Professional Documents
Culture Documents
Nursing Care Plan Fever
Uploaded by
Vincent QuitorianoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan Fever
Uploaded by
Vincent QuitorianoCopyright:
Available Formats
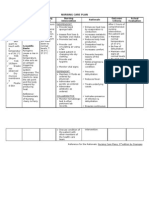
Nursing Care Plan
29
ASSESSMENT Subjective: Mataas pa rin ang lagnat nya hanggang ngayonas verbalized by the patients mother. Objective: Flushed skin Skin is warm to touch Temp: 38.2*C PR: 109 RR: 34
DIAGNOSIS Hyperthermia related to positive bacterial infection as manifested by flushed and warm to touch skin.
PLANNING
INTERVENTION
EVALUATION After all the nursing intervention the clients body temp subsided within the normal range.
Short term: within 1 hour of Independent: nursing intervention the patients elevated temperature of 36.2 will lessen to 37.4 degree Celsius. Long term: within 3 consecutive days of nursing intervention, the patients body temperature will return to its normal range. Established rapport to mother to gain trust and cooperation. Promote surface cooling by means of undressing ( heat loss by radiation and conduction) Demonstrate on how to do a proper tepid sponge bath using wet and dry cloth. Provide nutritious diet to meet increase metabolic demands
Dependent: Administer antipyretic as ordered.
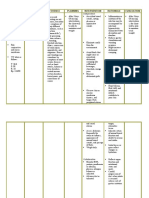
Nursing Care Plan
ASSESSMENT Subjective: Umiiyak yan kapag nahahawakan yung batok nya saka nung may ginawa yung doctor nya as verbalized by the mother. DIAGNOSIS Acute pain related to meningeal infection with spasm of extensor muscle (neck, shoulder and back) as manifested by positive kernigs and brudzinskis sign. Objective: Facial grimace Irritable (+) Brudzinskis sign (+)Kernigs sign Promote rest in the room by keeping stimulation and the room to minimum Institute respiratory isolation Monitor and record carefully intake and output. Position on the side with head gently supported in extension PLANNING Within 3 hours of nursing intervention the patients pain from 8 will reduce to 4 using the facial pain rating scale. INTERVENTION Independent: Use pain rating scale appropriate to its age Assess for neurologic exam and vital signs
30
EVALUATION After 3 hours of nursing intervention there is no sign of facial grimace and irritability in the patient.
Nursing Care Plan
ASSESSMENT Objective: Facial grimace Irritable (+) Brudzinskis sign (+)Kernigs sign DIAGNOSIS Impaired Social Interaction related to decreased level of consciousness, hospitalization, and isolation PLANNING After 8 hours of nursing intervention The childs social interaction will be Near normal despite isolation. Encourage parents to help with daily activities such as feeding and Bathing. INTERVENTION Educate parents and other visitors to use proper infection control Techniques. Rationale Family members help fulfil the emotional and social needs of the ill And contagious child. Parental involvement in the childs care provides the child with a sense of security and emotional wellbeing. Parents have a sense of control and a feeling that they are doing something to enhance the Childs recovery. Have age-appropriate Providing the
31
EVALUATION The childs social and developmental needs are met by family members despite the childs illness and Hospitalization.
games and Toys in the room. Play with the Child. When the child is feeling better, encourage watching television/videotape or listening to The radio/audiotape. Arrange for hearing assessment prior to discharge
child with toys and games as well as sensory stimulation helps the child achieve A sense of wellbeing.
Hearing loss is a common Complication. Early intervention is needed to promote g
32
Nursing Care Plan
ASSESSMENT Subjective: masakit ang ulo ko as verbalized by the patient. Objective: Restlessness Change in motor or sensory responses Difficulty in swallowing skin discoloration decrease motor response Demonstrate behaviours/lifestyle changes to improve circulation. DIAGNOSIS Risk for ineffective cerebral Tissue perfusion related to cerebraledema PLANNING After 8 hrs. of nursing interventions, the client will demonstrate stable Vital signs and absence of signs of intracranial pressure. Instruct patient to avoid or limit coughing, Vomiting, straining at defecation, bearing down as possible. R: These activities increase thoracic and intra-abdominal pressure which can increase intracranial pressure. Elevate head and maintain head/neck in midline neutral position Prevention: Observe for seizure activity R: Seizure can occur as INTERVENTION Independent: Decrease extraneous stimuli and provide comfort measures like back massage, quiet environment, soft voice. R: Provides calming effect, reduces Adverse physiological response and promotes rest to maintain or lower intracranial pressure. Rationale
33
EVALUATION After 8 hrs. Of nursing interventions, the client demonstrated stable Vital signs and absence of signs of intracranial pressure.
R: to promote circulation/venous drainage
and protect patient from injury.
result of cerebral irritation, hypoxia or increase intracranial pressure.
Maintain head or neck in midline or neutral position, R: Turning head to one
support with small towel rolls side compresses the and pillows: Provide rest periods between care activities and limit duration of procedures. jugular veins and inhibits cerebral venous drainage, thereby increasing intracranial pressure.
R: Continual activity can increase intracranial Curative: Administer supplemental oxygen as indicated pressure
R: Reduces hypoxemia. Investigate reports of pain out of proportion to degree of injury: R: May reflect developing compartment syndrome
Administer
R: used to decrease
medications(antihypertensive, edema. diuretics)
Rehabilitation: Encourage quiet, restful atmosphere:
R: Conserves energy and lower oxygen demand
Limit daily activities and caution client to avoid strenuous activities
R: over exertion may cause dizziness
35
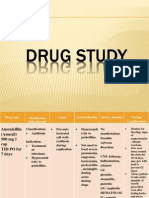
Nursing Care Plan
ASSESSMENT Subjective Dalawang araw na sya nagsususka as verbalized by the mother. Objective: Weak in appearance Irritable (+) Nausea and vomiting Temp: 37.4 RR 40 PR 105 Provide a flexible feeding schedule with small feedings of favourite foods. Minimise handling around feeding times. Assist the child with chewing with the childs chin and jaw in the nurses hand, if swallowing is impaired & if so Nausea and vomiting controlled. Position the infant or child upright after feeding. DIAGNOSIS Altered nutrition: less than body requirements related to restricted intake; nausea, and vomiting, swallowing and chewing difficulty. PLANNING The childs weight will be stable and appropriate for age, normal serum protein, moist mucous membrane and adequate urine output. Monitor skin turgor, mucous membrane and urine output. INTERVENTION Weight the child daily on the same scale and record on growth chart. EVALUATION
36
The child shows normal growth and development, nausea and vomiting under control, adequate daily caloric intake and proper hydration verbalized by the S.O.
feed by NG Tube. Consult dietician. Assess level of consciousness before giving liquids.
37
You might also like
- Fever Nursing Care PlanDocument3 pagesFever Nursing Care PlanMarie Anne T85% (39)
- Nursing Care Plan FeverDocument3 pagesNursing Care Plan Feverderic96% (69)
- Nursing Care Plan Problem Nursing Diagnosis Rationale Objective of Care Nursing Intervention Rationale EvaluationDocument1 pageNursing Care Plan Problem Nursing Diagnosis Rationale Objective of Care Nursing Intervention Rationale Evaluationplug06100% (1)
- NCP FeverDocument1 pageNCP FeverLuis Romnic Vinuya100% (2)
- NCP FeverDocument3 pagesNCP Feversinister1785% (48)
- NCP FeverDocument2 pagesNCP FeverMary Joyce LimoicoNo ratings yet
- Fever NCPDocument3 pagesFever NCPBruno MercuryNo ratings yet
- Nursing Care Plan HyperthermiaDocument1 pageNursing Care Plan Hyperthermiasamanthabox50% (2)
- Fever NCPDocument5 pagesFever NCPNikael Patun-ogNo ratings yet
- NCP For FeverDocument2 pagesNCP For FeverSherwin B. CaytapNo ratings yet
- Nursing Diagnosis HyperthermiaDocument2 pagesNursing Diagnosis HyperthermiaErl Driz100% (1)
- NCP Altered Body TemperatureDocument1 pageNCP Altered Body TemperatureKristine Young100% (3)
- NCP (Fever)Document2 pagesNCP (Fever)Kei-Ann Magpantay Aguila50% (2)
- Assessment Nursing Diagnosis Planning Implementation Rationale EvaluationDocument3 pagesAssessment Nursing Diagnosis Planning Implementation Rationale EvaluationChloie Marie RosalejosNo ratings yet
- Fever NCPDocument3 pagesFever NCPFretzy Quirao Villaspin100% (2)
- Doenges, Et. Al, (2008) - Nurse's Pocket Guide. 11 Edition. F.A. Davis Company. P. 385Document3 pagesDoenges, Et. Al, (2008) - Nurse's Pocket Guide. 11 Edition. F.A. Davis Company. P. 385Theresa AbrilloNo ratings yet
- "Nilalagnat Anak Ko. Kagabi Pa Po Siya Mainit" As: Objectives Nursing Interventions Rationale EvaluationDocument1 page"Nilalagnat Anak Ko. Kagabi Pa Po Siya Mainit" As: Objectives Nursing Interventions Rationale EvaluationMiguel LeybaNo ratings yet
- FEver NCPDocument1 pageFEver NCPSam AlipioNo ratings yet
- NCP (Hyperthermia)Document3 pagesNCP (Hyperthermia)Flauros Ryu Jabien100% (1)
- NCP FeverDocument2 pagesNCP FeverRic Velasco100% (2)
- NCP - HyperthermiaDocument2 pagesNCP - Hyperthermiagiadda91% (67)
- NCP HyperthermiaDocument3 pagesNCP HyperthermiaMarla NavarroNo ratings yet
- NCP Altered Thermoregulation HypothermiaDocument2 pagesNCP Altered Thermoregulation HypothermiaMaila Joy Pring Fuentes100% (10)
- NCP DengueDocument3 pagesNCP DengueYeana Alon50% (4)
- Altered Body Temp (NCP)Document2 pagesAltered Body Temp (NCP)John MIchael Ausa63% (8)
- Nursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAbdallah AlasalNo ratings yet
- Nursing Care Plan On FeverDocument15 pagesNursing Care Plan On Feverkamini ChoudharyNo ratings yet
- Hyperthermia NCPDocument5 pagesHyperthermia NCPJayson John Domingo89% (9)
- CHN NCPDocument2 pagesCHN NCPIna Marie Calungcaguin Castro100% (1)
- Assessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesAssessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDanica Kate GalleonNo ratings yet
- Nursing Care Plan Pulmonary TuberculosisDocument2 pagesNursing Care Plan Pulmonary Tuberculosisjenypot90% (96)
- Nursing Care Plan DiarrheaDocument2 pagesNursing Care Plan Diarrheaderic95% (43)
- NCP For CoughDocument6 pagesNCP For Coughmelerine16100% (5)
- NCP On HyperthermiaDocument3 pagesNCP On Hyperthermiamydrummer76% (17)
- Hyperthermia Pneumonia Nursing Care PlanDocument1 pageHyperthermia Pneumonia Nursing Care Planjustin_saneNo ratings yet
- Nursing Care PlanDocument10 pagesNursing Care PlanGinel Laquiores100% (1)
- NCPPPPDocument6 pagesNCPPPPIvan Liquiran AvenadoNo ratings yet
- Child - Major Burn PDFDocument3 pagesChild - Major Burn PDFAldith GrahamNo ratings yet
- Nursing Care PlanDocument11 pagesNursing Care PlanKevin John ReaLubit SaLisi100% (6)
- NCPsDocument4 pagesNCPspjcolitaNo ratings yet
- Nursing Care Plan For PostpartumDocument5 pagesNursing Care Plan For PostpartumTheeya Quigao91% (11)
- RNCPDocument5 pagesRNCPReymon Jan RodadoNo ratings yet
- NCP FinalDocument18 pagesNCP FinalJessica Medina100% (1)
- Rosilla, Leandro AGE: 5 Yrs Old Diagnosis: DHF IiiDocument4 pagesRosilla, Leandro AGE: 5 Yrs Old Diagnosis: DHF IiiAlexander Rodriguez OlipasNo ratings yet
- Diagnostic Procedure, Discharge Plan, NCP Imbalanced Nutri - MariscotesDocument4 pagesDiagnostic Procedure, Discharge Plan, NCP Imbalanced Nutri - MariscotesCindy MariscotesNo ratings yet
- Revised NCPDocument8 pagesRevised NCPKryza Dale Bunado BaticanNo ratings yet
- Nursing Diagnosis #1Document8 pagesNursing Diagnosis #1Ynez100% (1)
- NCP For Parent and ChildDocument3 pagesNCP For Parent and ChildEric Evangelista100% (1)
- Efremidis 4115p 6westconceptmapDocument2 pagesEfremidis 4115p 6westconceptmapapi-283407433No ratings yet
- Nursing An Orphanange in A Clien With DysmenorreheaDocument3 pagesNursing An Orphanange in A Clien With DysmenorreheaNadilaNo ratings yet
- Palliative Nursing Care PlanDocument5 pagesPalliative Nursing Care Planstudent_019No ratings yet
- Post Assessment PediatricsDocument4 pagesPost Assessment Pediatricscuicuita100% (4)
- Nursing Care PlanDocument10 pagesNursing Care PlanSittie Rohaina SabanNo ratings yet
- Nursing Care Plan The Child With A Major Burn InjuryDocument3 pagesNursing Care Plan The Child With A Major Burn InjuryPamela Soledad Delgado SuárezNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care PlanJess Fernandez BorgaNo ratings yet
- Pott's Disease NCPDocument7 pagesPott's Disease NCPkristel_nicole18yahoNo ratings yet
- Nursing Care PneumoniaDocument26 pagesNursing Care PneumoniaIsaac Kipkemoi100% (1)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument10 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationLean Ashly Tuddao Macarubbo0% (1)
- Nursing Care Plan PediaDocument7 pagesNursing Care Plan PediaYvonne Niña Aranton100% (1)
- Drug Study and NCPDocument10 pagesDrug Study and NCPRachel PerandoNo ratings yet
- Impact of Inflation On PovertyDocument5 pagesImpact of Inflation On PovertyVincent QuitorianoNo ratings yet
- Amanda McGuire ThesisDocument204 pagesAmanda McGuire ThesisVincent QuitorianoNo ratings yet
- Amanda McGuire ThesisDocument204 pagesAmanda McGuire ThesisVincent QuitorianoNo ratings yet
- Pneumonia and TuberculosisDocument18 pagesPneumonia and TuberculosisVincent QuitorianoNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care PlanVincent QuitorianoNo ratings yet
- John Aurel MDocument2 pagesJohn Aurel MVincent QuitorianoNo ratings yet
- Jam (Drug Study)Document11 pagesJam (Drug Study)Vincent QuitorianoNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care PlanVincent QuitorianoNo ratings yet
- Book ReportDocument1 pageBook ReportVincent QuitorianoNo ratings yet
- Patient CareDocument20 pagesPatient CareVincent QuitorianoNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care PlanVincent QuitorianoNo ratings yet
- Brain ShrinkDocument5 pagesBrain ShrinkVincent QuitorianoNo ratings yet
- Homily ReporyDocument1 pageHomily ReporyVincent QuitorianoNo ratings yet
- Changing Lifestyle BehaviorDocument23 pagesChanging Lifestyle BehaviorVincent QuitorianoNo ratings yet
- Drug Study and Mental Health AssessmentDocument8 pagesDrug Study and Mental Health AssessmentVincent Quitoriano100% (1)
- Disability EssayDocument7 pagesDisability Essayapi-459529771No ratings yet
- Microbial SafariDocument5 pagesMicrobial SafariClauu VargasNo ratings yet
- Cataract Consent FormDocument4 pagesCataract Consent FormHitesh Sharma100% (1)
- CASE STUDY 10 NCPDocument46 pagesCASE STUDY 10 NCPRosemarie R. Reyes100% (8)
- Eye LubricantDocument9 pagesEye LubricantbuddhahandNo ratings yet
- Syphilis: Jessica Lyons Period D STD Project 4/22/13Document3 pagesSyphilis: Jessica Lyons Period D STD Project 4/22/13jesssielynnn33No ratings yet
- Magic of The Minimum Dose PDFDocument221 pagesMagic of The Minimum Dose PDFminunat100% (1)
- A Detailed Lesson Plan Practical Research 2Document29 pagesA Detailed Lesson Plan Practical Research 2Erica CanonNo ratings yet
- Material Safety Data Sheet: 80W-90 Gear LubeDocument4 pagesMaterial Safety Data Sheet: 80W-90 Gear LubeFrank RodriguezNo ratings yet
- Final Warning A History of The New World Order by David Allen Rivera - SUMMARY / EXCERPTSDocument7 pagesFinal Warning A History of The New World Order by David Allen Rivera - SUMMARY / EXCERPTSKeith KnightNo ratings yet
- Difficult Airway AlgorithmDocument48 pagesDifficult Airway AlgorithmshikhaNo ratings yet
- Statistics Notes in The British Medical Journal (Bland JM, Altman DG. - NEJ)Document95 pagesStatistics Notes in The British Medical Journal (Bland JM, Altman DG. - NEJ)pegazus_arNo ratings yet
- NewFood 2015 Nr004Document88 pagesNewFood 2015 Nr004XavierNo ratings yet
- Transient Tachypnea of The Newborn (TTN)Document6 pagesTransient Tachypnea of The Newborn (TTN)Wivan Havilian DjohanNo ratings yet
- Palmer Et Al v. Amazon - Com Inc Et AlDocument41 pagesPalmer Et Al v. Amazon - Com Inc Et AlGeekWireNo ratings yet
- Cosmetology Library ResourcesDocument40 pagesCosmetology Library Resourcesemiliana magerusanNo ratings yet
- Lung Cancer Prediction Using Data Mining TechniquesDocument6 pagesLung Cancer Prediction Using Data Mining TechniquesKEZZIA MAE ABELLANo ratings yet
- Semey State Medical University: Department of Psychiatry Topic Schizophrenia Raja Ali HassanDocument45 pagesSemey State Medical University: Department of Psychiatry Topic Schizophrenia Raja Ali HassanRaja HassanNo ratings yet
- Probiotics, Prebiotics and The Gut Microbiota: Ilsi Europe Concise Monograph SeriesDocument40 pagesProbiotics, Prebiotics and The Gut Microbiota: Ilsi Europe Concise Monograph Seriesjimmy7forever100% (1)
- 1 s2.0 S0160412006000857 MainDocument10 pages1 s2.0 S0160412006000857 MainIsaac MotaungNo ratings yet
- Reproductive and Child Health ProgrammeDocument10 pagesReproductive and Child Health ProgrammeMebin NinanNo ratings yet
- Excretory Products and Their EliminationDocument6 pagesExcretory Products and Their Eliminationkanth3012No ratings yet
- Arcega ErlindaDocument7 pagesArcega ErlindaIvonne TernidaNo ratings yet
- MS LectureDocument5 pagesMS LectureAntoinette PeleñaNo ratings yet
- 9 Steps To Reverse DementiaDocument36 pages9 Steps To Reverse DementiaLavinia PirlogNo ratings yet
- Respiratory PhysiologyDocument16 pagesRespiratory PhysiologyYsabel Salvador DychincoNo ratings yet
- Assessment Dianosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Dianosis Planning Intervention Rationale Evaluationkyaw100% (1)
- 1 Title and SynopsisDocument11 pages1 Title and SynopsisMuhammad Arief ArdiansyahNo ratings yet
- Occupational HealthDocument8 pagesOccupational HealthFemale calm0% (1)
- Brief Notes Parish of St. RafaelDocument3 pagesBrief Notes Parish of St. RafaelAl F. Dela CruzNo ratings yet