiotics in the initial therapy of chronic adult periodontitis: microbiological aspects. Periodontol 2000 2002; Vol. 28: 7290 18. Greenstein G,Tonetti M.Academy report: The role of controlled drug delivery for periodontitis(Position paper).J Periodontol 2000;71:125-40. 19. Goodson J. Pharmacokinetic principles controlling efficacy of oral therapy. J Dent Res 1989;68: 1625- 32. 20. Chadha VS, Arora K, Manjunath B C, Kalra S. Local drug delivery in periodontics: current concepts and trends. Int J Adv Res Ora Sci 2012;1:1: 1 -9. 21. Axelsson P. Preventive materials, methods and programs. 4th Ed.Germany: Quintessence pub; 1999 22. Tanner AC, Goodson JM. Sampling of microorganisms associated with periodontal disease. Oral Microbiol Immunol 1986: 1: 1522. 23. Soskolone WA, Friedman M. Intra-periodontal pocket drug delivery systems. Ed by Michael J Rathbone., In: Oral mucosal drug delivery 2004; 74, Marcel Dekker Inc; 359- 79. 24. Bruschi ML, de Freitas O. Oral Bioadhesive Drug Delivery Systems. Drug Dev Ind Pharm. 2005 Mar;31(3):293-310. 25. Kaparissides C, Alexandridou S, Kotti K, Chaitidou S. Recent Advances in Novel Drug Delivery Systems. AZoJono [serial on the internet]. 2006 Mar 2005; [cited 2007 June 15]. Available from: http://www.azonano.com/Details.asp?ArticleID=1538. 26. Pragati S, Ashok S, Kuldeep S. Recent advances in periodontal drug delivery systems. Int J Drug Del 2009; 1: 1-14. Corresponding Author:Dr. Mehak Chhokra Department of Periodontology ITS-CDSR,Ghaziabad, India. Contact no:- +91-9811655332.
27. Goodson JM et al. Monolithic tetracycline-containing fibres for controlled delivery to periodontal pockets. J Periodontol 1983;54: 57579. 28. Goodson JM, Offenbacher S, Farr DH, Hogan PE. Periodontal Disease Treatment by Local Drug Delivery. J Periodontol 1985;56; 5:265-27. 29. Soskolne WA,Proskin HM,Stabholz A. Probing depth changes following 2 years of periodontal maintenance therapy including adjunctive controlled-release of chlorhexidine. J Periodontol 2003;74: 420-7. 30. Perugini P, Genta I, Conti B, Modena T, Pavanett F. Periodontal delivery of ipriflavone: new chitosan/PLGA film delivery system for a lipophilic drug. Int J Pharm 2003;(12); 1-9 . 31. Jeffcoat MK, Palcanis KG, Weatherford TW, Reese M, Geurs NC, Flashner M. Use of a biodgredable chlorhexidine chip in the treatment of adult periodontitis. Clinical and radiographic findings. J Periodontol 2000: 71: 256-62. 32. Salvi GE, Mombelli A, Local antimicrobial therapy after initial periodontal treatment. J Clin Periodontol 2002: 29: 540-550. 33. Abdaly MA, Refai AN, Gouda UM, Atty HA.Local Delivery of Atridox (Doxycycline gel) as Adjunctive in Management of Chronic Periodontitis. Suez Canal Univ Med J 2008; 11(I) :41-6. 34. Patravale VB, Date AA, Kulkarni RM. Nanosuspensions: a promising drug delivery strategy. J pharma and pharmacology 2004: 56: 82740. 35. Nakahara T, Nakamura T, Kobayashi E, Inoue M, Shigeno K,et.al. Novel Approach to Regeneration of Periodontal Tissues Based on in Situ Tissue Engineering: Effects of Controlled Release of Basic Fibroblast Growth Factor from a Sandwich Membrane. Tissue Engineering 2003; 9(1): 153-62. 36. Renvert S, Lessem J, Dahle NG, Lindahl C, Svensson M. Topical minocycline microspheres versus topical chlorhexidine gel as an adjunct to mechanical debridement of incipient periimplant infections: a randomized clinical trial. J Clin Periodontol 2006; 33: 36269.
Quick Response code (QR-Code) for mobile user to access JPBMS website electronically. Website link:- www.jpbms.info
Journal of Pharmaceutical and Biomedical Sciences (JPBMS), Vol. 20, Issue 20
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Spontaneous Harmonization EffectsDocument20 pagesSpontaneous Harmonization EffectsMaría Victoria100% (1)
- Bond Pricing and Bond Yield New - 1Document66 pagesBond Pricing and Bond Yield New - 1Sarang Gupta100% (1)
- Bonded Composites Versus Ceramic Veneers PDFDocument7 pagesBonded Composites Versus Ceramic Veneers PDFAndykaYayanSetiawanNo ratings yet
- The Bangladesh Liberation War, The Sheikh Mujib Regime, and Contemporary ControversiesDocument214 pagesThe Bangladesh Liberation War, The Sheikh Mujib Regime, and Contemporary Controversieshadiuzzaman sajeebNo ratings yet
- Debate-Script 1Document3 pagesDebate-Script 1api-537254339No ratings yet
- Full Denture ProstheticDocument6 pagesFull Denture ProstheticAndykaYayanSetiawanNo ratings yet
- Oral N Maxilofacial Surgery PDFDocument9 pagesOral N Maxilofacial Surgery PDFAndykaYayanSetiawanNo ratings yet
- Inside Outside Bleaching Technique - Poyser NJ, Kelleher MGD PDFDocument8 pagesInside Outside Bleaching Technique - Poyser NJ, Kelleher MGD PDFAndykaYayanSetiawanNo ratings yet
- Paul M.C. (Ed.) - Fiber Laser PDFDocument415 pagesPaul M.C. (Ed.) - Fiber Laser PDFXuan Phuong Huynh100% (1)
- Analisis Insiden Menggunakan RCADocument34 pagesAnalisis Insiden Menggunakan RCAAndykaYayanSetiawanNo ratings yet
- Putty TeknikDocument1 pagePutty TeknikAndykaYayanSetiawanNo ratings yet
- Clinical Sheet Oral and Maxillofacial Surgery: Azienda Ospedaliera Universitaria IntegrataDocument2 pagesClinical Sheet Oral and Maxillofacial Surgery: Azienda Ospedaliera Universitaria IntegrataAndykaYayanSetiawanNo ratings yet
- Veneer Classification .PDGDocument10 pagesVeneer Classification .PDGAndykaYayanSetiawanNo ratings yet
- Veneer Classification .PDGDocument10 pagesVeneer Classification .PDGAndykaYayanSetiawanNo ratings yet
- Midline Diastema Closure With Partial Laminate Veneers: A Case ReportDocument4 pagesMidline Diastema Closure With Partial Laminate Veneers: A Case ReportAndykaYayanSetiawanNo ratings yet
- April Mayart 1Document4 pagesApril Mayart 1AndykaYayanSetiawanNo ratings yet
- Thesis of Marwa ElsharkasiDocument70 pagesThesis of Marwa ElsharkasiAndykaYayanSetiawanNo ratings yet
- Tooth Whitening: Efficacy, Effects and Biological SafetyDocument6 pagesTooth Whitening: Efficacy, Effects and Biological SafetyAndykaYayanSetiawanNo ratings yet
- Pharmacotherapy of StrokeDocument37 pagesPharmacotherapy of StrokeAndykaYayanSetiawanNo ratings yet
- University of Caloocan City: (Week 12)Document8 pagesUniversity of Caloocan City: (Week 12)Gilyn NaputoNo ratings yet
- Pizza Experts (Furqan Project)Document17 pagesPizza Experts (Furqan Project)Umer MalikNo ratings yet
- Fullsummary PDFDocument118 pagesFullsummary PDFEsa SulyNo ratings yet
- Chapter One: An To The Nature of ManagementDocument32 pagesChapter One: An To The Nature of ManagementHaymanot endaleNo ratings yet
- Project Name: Management Functions of BisconniDocument6 pagesProject Name: Management Functions of BisconniUsman RaoNo ratings yet
- A Himalayan Challenge PDFDocument39 pagesA Himalayan Challenge PDFAdheesh TelangNo ratings yet
- 52594bos42131 Inter Corporate LawsDocument12 pages52594bos42131 Inter Corporate LawsHapi PrinceNo ratings yet
- Control - Statistical Process Control SPCDocument22 pagesControl - Statistical Process Control SPCHalimNo ratings yet
- Triple Screw PumpsDocument2 pagesTriple Screw PumpsSaravanan SelvaNo ratings yet
- Autodesk 2015 Products Direct Download LinksDocument2 pagesAutodesk 2015 Products Direct Download LinksALEXNo ratings yet
- BSP M-2022-024 s2022 - Rural Bank Strengthening Program) PDFDocument5 pagesBSP M-2022-024 s2022 - Rural Bank Strengthening Program) PDFVictor GalangNo ratings yet
- Patient Experience Measurement: Presented by Anum HashmiDocument16 pagesPatient Experience Measurement: Presented by Anum HashmiAnumNo ratings yet
- Facebook Addiction Chapter1Document22 pagesFacebook Addiction Chapter1Catherine BenbanNo ratings yet
- AgrrrraaDocument31 pagesAgrrrraaAnonymous apYVFHnCYNo ratings yet
- What Makes An Event A Mega Event DefinitDocument18 pagesWhat Makes An Event A Mega Event DefinitMoosaNo ratings yet
- Agribusiness GlosaryDocument6 pagesAgribusiness GlosaryJosé RamirezNo ratings yet
- 2020 Media Strategy Report: Insights From The WARC Media AwardsDocument53 pages2020 Media Strategy Report: Insights From The WARC Media AwardsShachin ShibiNo ratings yet
- Nelson Labs Valve Leak Test 1112597-S01 PDFDocument2 pagesNelson Labs Valve Leak Test 1112597-S01 PDFFaiq FuatNo ratings yet
- Inner Mongolia ProspectusDocument300 pagesInner Mongolia ProspectusSean GrayNo ratings yet
- Energies 10 02018 PDFDocument20 pagesEnergies 10 02018 PDFيوليسيس أوريروNo ratings yet
- Principles of ManagementDocument8 pagesPrinciples of Managementwriter bestNo ratings yet
- AFSCN Architecture EvolutionDocument7 pagesAFSCN Architecture Evolutionbaixiu0813No ratings yet
- The Trends in GlobalizationDocument2 pagesThe Trends in GlobalizationBielan Fabian GrayNo ratings yet
- Master Formula New UpdateDocument5 pagesMaster Formula New UpdateAdhoNo ratings yet
- Pumper March 2011 IssueDocument108 pagesPumper March 2011 IssuePumper MagazineNo ratings yet