Professional Documents
Culture Documents
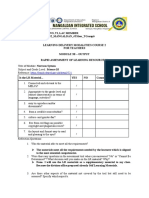
Diagnostic Test
Uploaded by
Mae UsquisaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diagnostic Test
Uploaded by
Mae UsquisaCopyright:
Available Formats
PERCEPTION AND COORDINATION Sensory perception- involves the conscious organization and translation of the data or stimuli into
meaningful information Sensory reception- process of receiving stimuli or data Kinesthetics- awareness of the position and movement of body parts Stereognosis- ability to perceive and understand an object through its size, shape and texture Visceral - any large organ within the body Four aspects of sensory process Stimulus an agent or act that stimulates a nerve receptor Receptor- a nerve cell that concerts stimulus to a nerve impulse Impulse conduction- the impulse travels along nerve pathways to the spinal cord or directly to the brain Perception- perception, or awareness and interpretation of stimuli happens in the brain where specialized brain cells interpret the nature and quality of the sensory stimuli. The LOC affects the perception of stimuli PROMOTING NORMAL SENSORY PERCEPTION STRUCTURE and FUNCTION of SENSORY PERCEPTION Sensory Awareness -Reticular activating systemresponsible for bringing together information from the cerebellum and other parts of the brain with that obtained from the sense organs Input by senses -Special senses-vision, hearing, smell and taste -Somatic senses-touch, kinesthetics (or proprioceptive) sensation, and visceral sensation PROMOTING NORMAL SENSORY PERCEPTION SENSORISTASIS- state of optimum arousal-not too much not too little ADAPTATION beyond the point of sensoristasis AWARENESS ability to perceive environmental stimuli and body reactions and to respond appropriately through thought and action. FACTORS AFFECTING SENSORY PERCEPTION Environment, Previous Experience, Lifestyle and Habits, Illness, Medications, Variations in Stimulation, Sensory deprivation SENSORY ALTERATIONS SENSORY DEPRIVATION- decrease in or lack of meaningful stimuli SENSORY DEFICIT- impaired reception, perception, or both, of one or more of the senses. SENSORY OVERLOAD- occurs when a person unable to process or manage the amount or intensity of the sensory stimuli - Factors: Increased quality and quantity of internal stimuli Increased quality and quantity of external stimuli Inability to disregard stimuli selectively
ALTERED SENSORY PERCEPTION FUNCTION Manifestations of Altered Sensory Perception function Anxiety, Cognitive Dysfunction, Hallucinations and delusions, Sensory deficits, Depression and withdrawal NURSING PROCESS ASSESSMENT Normal pattern identification Risk identification -Sensory overload- Lengthy verbal explanations before the procedure -Room close to the nurses station -Bright lights -Use of ECG monitor, mechanical ventilators, Oxygen ,IV tubes other equipment -Frequent treatments -Sensory deprivation -Private room, eyes bandaged, bedrest, sensory aid not available isolation precautions, few visitors ASSESSMENT CHARACTERISTICS OF NORMAL SENSORY PERCEPTION Normal vision-visual acuity at or near 20/20, full field of vision and tricolor vision (red, green and blue) Normal hearing-auditory acuity of sounds at an intensity of 0 to 25 dB, at frequencies of 125 to 8000 cycles per second Normal taste- ability to discriminate sour, salty, sweet and bitter Normal smell-discrimination of primary odours such as musky, floral, pepperminty, pungent Somatic senses-discrimination of touch, pressure, vibration, position, tickling, temperature and pain State of Awareness Full consciousness Alert; oriented to time, place, person; understands verbal and written words Disoriented Not oriented to time, place, or person Confused Reduced awareness, easily bewildered; poor memory, misinterprets stimuli; impaired judgment Somnolent Extreme drowsiness but will respond to stimuli Semicomatose Can be aroused by extreme or repeated stimuli Coma Will not respond to verbal stimuli NURSING PROCESS PHYSICAL ASSESSMENT Vision- use of snellen chart to measure visual acuity (or have the client read newspaper, menu or whatever) Smell- with eyes closed, have client identify 3 odors, such as coffee, tobacco and cloves, one nostril at a time, while occluding the other nostril Hearing- whisper numbers in each ear, while occluding the other; ask the client to repeat; perform Weber and Rinne tuning fork test WEBERS TEST- assesses bone conduction by testing the lateralization ( sideward transmission) of sounds.
RINNE TEST- test compares air conduction to bone conduction Sound conducted by air is heard more readily than sound conducted by bone. Taste-with eyes closed, have client identify 3 tastes such as lemon, salt, and sugar, waiting 1 minute and giving sips of water in between. Somatic sensations-Test light touch of extremities with a wisp of cotton; test sharp and dull sensation using the point and blunt end of a pin; test two-point discrimination using two pins held close together; test hot and cold sensation using test tube filled with warm and cold water; test position sense by moving the clients fingers or toes ELECTROENCEPHALOGRAM (EEG) OR Brain wave test An electroencephalogram (EEG) is a test to measure the electrical activity of the brain. How the Test is Performed Brain cells talk to each other by producing tiny electrical signals, called impulses. An EEG helps measure this activity. The test is done by a EEG specialist in your doctor's office or at a hospital or laboratory. You will be asked to lie on your back on a bed or in a reclining chair. Flat metal disks called electrodes are placed all over your scalp. The disks are held in place with a sticky paste. The electrodes are connected by wires to a speaker and recording machine. The recording machine changes the electrical signals into patterns that can be seen on a computer. It looks like a bunch of wavy lines. You will need to lie still during the test with your eyes closed because movement can change the results. But, you may be asked to do certain things during the test, such as breathe fast and deeply for several minutes or look at a bright flashing light. How to Prepare for the Test Wash your hair the night before the test. Do not use any oils, sprays, or conditioner on your hair before this test. If you have a hair weave, you may want to ask your doctor or nurse for special instructions. Your health care provider may want you to stop taking certain medications before the test. Do not change or stop taking medications without first talking to your health care provider. Bring a list of your medications with you. Avoid all food and drinks containing caffeine for 8 hours before the test.
Sometimes you may need to sleep during the test, so you may be asked to reduce your sleep time the night before. If you are asked to sleep as little as possible before the test, do not eat or drink any caffeine, energy drinks, or other products that help you stay awake. How the Test Will Feel The electrodes may feel sticky and strange on your scalp but should not cause any other discomfort. You should not feel any discomfort during the test. Why the Test is Performed EEG is used to look at your brain activity. It can help diagnose seizures. It may also be used to diagnose or monitor the following health conditions: Abnormal changes in body chemistry that affect the brain Brain diseases such as Alzheimer's disease Confusion Head injuries Infections Tumors EEG is also used to: Evaluate problems with sleep ( sleep disorders) Investigate periods of unconsciousness Monitor the brain during brain surgery An EEG may be done to show that the brain has no activity, in the case of someone who is in a deep coma. It can be helpful when trying to decide if someone is brain dead. EEG cannot be used to measure intelligence. Normal Results Brain electrical activity has a certain number of waves per second (frequencies) that are normal for different levels of alertness. For example, brain waves are faster when you are awake, and slower when you are sleeping. There are also normal patterns to these waves. Abnormal Results Mean Abnormal results on an EEG test may be due to: Abnormal bleeding (hemorrhage) An abnormal structure in the brain (such as a brain tumor) Attention problems Tissue death due to a blockage in blood flow (cerebral infarction) Drug or alcohol abuse Head injury Migraines (in some cases) Seizure disorder (such as epilepsy or convulsions) Sleep disorder (such as narcolepsy) Swelling of the brain (encephalitis) Note: A normal EEG does not mean that a seizure did not occur.
Risks The procedure is very safe. However, the flashing lights or fast breathing (hyperventilation) required during the test may trigger seizures in those with seizure disorders. The health care provider performing the EEG is trained to take care of you if this happens. It may be difficult to get the paste out of your hair, but it should come out after a few washings with regular shampoo. Cerebral angiography Cerebral angiography is a procedure that uses a special dye (contrast material) and x-rays to see how blood flows through the brain. How the Test is Performed Cerebral angiography is done in the hospital or radiology center. You will be asked to lie on an x-ray table. Your head is held still using a strap, tape, or sandbags, so you do not move it during the procedure. Before the test starts, you will be given a mild sedative to help you relax. Electrocardiogram (ECG) is used to monitor your heart activity during the test. Sticky patches, called leads, will be placed on your arms and legs. Wires connect the leads to the ECG machine. An area of your body, usually the groin, is cleaned and numbed with a local numbing medicine (anesthetic). A thin, hollow tube called a catheter is placed through an artery and carefully moved up through the main blood vessels in the belly area and chest and into an artery in the neck. X-rays help guide the doctor to the correct position. Once the catheter is in place, a special dye (contrast material) goes through the catheter. X-ray images are taken to see how the dye moves through the artery and blood vessels of the brain. The dye helps highlight any blockages in blood flow. Sometimes, a computer removes the bones and tissues on the images being viewed, so that only the blood vessels filled with the contrast dye are seen. This is called digital subtraction angiography (DSA). After the x-rays are taken, the needle and catheter are withdrawn. Pressure is immediately applied on the leg at the site of insertion for 10 - 15 minutes to stop the bleeding. After that time, the area is checked and a tight bandage is applied. Your leg should be kept straight for 4 6 hours after the procedure. Watch the area for bleeding for at least the next 12 hours. How to Prepare for the Test Before the procedure, your health care provider will examine you and order blood tests.
Tell the health care provider if you: Are allergic to shellfish or iodine substances Have a history of bleeding problems Have had an allergic reaction to x-ray contrast dye or any iodine substance May be pregnant You may be told not to eat or drink anything for 4 to 8 hours before the test. You must sign a consent form. Your health care provider will explain the procedure and its risks. When you arrive at the testing site, you will be given a hospital gown to wear. You must remove all jewelry. How the Test Will Feel The x-ray table may feel hard and cold. You may ask for a blanket or pillow. Some people feel a sting when the numbing medicine (anesthetic) is given. You will feel a brief, sharp pain and pressure as the catheter is moved into the body. The contrast may cause a warm or burning feeling of the skin of the face or head. You may have slight tenderness and bruising at the site of the injection after the test. Why the Test is Performed Cerebral angiography is most frequently used to identify or confirm problems with the blood vessels in the brain. Your doctor may order this test if you have symptoms or signs of: Abnormal blood vessels (vascular malformation) Aneurysm Narrowing of the arteries in the brain Vasculitis It is sometimes used to: Confirm a brain tumor Evaluate the arteries of the head and neck before surgery Find a clot that may have caused a stroke In some cases, this procedure may be used to get more detailed information after something abnormal has been detected by an MRI or CT scan of the head. This test may also be done in preparation for medical treatment (interventional radiology procedures) by way of certain blood vessels. Abnormal Results Mean Contrast dye flowing out of the blood vessel may be a sign of internal bleeding.
Narrowed arteries may suggest cholesterol deposits, a spasm, or inherited disorders. Out of place blood vessels may be due to brain tumors, bleeding within the skull, aneurysm (bulging of the artery walls), or arteriovenous malformation. Abnormal results may also be due to: Intracerebral hemorrhage Metastatic brain tumor Neurosyphilis Optic glioma Pituitary tumor Primary brain tumors Risks There is the possibility of significant complications, including: Allergic reaction to the contrast dye Blood clot or bleeding at the needle stick site, which could partly block blood flow to the leg Damage to an artery or artery wall from the catheter, which can block blood flow and cause a stroke (rare) Considerations Tell your health care provider immediately if you have: Facial weakness Numbness in your leg during or after the procedure Slurred speech Vision problems Ventriculogram A ventriculogram is a test done during cardiac catheterization that evaluates the main pumping chamber of your heart (left ventricle). During a ventriculogram, your doctor injects a dye into your heart that makes the inside of your heart show up on X-ray. The images are recorded on film or on a computer. A ventriculogram can show: The movement of your heart muscle as your left ventricle fills and pumps blood. The size of your left ventricle. How efficiently your left ventricle pumps blood (ejection fraction). How well blood flows through your heart valves (aortic and mitral valves). Visual, Auditory, and Kinesthetic Learning Styles (VAK) The VAK learning style uses the three main sensory receivers: Visual, Auditory, and Kinesthetic (movement) to determine the dominant learning style. It is sometimes known as VAKT (Visual, Auditory, Kinesthetic, & Tactile). It is based on modalitieschannels by which human
expression can take place and is composed of a combination of perception and memory. VAK is derived from the accelerated learning world and seems to be about the most popular model nowadays due to its simplicity. While the research has shown a connection with modalities and learning styles (University of Pennsylvania, 2009), the research has so far been unable to prove the using one's learning style provides the best means for learning a task or subject. This is probably because it is more of a preference, rather than a style. Hints for Recognizing and Implementing the Three VAK Styles Auditory learners often talk to themselves. They also may move their lips and read out loud. They may have difficulty with reading and writing tasks. They often do better talking to a colleague or a tape recorder and hearing what was said. To integrate this style into the learning environment: Begin new material with a brief explanation of what is coming. Conclude with a summary of what has been covered. This is the old adage of tell them what they are going to lean, teach them, and tell them what they have learned. Use the Socratic method of lecturing by questioning learners to draw as much information from them as possible and then fill in the gaps with you own expertise. Include auditory activities, such as brainstorming, buzz groups, or Jeopardy. Leave plenty of time to debrief activities. This allows them to make connections of what they leaned and how it applies to their situation. Have the learners verbalize the questions. Develop an internal dialogue between yourself and the learners.
Visual learners have two sub-channelslinguistic and spatial. Learners who are visual-linguistic like to learn through written language, such as reading and writing tasks. They remember what has been written down, even if they do not read it more than once. They like to write down directions and pay better attention to lectures if they watch them. Learners who are visual-spatial usually have difficulty with the written language and do better with charts, demonstrations, videos, and other visual materials. They easily visualize faces and places by using their imagination and seldom get lost in new surroundings. To integrate this style into the learning environment: Use graphs, charts, illustrations, or other visual aids. Include outlines, concept maps, agendas, handouts, etc. for reading and taking notes.
Include plenty of content in handouts to reread after the learning session. Leave white space in handouts for note-taking. Invite questions to help them stay alert in auditory environments. Post flip charts to show what will come and what has been presented. Emphasize key points to cue when to takes notes. Eliminate potential distractions. Supplement textual information with illustrations whenever possible. Have them draw pictures in the margins. Have the learners envision the topic or have them act out the subject matter.
You will be asked to remove your glasses or contact lenses and stand or sit 20 feet from the eye chart. You will keep both eyes open. You will be asked to cover one eye with the palm of your hand, a piece of paper, or a small paddle while you read out loud the smallest line of letters you can see on the chart. Numbers or pictures are used for people who cannot read, especially children. If you are not sure of the letter, you may guess. This test is done on each eye, one at a time. If needed, it is repeated while you wear your glasses or contacts. You may also be asked to read letters or numbers from a card held 14 inches from your face. This will test your near vision. How to Prepare for the Test No special preparation is necessary for this test. How the Test Will Feel There is no discomfort. Why the Test is Performed The visual acuity test is a routine part of an eye examination or general physical examination, particularly if there is a change in vision or a problem with vision. In children, the test is performed to screen for vision problems. Vision problems in young children can often be corrected or improved. Undetected or untreated problems may lead to permanent vision damage. There are other ways to check vision in very young children, or in people who do not know their letters or numbers. Normal Results Visual acuity is expressed as a fraction. The top number refers to the distance you stand from the chart. This is usually 20 feet. The bottom number indicates the distance at which a person with normal eyesight could read the same line you correctly read. For example, 20/20 is considered normal. 20/40 indicates that the line you correctly read at 20 feet away can be read by a person with normal vision from 40 feet away. Even if you miss one or two letters on the smallest line you can read, you are still considered to have vision equal to that line. What Abnormal Results Mean Abnormal results may be a sign that you need glasses or contacts. Or it may mean that you have an eye condition that needs further evaluation by a health care provider. Risks
Kinesthetic learners do best while touching and moving. It also has two sub-channels: kinesthetic (movement) and tactile (touch). They tend to lose concentration if there is little or no external stimulation or movement. When listening to lectures they may want to take notes for the sake of moving their hands. When reading, they like to scan the material first, and then focus in on the details (get the big picture first). They typically use color high lighters and take notes by drawing pictures, diagrams, or doodling. To integrate this style into the learning environment: Use activities that get the learners up and moving. Play music, when appropriate, during activities. Use colored markers to emphasize key points on flip charts or white boards. Give frequent stretch breaks (brain breaks). Provide toys such as Koosh balls and Play-Dough to give them something to do with their hands. To highlight a point, provide gum, candy, scents, etc. which provides a cross link of scent (aroma) to the topic at hand (scent can be a powerful cue). Provide high lighters, colored pens and/or pencils. Guide learners through a visualization of complex tasks. Have them transfer information from the text to another medium such as a keyboard or a tablet.
Visual acuity test The visual acuity test is used to determine the smallest letters you can read on a standardized chart (Snellen chart) or a card held 20 feet away. Special charts are used when testing at distances shorter than 20 feet. How the Test is Performed This test may be done in a health care provider's office, a school, a workplace, or elsewhere.
There are no risks. Alternative Names Eye test - acuity; Vision test - acuity; Snellen test Visual Field Test A visual field test is a method of measuring an individual's entire scope of vision, that is their central and peripheral (side) vision. Visual field testing actually maps the visual fields of each eye individually. The visual field test is a subjective examination, requiring the patient to understand the testing instructions, fully cooperate, and complete the entire test in order to provide useful information. What is a visual field test used for? Visual field testing is most frequently used to detect any signs of glaucoma damage to the optic nerve. In addition, visual field tests are useful for detection of central or peripheral retinal disease, eyelid conditions such as ptosis or drooping, optic nerve disease, and diseases affecting the visual pathways within the brain. The visual pathways carry information from the eye to the visual or occipital cortex in the brain, where this information is processed into vision. How is visual field testing done? There are a variety of methods utilized to measure the visual fields. Virtually all visual field testing is performed one eye at a time, with the opposite (contralateral) eye completely covered to avoid errors. In all testing, the patient must look straight ahead at all times in order to avoid testing the central vision rather than the periphery. Most modern visual field testing devices also continuously monitor fixation, or the ability of the patient to maintain a consistent straight ahead gaze. To summarize, visual field testing is useful for numerous reasons: screening for glaucoma, testing patient with glaucoma for treatment response, screening and testing for lid droop or ptosis, particularly for insurance approval of lid lift surgical procedures, testing for macular diseases such as macular degeneration or toxicity from certain medications such as Plaquenil used for rheumatoid arthritis, testing for peripheral retinal disease such as retinal detachment or retinitis pigmentosa, testing for malingerers, or patients who may have secondary gains from poor vision, such as a false insurance claim, testing the function of the optic nerve looking for tumor, injury, poor circulation or stroke, .
compression from swelling in the eye socket or orbit, or severe dietary deficiency, testing the visual pathways to the brain, looking for tumor, brain swelling, injury, or poor circulation, and testing the visual or occipital cortex, looking for tumor, injury, brain swelling, or poor circulation.
A crude visual field test can be done by having the patient look straight ahead and count the fingers shown by the examiner from the side. More typically, however, visual fields are measured by a computerized assessment in an optometrist's, ophthalmologist's, or neurologist's office. For these procedures, one eye is covered and the patient places his or her chin in a bowl-shaped chin rest. Then, when the patient sees lights or movement of various intensities and at different locations, he or she pushes a button. In all standardized testing, the right eye is tested first, followed by the left eye. This process produces a computerized map of the visual field. Thus, visual field testing can be grouped into several important categories: Confrontational: The test is given one on one by a doctor or technician as a screening tool, in which peripheral finger movements are brought from the far periphery to the near periphery in four quadrants Amsler grid: It's an important tool to test macular vision in and around the center of the retina and detect specific conditions such as macular degeneration Static perimetry: The most common type of modern visual field testing employs a device with fixed light sources, either stationary pinpoint light sources or projected dots within a large white bowl. Popular devices include the Octopus or the Humphrey-Zeiss field analyzer. These tests are automated and run by the onboard computer, thus minimizing the time spent by a technician running the test. Kinetic perimetry: The process utilizes moving light sources, such as the traditional workhorse Goldman perimeter. This test produces an island map of peripheral visual perception intensity. Fixation monitoring as well as movement of the light source require a dedicated trained technician throughout the entire test. This test is particularly useful in weeding out malingerers. Frequency doubling analysis: This test utilizes varying intensities of a shimmering grid of light in standardized sectors of the peripheral and central visual field. It is particularly useful in
detecting early glaucoma field loss and can be about 40% more sensitive in doing so than standard static or kinetic perimetry. Visual field testing is generally covered by virtually all health-care insurance plans. Testing may be limited to one time per year for patients who are called glaucoma suspects, that is, likely to develop glaucoma in the future. Insurance plans usually allow two visual field tests per year for patients who have already been diagnosed with glaucoma. These visual field testing devices all incorporate an internal computer with the ability to store, print, and transmit important patient data. The field report generated by modern visual field devices includes a wealth of information, all of which can be useful to the doctor interpreting the results: Fixation errors: the number of times the patient looks away from the central target. This is a key indicator of patient cooperation or fatigue. False positives: the number of times the patient pushes the button when, in reality, a light source is not illuminated. False negatives: the number of times the patient fails to push the button when, in reality, there is a light source illuminated. These spots can be repeat tested by the onboard computer at exactly the same spot to best understand the patient's ability to produce an accurate field test. Points tested: indicates the total number of separately illuminated testing points, and therefore data points presented to the patient for testing. Reliable patients can produce a very useful field with a limited number of test points. Reliability index: the overall reliability of the patient's testing for each eye. Poor reliability may indicate patient fatigue, insufficient understanding of the test, or poor vision for other reasons such as cataracts. Visual field tests can also be used to ferret out malingerers. Standard deviation: the difference in peripheral field acuity when compared to a normative data base, or simply put, a large group of similar normal patients. This tells the doctor whether or not a particular part of the peripheral field is normal, depressed, or absent. Visual field map: the final basic report indicating the patient's visual field anywhere from the central 10 degrees all the way out to the farthest reaches of the field at 90 degrees. Altered patterns in the field map from reliable patient testing are often extremely useful in the diagnosis of ocular or neurological disorders.
most otherwise healthy patients, but it may be moderately tiring or stressful for ill or elderly patients. Visual field testing is also very difficult for younger children or patients with mental disabilities or developmental delay, such as Down's syndrome for example. Common testing time for visual fields in both eyes: Amsler grid: one minute Confrontational field: two minutes Static field for glaucoma screen: eight minutes Static field for lid droop or ptosis screen: eight minutes Static field for complete glaucoma evaluation: 15 minutes Kinetic Goldman field for complete glaucoma evaluation: 20 minutes Frequency doubling analysis for glaucoma screen or evaluation: 10 minutes
A visual field test is used to assess a person's central and peripheral vision and detect signs of glaucoma damage to the optic nerve, eyelid conditions such as ptosis, optic nerve disease, and diseases that affect visual pathways in the brain. Ophthalmoscopy Ophthalmoscopy is an examination of the back part of the eye (fundus), which includes the retina, optic disc, choroid, and blood vessels. How the Test is Performed There are different types of ophthalmoscopy. Direct ophthalmoscopy: You will be seated in a darkened room. The health care provider performs this common exam by shining a beam of light through the pupil using an instrument called an ophthalmoscope. An ophthalmoscope is about the size of a flashlight. It has a light and several different tiny lenses that allow the examiner to view the back of the eyeball. Indirect ophthalmoscopy: You will either lie or sit in a semi-reclined position. The health care provider holds your eye open while shining a very bright light into the eye using an instrument worn on the head. (The instrument looks like a miner's light.) The health care provider views the back of the eye through a hand-held lens held close to your eye. Some pressure may be applied to the eyeball using a small, blunt probe. You will be asked to look in various directions. Slit-lamp ophthalmoscopy: You will sit in a chair with the instrument placed in front of you. You will be asked to rest your chin and forehead on a support to keep your head steady. The health care provider will use the microscope part of the slit lamp and a tiny lens placed close to the front of the eye. The health care provider can see about the same with this technique as with indirect ophthalmoscopy, but with higher magnification.
The visual field test generally is performed after visual acuity testing, but before examination by the doctor. Visual field testing requires a minimal amount of time for
The opthalmoscopy examination usually takes about 5 to 10 minutes. How to Prepare for the Test Indirect ophthalmoscopy and slit-lamp ophthalmoscopy are performed after eyedrops are placed to widen (dilate) the pupils. Direct ophthalmoscopy and slit-lamp ophthalmoscopy can be performed with or without the pupil dilated. The eyedrops may make it hard for you to focus your eyes for several hours. You should arrange to have someone drive you after the examination. Wearing sunglasses or tinted lenses will help make your dilated pupils more comfortable. You should tell the health care provider if you: Are allergic to any medicines Are taking any medicines Have glaucoma or a family history of glaucoma How the Test Will Feel The bright light will be uncomfortable, but the test is not painful. You may briefly see images after the light shines in your eyes. The light is brighter with indirect ophthalmoscopy, so the sensation of seeing after-images may be greater. Pressure on the eye during indirect ophthalmoscopy by may be slightly uncomfortable, but it should not be painful. If eyedrops are used, they may sting briefly when placed in the eyes. You may also have an unusual taste in your mouth. Why the Test is Performed Ophthalmoscopy is done as part of a routine physical or complete eye examination. It is used to detect and evaluate symptoms of retinal detachment or eye diseases such as glaucoma. Ophthalmoscopy may also be done if you have signs or symptoms of high blood pressure, diabetes, or other diseases that affect the blood vessels. Normal Results The retina, blood vessels, and the optic disc should appear normal. What Abnormal Results Mean Abnormal results may be seen on ophthalmoscopy with any of the following conditions: CMV retinitis
Diabetes Glaucoma High blood pressure Macular degeneration Melanoma of the eye Optic nerve problems Retinal tear or detachment
Risks The test itself involves no risk. The dilating eye drops may rarely cause: An attack of narrow-angle glaucoma Dizziness Dryness of the mouth Flushing Nausea Vomiting If glaucoma is suspected, drops usually are not used.
Considerations Ophthalmoscopy is considered to be 90-95% accurate. It can detect the early stages and effects of many serious diseases. Alternative Names Funduscopy Slit-lamp exam The slit-lamp examination looks at structures that are at the front of the eye. How the Test is Performed The slit-lamp is a low-power microscope combined with a high-intensity light source that can be focused to shine in a thin beam. You will sit in a chair with the instrument placed in front of you. You will be asked to rest your chin and forehead on a support to keep your head steady. The health care provider will examine your eyes, especially the eyelids, cornea, conjunctiva, sclera, and iris. Often a yellow dye (fluorescein) is used to help examine the cornea and tear layer. The dye is either added as a drop, or the health care provider may touch a fine strip of paper stained with the dye to the white of your eye. The dye rinses out of the eye with tears as you blink. Next, drops may be placed in your eyes to widen (dilate) your pupils. The drops take about 15 to 20 minutes to work. The slit-lamp examination is then repeated using another small lens held close to the eye, so the back of the eye can be examined. How to Prepare for the Test No special preparation is necessary for this test.
How the Test Will Feel Your eyes will be sensitive to light for a few hours after the exam if dilating drops are used. Why the Test is Performed This test is used to examine the: Conjunctiva Cornea Eyelids Iris Lens Sclera Normal Results Structures in the eye are found to be normal.
What Abnormal Results Mean The slit lamp exam may detect many diseases of the eye, including: Cataract Corneal injury Dry eye syndrome Macular degeneration Retinal detachment Retinal vessel occlusion Retinitis pigmentosa Uveitis This list does not include all possible diseases of the eye. Risks The dilating drops may cause increased pressure in the eye with nausea and pain. This is very rare, but you should return to your doctor's office right away if you experience either of these symptoms. Alternative Names Biomicroscopy
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- ScrabbleDocument4 pagesScrabblepatricia anne guela89% (9)
- Charlie and The Chocolate Factory Lesson PlanDocument6 pagesCharlie and The Chocolate Factory Lesson Plandarkblu0% (2)
- Lipids Lesson PlanDocument4 pagesLipids Lesson Planapi-270448768100% (1)
- An Open To Letter To Florida's GovernorDocument2 pagesAn Open To Letter To Florida's GovernorActionNewsJaxNo ratings yet
- Maths Revision Guide UpdatedDocument16 pagesMaths Revision Guide UpdatedPaul Cowen67% (3)
- Science Workbook 1 AnswersDocument4 pagesScience Workbook 1 AnswersPradeep Kumara80% (5)
- Ace 1.1Document1 pageAce 1.1Mae UsquisaNo ratings yet
- Nursing As Informed Caring For The Well-Being of Others: Kristen SwansonDocument6 pagesNursing As Informed Caring For The Well-Being of Others: Kristen SwansonMae UsquisaNo ratings yet
- Thesis FDDocument84 pagesThesis FDMae UsquisaNo ratings yet
- Thesis GRBDocument101 pagesThesis GRBMae UsquisaNo ratings yet
- Case Study Nasopharyngeal CancerDocument31 pagesCase Study Nasopharyngeal CancerMae UsquisaNo ratings yet
- Nursing As Informed Caring For The Well-Being of Others: Kristen SwansonDocument6 pagesNursing As Informed Caring For The Well-Being of Others: Kristen SwansonMae UsquisaNo ratings yet
- Why Do You Think Nursing Is A Global ProfessionDocument2 pagesWhy Do You Think Nursing Is A Global ProfessionMae Usquisa100% (1)
- Giving The Client A Back MassageDocument13 pagesGiving The Client A Back MassageMae UsquisaNo ratings yet
- ResumeDocument3 pagesResumeMae UsquisaNo ratings yet
- Jarmaine Claire P. Paguirigan Bsa 2Document1 pageJarmaine Claire P. Paguirigan Bsa 2Mae UsquisaNo ratings yet
- Practice Test IIDocument18 pagesPractice Test IIShella Marie Usquisa100% (3)
- Introduction OADocument3 pagesIntroduction OAMae UsquisaNo ratings yet
- CancerDocument41 pagesCancerMae UsquisaNo ratings yet
- Maternity NursingDocument18 pagesMaternity NursingMae UsquisaNo ratings yet
- Jay AnnDocument8 pagesJay AnnMae UsquisaNo ratings yet
- Answer - Fundamentals of Nursing IV: Nursing Process, Physical and Health Assessment and Routine ProceduresDocument15 pagesAnswer - Fundamentals of Nursing IV: Nursing Process, Physical and Health Assessment and Routine ProceduresMae UsquisaNo ratings yet
- St. Paul University Philippines: Action PlanDocument3 pagesSt. Paul University Philippines: Action PlanMae UsquisaNo ratings yet
- ResumeDocument5 pagesResumeMae UsquisaNo ratings yet
- St. Paul University Philippines: Tuguegarao City, Cagayan 3500 School of Health SciencesDocument1 pageSt. Paul University Philippines: Tuguegarao City, Cagayan 3500 School of Health SciencesMae UsquisaNo ratings yet
- RizalDocument1 pageRizalMae UsquisaNo ratings yet
- Ap Studio Art DrawingDocument6 pagesAp Studio Art Drawingapi-304919709No ratings yet
- Call Iyt English 2019Document5 pagesCall Iyt English 2019Facultad de Ingeniería Universidad de AntioquiaNo ratings yet
- TQM, Why People Late Come To Class (Fishbone)Document7 pagesTQM, Why People Late Come To Class (Fishbone)Mohammad Fadhli0% (1)
- 08 - Chapter 1 PDFDocument38 pages08 - Chapter 1 PDFVaishnavi GnanasekaranNo ratings yet
- COntrol Systems Book Georgia TechDocument1 pageCOntrol Systems Book Georgia TechSachin AngadiNo ratings yet
- Summer Reading Camp Community Partnership Grant: S S C Department of EducationDocument49 pagesSummer Reading Camp Community Partnership Grant: S S C Department of Educationjimmylita echavezNo ratings yet
- Global Literacy Challenge & Enquiry PackDocument170 pagesGlobal Literacy Challenge & Enquiry PackStirlingLfSNo ratings yet
- Daisy - Soriano - LR Rapid AssessmentDocument3 pagesDaisy - Soriano - LR Rapid Assessmentdaisy sorianoNo ratings yet
- Willes and Bondi-1989 ModelDocument11 pagesWilles and Bondi-1989 ModelAshis kar100% (1)
- SCS Paper B September 2012 - FinalDocument2 pagesSCS Paper B September 2012 - FinalYZ WandiNo ratings yet
- Guess The WordDocument2 pagesGuess The WordPaula Cristina Mondaca AlfaroNo ratings yet
- Methods of Empirical ResearchDocument68 pagesMethods of Empirical ResearchSuren TheannilawuNo ratings yet
- Micro TeachingDocument9 pagesMicro TeachingDANIEL TSHABALALANo ratings yet
- Participation RubricDocument2 pagesParticipation RubricCarmen Ibañez AlvarezNo ratings yet
- Usf Lesson Plan Template Oct 4Document4 pagesUsf Lesson Plan Template Oct 4api-337071056No ratings yet
- Week: 3 Class / Subject Time Topic/Theme Focus Skill Content Standard Learning Standard Learning ObjectivesDocument9 pagesWeek: 3 Class / Subject Time Topic/Theme Focus Skill Content Standard Learning Standard Learning ObjectivesAlya FarhanaNo ratings yet
- Math g7 m1 Topic A Lesson 1 TeacherDocument8 pagesMath g7 m1 Topic A Lesson 1 TeacherbangiidamanNo ratings yet
- BSED Syllabus Assessment in Learning1Document17 pagesBSED Syllabus Assessment in Learning1Marimar LiwanagNo ratings yet
- Leave of Absence Form: InstructionsDocument2 pagesLeave of Absence Form: InstructionsCharo GironellaNo ratings yet
- Final ResumeDocument2 pagesFinal Resumeapi-241949549No ratings yet
- Understanding The Embrace of Filipino Te PDFDocument9 pagesUnderstanding The Embrace of Filipino Te PDFrizhmeenNo ratings yet
- Arusha Technical College - Prospectus 2012/2013Document151 pagesArusha Technical College - Prospectus 2012/2013Gasto LeseiyoNo ratings yet
- Reference Essays For Crime TopicsDocument7 pagesReference Essays For Crime Topicsapi-300866770No ratings yet
- Jonathan Law Senior SpotlightDocument1 pageJonathan Law Senior SpotlightNHRSportsNo ratings yet