Professional Documents
Culture Documents
Excretory Products and Their Elimination
Uploaded by
kanth3012Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Excretory Products and Their Elimination
Uploaded by
kanth3012Copyright:
Available Formats
CHAPTER
19
anand_mani16 Dr. Anand Mani https://www.anandmani.com https://discord.io/anandmani t.me/anandmani001
Excretion is the elimination of metabolic wastes like ammonia, urea, uric acid etc. from the tissues.
1. Ammonotelism: Process of excretion of NH3.
Ammonotelic animals: Aquatic invertebrates, aquatic insects,
bony fishes, aquatic amphibians etc.
o NH3 is highly toxic. So, excretion needs excess of water.
o NH3 is readily soluble in water and is excreted by diffusion
through body surface or gill surfaces (in fishes as
ammonium ions.
o Kidneys do not play any significant role in its removal.
2. Ureotelism: Process of excretion of urea.
Ureotelic animals: Cartilaginous fishes, terrestrial & semi-
aquatic amphibians (frogs, toads etc.), aquatic or semi- aquatic
reptiles (alligators, turtles), mammals etc. In liver,
o NH3 is converted into less toxic urea. So, it needs only
moderate quantity of water for excretion.
o Some amount of urea may be retained in the kidney matrix
of some animals to maintain a desired osmolarity.
3. Uricotelism: Process of excretion of uric acid. It is water
insoluble & less toxic. So, water is not needed for excretion.
Uricotelic animals: Insects, some land crustaceans, land snails,
terrestrial reptiles & birds.
o Ureotelism & uricotelism are needed for water conservation.
Protonephridia (flame cells): In Flatworms, rotifers, some annelids & cephalochordate. Protonephridia are primarily
for osmoregulation.
Nephridia: In Annelids. Help in the removal of nitrogenous wastes and osmoregulation.
Malpighian tubules: In Insects. Help in the removal of nitrogenous wastes and osmoregulation.
Antennal or green glands: In Crustaceans (prawn etc.)
Kidneys: In higher animals..
It includes kidneys, ureters, urinary bladder & urethra.
• Reddish brown, bean-shaped structures situated between the
levels of last thoracic & 3rd lumbar vertebra.
• Length: 10-12 cm, Width: 5-7 cm, Thickness: 2-3 cm. Average weight:
120-170 gm.
• It is enclosed in a tough, 3-layered fibrous renal capsule.
• On the concave side of kidney, there is an opening (hilum or hilus)
through which blood vessels, nerves, lymphatic ducts and ureter
enter the kidney.
• Hilum leads to funnel shaped cavity called renal pelvis with
projections called calyces.
anand_mani16 Dr. Anand Mani https://www.anandmani.com https://discord.io/anandmani t.me/anandmani001
• A kidney has outer cortex & inner medulla.
• Medulla has few conical projections called medullary pyramids (renal pyramids) projecting into the calyces.
• Cortex extends in between the medullary pyramids as renal columns (Columns of Bertini).
• Each kidney has nearly one million tubular nephrons.
• Nephrons are the structural & functional units of kidney.
• Each nephron has 2 parts: Glomerulus & Renal tubule.
• Glomerulus: A tuft of capillaries formed by afferent
arteriole (a fine branch of renal artery). Blood from
glomerulus is carried away by efferent arteriole.
• Renal tubule: It begins with a double walled cup-like
Bowman’s capsule which encloses the glomerulus.
Glomerulus + Bowman’s capsule = Malpighian body
• The tubule continues with proximal convoluted tubule
• (PCT), Henle’s loop & distal convoluted tubule (DCT).
• Henle’s loop is hairpin-shaped. It has descending and
ascending limbs.
• The DCTs of many nephrons open into a collecting duct.
Collecting duct extends from cortex to inner parts of
medulla. They converge and open into the renal pelvis through
medullary pyramids in the calyces.
• Malpighian body (Renal corpuscle), PCT and DCT are situated
in renal cortex. Loop of Henledips into medulla.
• The efferent arteriole forms a fine capillary network
(peritubular capillaries) around the renal tubule. A minute
vessel of this network runs parallel to Henle’s loop forming a
‘U’ shaped vasa recta.
1. Cortical nephrons (85%): In this, the Henle’s loop is short and extends only very little into the medulla. Vasa recta
is absent or highly reduced.
2. Juxtamedullary nephrons (15%): In this, Henle’s loop is long and runs deep into medulla. Vasa recta present.
3 processes: Glomerular filtration, reabsorption & secretion.
• The glomerular capillary blood pressure causes filtration of blood through 3 layers, i.e. endothelium of glomerular
blood vessels, epithelium of Bowman’s capsule & a basement membrane between these 2 layers.
• The epithelial cells (podocytes) of the Bowman’s capsule are arranged in an intricate manner leaving some minute
spaces called filtration slits (slit pores).
• Almost all constituents of the blood plasma except the proteins pass onto the lumen of the Bowman’s capsule.
anand_mani16 Dr. Anand Mani https://www.anandmani.com https://discord.io/anandmani t.me/anandmani001
• About 1100-1200 ml of blood is filtered by the kidneys per minute. It constitutes 1/5th of the blood pumped out by
each ventricle of the heart in a minute.
• The amount of the filtrate formed per minute is called Glomerular filtration rate (GFR).
• Normal GFR = 125 ml/minute, i.e., 180 litres/day.
• 180 litres of glomerular filtrate is produced daily. But about
99% of this is reabsorbed by the renal tubules.
• So normal volume of urine released is 1.5 litres.
• From the filtrate, glucose, amino acids, Na+, etc. are reabsorbed
actively and nitrogenous wastes are absorbed passively.
Passive reabsorption of water occurs in the initial segments
of the nephron.
• PCT reabsorbs most of the nutrients, and 70-80% of
electrolytes & water. Simple cuboidal brush border epithelium
of PCT increases surface area for reabsorption.
• In loop of Henle, minimum reabsorption takes place. It
maintains high osmolarity of medullary interstitial fluid. The
descending limb is permeable to water but almost
impermeable to electrolytes. This concentrates the filtrate. The
ascending limb is impermeable to water but allows transport
of electrolytes. So, the filtrate gets diluted.
• In DCT, conditional reabsorption of Na+ & water takes place.
• Collecting duct extends from cortex to inner parts of medulla. It reabsorbs large amount of water to concentrate
urine. It also allows passage of small amounts of urea into medullary interstitium to keep up the osmolarity.
• Cells of PCT & DCT maintain ionic (Na-K balance) and acid-base balance (pH) of body fluids by selective secretion
of H+, K+& NH3into the filtrate and absorption of HCO3- from it.
• Collecting duct maintain pH and ionic balance of blood by the secretion of H+ and K+ ions.
• Henle’s loop & vasa recta help to concentrate the urine.
• The flow of filtrate in the 2 limbs of Henle’s loop and
the flow of blood through the 2 limbs of vasa recta
are in
• opposite directions (i.e. in a counter current pattern).
• Due to the counter current and proximity between the
Henle’s loop & vasa recta, osmolarity increases from
cortex (300 mOsmolL-1) to the inner medullary
interstitium (1200 mOsmolL-1). This gradient is mainly
caused by NaCl and urea.
• NaCl is transported by ascending limb of Henle’s loop
that is exchanged with descending limb of vasa recta.
NaCl is returned to interstitium by ascending limb of
vasa recta.
anand_mani16 Dr. Anand Mani https://www.anandmani.com https://discord.io/anandmani t.me/anandmani001
• Similarly, small amount of urea enters the thin segment of the ascending limb of Henle’s loop which is
transported back to the interstitium by the collecting tubule.
• This transport of substances facilitated by Henle’s loop & vasa recta is called Counter current mechanism. It
maintains a concentration gradient (interstitial gradient) in medullary interstitium. It enables easy passage of
water from collecting tubule to concentrate the filtrate (urine).
• Human kidneys produce urine four times concentrated than the initial filtrate formed hereby decreases the blood
pressure.
• Gradual filling of urinary bladder causes stretching. As a result,
stretch receptors on its wall send impulses to CNS. The CNS
passes on motor messages. It causes the contraction of smooth
muscles of the bladder and simultaneous relaxation of the
urethral sphincter. It results in micturition (release of urine).
• The neural mechanism causing micturition is called micturition
reflex.
• An adult human excretes 1 to 1.5 litres of urine (25-30 gm urea) per
day.
• Urine is a light yellow coloured watery fluid, slightly acidic (pH-6.0)
and has a characteristic odour.
• Various conditions can affect the characteristics of urine.
• Analysis of urine helps in clinical diagnosis of many metabolic
disorders and malfunctioning of the kidney.
• E.g. Glycosuria (presence of glucose) and Ketonuria (ketone
bodies) in urine indicates diabetes mellitus.
1. Lungs: Remove CO2 (18 litres/day) and water.
2. Liver: Secretes bile containing bilirubin, biliverdin, cholesterol,
degraded steroid hormones, vitamins and drugs. Most of them pass
out along with digestive wastes.
3. Skin (Sweat glands & sebaceous glands): Sweat contains water, NaCl,
small amounts of urea, lactic acid, etc. Primary function of sweat is to
give a cooling effect on body surface. Sebaceous glands eliminate
sterols, hydrocarbons, waxes etc. through sebum. Sebum provides a
protective oily covering for the skin.. Saliva eliminates small amounts
of nitrogenous wastes.
- It is done by hormonal feedback mechanisms involving the hypothalamus, JGA and the heart.
- Changes in blood volume, body fluid volume and ionic concentration activate Osmoreceptors in the body.
• When body fluid level decreases, the osmoreceptors stimulate hypothalamus to release antidiuretic hormone
(ADH). It stimulates water reabsorption from DCT & collecting duct. Thus, ADH prevents diuresis and increases
body fluid volume. Increase in fluid volume switches off the osmoreceptors and suppresses ADH release to
complete the feedback.
• ADH constricts blood vessels resulting in an increase of BP. This increases the glomerular blood flow and GFR.
anand_mani16 Dr. Anand Mani https://www.anandmani.com https://discord.io/anandmani t.me/anandmani001
• JGA (Juxta glomerular apparatus) is a sensitive region formed by cellular modification of DCT and the afferent
arteriole at the location of their contact.
• JGA regulates the GFR.
• A fall in glomerular blood flow/glomerular blood pressure/GFR activates the JG cells to release renin.
• Renin converts angiotensinogen in blood to angiotensin 1 and further to angiotensin II (a vasoconstrictor).
• Angiotensin II performs the following functions:
• Increases glomerular blood pressure and thereby GFR.
• Activates adrenal cortex to release Aldosterone.
• Aldosterone causes reabsorption of Na+ and water from the distal parts of the tubule. This also leads to an
increase in blood pressure and GFR.
• ANF check on the renin- angiotensin mechanism.
• An increase in blood flow to the atria of the heart causes the release of Atrial Natriuretic Factor (ANF).
• ANF causes vasodilation (dilation of blood vessels) and thereby decreases the blood pressure.
• Uremia: Accumulation of urea in blood which may lead to kidney failure.
• Renal calculi: Stone or insoluble mass of crystallized salts (oxalates, etc.) formed within the kidney.
• Glomerulonephritits: Inflammation of glomeruli.
• In patients with uremia, urea is removed by hemodialysis.
• The dialyzing unit (artificial kidney) contains a coiled
cellophane tube surrounded by dialyzing fluid. It has same
composition of plasma except nitrogenous wastes.
• Blood drained from a convenient artery is pumped into
dialyzing unit after adding anticoagulant like heparin.
• The porous cellophane membrane of the tube allows the
passage of molecules based on concentration gradient.
• As nitrogenous wastes are absent in dialyzing fluid, these
substances freely move out, thereby clearing the blood.
• The cleared blood is pumped back to the body through a
vein after adding anti-heparin to it.
• It is the ultimate method in the correction of acute renal
failures. A functioning kidney is taken from a donor.
• It is better to receive kidney from a close relative to
minimize chances of rejection by immune system of host.
anand_mani16 Dr. Anand Mani https://www.anandmani.com https://discord.io/anandmani t.me/anandmani001
You might also like
- Vipin Sir Biology 19. Excretory Products and Their EliminationDocument55 pagesVipin Sir Biology 19. Excretory Products and Their EliminationvanshpatelssisNo ratings yet
- Renal Reflections: Exploring the Marvels of Nephrology: The Intricate Ballet of Kidney Functions UnveiledFrom EverandRenal Reflections: Exploring the Marvels of Nephrology: The Intricate Ballet of Kidney Functions UnveiledNo ratings yet
- Excretory Products and Their ElimnationDocument5 pagesExcretory Products and Their ElimnationSanskriti VermaNo ratings yet
- Kidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandKidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- EXCRETORY PRODUCTSDocument7 pagesEXCRETORY PRODUCTSSreeyansu RajNo ratings yet
- Chapter-19 Excretory Products and Their Elimnation: Forms of Nitrogen ExcretionsDocument8 pagesChapter-19 Excretory Products and Their Elimnation: Forms of Nitrogen Excretionsmaryak3050No ratings yet
- XQ WFHKLJW WWHAfu 0 DGWFDocument10 pagesXQ WFHKLJW WWHAfu 0 DGWFGiridharan & Balaji RNNo ratings yet
- Hafeezullah: Subject:Anatomy Topic: Anatomy of Excretory System Roll No: 15 Semester: 1 RepeaterDocument10 pagesHafeezullah: Subject:Anatomy Topic: Anatomy of Excretory System Roll No: 15 Semester: 1 RepeaterMuhammad ShahzaibNo ratings yet
- KidneyDocument85 pagesKidneyIshita SinghNo ratings yet
- Human Excretory System - Grade 11 & 12Document19 pagesHuman Excretory System - Grade 11 & 12Ishita SinghNo ratings yet
- Excretory Products and EliminationDocument48 pagesExcretory Products and EliminationDivya AgarawalNo ratings yet
- 11 Biology Notes ch19 Excretory Products and Their Elimination PDFDocument3 pages11 Biology Notes ch19 Excretory Products and Their Elimination PDFRamachandranPerumalNo ratings yet
- Excretory Products and their EliminationDocument7 pagesExcretory Products and their EliminationAjay JamwalNo ratings yet
- Selected Lecture Notes Chapter 25: The Urinary System: I. Kidney Functions and AnatomyDocument12 pagesSelected Lecture Notes Chapter 25: The Urinary System: I. Kidney Functions and AnatomyMarilia BonorinoNo ratings yet
- Excretion and OsmoregulationDocument33 pagesExcretion and OsmoregulationS S100% (1)
- 11 Biology Chapter 20.Document4 pages11 Biology Chapter 20.jackieaj093No ratings yet
- The Kidney: Hemanth P Dialysis Tutor B N Patel Institute of Paramedical & SciencesDocument46 pagesThe Kidney: Hemanth P Dialysis Tutor B N Patel Institute of Paramedical & SciencesHemanth PrakashNo ratings yet
- 6 Renal PhysiologyDocument37 pages6 Renal PhysiologyD TekNo ratings yet
- Chapter 19 Points To RememberDocument5 pagesChapter 19 Points To RememberSaksham YadavNo ratings yet
- Urine Formation - Human Excretory SystemDocument13 pagesUrine Formation - Human Excretory SystemRaj KumarNo ratings yet
- Excretion of WaterDocument5 pagesExcretion of WaterKamrul Alam MasumNo ratings yet
- Excretory Products and Their EliminationDocument13 pagesExcretory Products and Their Eliminationaravind kishanNo ratings yet
- الجهاز البولىDocument6 pagesالجهاز البولىNajwa AbdualgaderNo ratings yet
- Excretory Products and their Elimination: How Different Organisms Eliminate WastesDocument27 pagesExcretory Products and their Elimination: How Different Organisms Eliminate Wastesamit lakraNo ratings yet
- STUDY.STUDY.STUDY...princerenerperaDocument14 pagesSTUDY.STUDY.STUDY...princerenerperaPrince Rener Velasco Pera100% (1)
- Zoo 1 Excretion and OsmoregulationDocument17 pagesZoo 1 Excretion and OsmoregulationMaheshkumar KalalNo ratings yet
- ExcretiDocument22 pagesExcretinihalbolla2023No ratings yet
- Urinary SystemDocument28 pagesUrinary Systemgabanule brandonNo ratings yet
- Excretory SystemDocument55 pagesExcretory SystemBhargavi PriyaNo ratings yet
- Urinalysis and Body FluidsDocument54 pagesUrinalysis and Body FluidsabdishakurNo ratings yet
- BiologyNotesForClass11hChapter PDFDocument7 pagesBiologyNotesForClass11hChapter PDFNaresh BorkarNo ratings yet
- Final UrinarysystemDocument15 pagesFinal UrinarysystemPrabhjot KaurNo ratings yet
- Revision Notes: Excretory OrgansDocument4 pagesRevision Notes: Excretory Organskavitaruby1980No ratings yet
- Jigjiga University College of Veterinary Medicine: by DR Mahamud A. (DVM, MSC)Document56 pagesJigjiga University College of Veterinary Medicine: by DR Mahamud A. (DVM, MSC)Shemsu LoveNo ratings yet
- Anatomy and Physiology of KidneyDocument5 pagesAnatomy and Physiology of KidneyMaLik ZaKwan IwAnNo ratings yet
- Kidney Anatomy and PhysiologyDocument6 pagesKidney Anatomy and PhysiologyJohn Wilbert BirungNo ratings yet
- Unit 2 Urinary System, Educational PlatformDocument45 pagesUnit 2 Urinary System, Educational Platformneedo707070No ratings yet
- Anatomy and Physiology of The KidneysDocument21 pagesAnatomy and Physiology of The Kidneysccbrown750% (2)
- The Urinary System: Structure and Functions in 40 CharactersDocument30 pagesThe Urinary System: Structure and Functions in 40 CharactersRadia RaicyNo ratings yet
- Excretory Products and Their EliminationDocument9 pagesExcretory Products and Their EliminationBiju MylachalNo ratings yet
- Urinary System 1. List The Functions of The KidneysDocument6 pagesUrinary System 1. List The Functions of The KidneysheerNo ratings yet
- The Urinary SystemDocument51 pagesThe Urinary SystemmaoNo ratings yet
- Renal Physiology 1 170407164141Document76 pagesRenal Physiology 1 170407164141Vhutshilo MasithembiNo ratings yet
- Anatomy of The Excretory SystemDocument6 pagesAnatomy of The Excretory SystemCherry Grace Articulo DabuconNo ratings yet
- Sken D Blok 20 Kel 2 '17Document18 pagesSken D Blok 20 Kel 2 '17dewi fortuna agustiaNo ratings yet
- HomeostasisDocument10 pagesHomeostasisSiddhesh YadavNo ratings yet
- Renal Physiology: The Functions and Anatomy of the KidneysDocument88 pagesRenal Physiology: The Functions and Anatomy of the Kidneysfentaw melkieNo ratings yet
- Anatomy and Physiology-FinalDocument4 pagesAnatomy and Physiology-FinalSlyne CenarosaNo ratings yet
- Anatomy and Physiology of The KidneysDocument3 pagesAnatomy and Physiology of The KidneysNeil AlviarNo ratings yet
- Revision Notes Class 11 - Biology Chapter 19 - Excretory Product and Their EliminationDocument9 pagesRevision Notes Class 11 - Biology Chapter 19 - Excretory Product and Their EliminationHarpreetNo ratings yet
- 11 Biology Notes ch19 Excretory Products and Their Elimination 1Document4 pages11 Biology Notes ch19 Excretory Products and Their Elimination 1Sumanth SY 1119No ratings yet
- Unit - Ii Human Anatomy and PhysiologyDocument15 pagesUnit - Ii Human Anatomy and PhysiologyRK YeleswarapuNo ratings yet
- Review of AnaphysioDocument8 pagesReview of AnaphysioDizerine Mirafuentes RolidaNo ratings yet
- Excretory SystemDocument42 pagesExcretory Systemadedayoadeboye0107No ratings yet
- Renal Anatomy and PhysiologyDocument15 pagesRenal Anatomy and PhysiologySapna JainNo ratings yet
- Revision Notes On Excretory Products and Their Elimination For NEET 2023 - Free PDF DownloadDocument11 pagesRevision Notes On Excretory Products and Their Elimination For NEET 2023 - Free PDF Downloadtulsiram.op.69No ratings yet
- The Urinary System: Kidneys, Ureters, Bladder and UrethraDocument8 pagesThe Urinary System: Kidneys, Ureters, Bladder and UrethraanyaNo ratings yet
- Urinary SystemDocument10 pagesUrinary Systemapi-19824701No ratings yet
- Urinary SystemDocument48 pagesUrinary Systemnav_malhiNo ratings yet
- PT Test Planner Regular Medical 2022 23 FT Phase 02 Version 2 0Document2 pagesPT Test Planner Regular Medical 2022 23 FT Phase 02 Version 2 0kanth3012No ratings yet
- Concept Strengthening Sheet CSS 04 Based On AIATS 04 CF OYM ZoologyDocument4 pagesConcept Strengthening Sheet CSS 04 Based On AIATS 04 CF OYM Zoologykanth3012No ratings yet
- Part 2 15 QuesDocument2 pagesPart 2 15 Queskanth3012No ratings yet
- Cheat Codes-Physical ChemistryDocument34 pagesCheat Codes-Physical Chemistrykanth3012No ratings yet
- Environmental EducationDocument11 pagesEnvironmental Educationkanth3012No ratings yet
- Anemia in Heart Failure: A Review of Pathophysiology, Treatment Challenges and UnknownsDocument13 pagesAnemia in Heart Failure: A Review of Pathophysiology, Treatment Challenges and UnknownsHedya Nadhrati SururaNo ratings yet
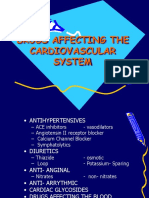
- CVS Drugs: Antihypertensives, Diuretics, Anti-AnginalsDocument21 pagesCVS Drugs: Antihypertensives, Diuretics, Anti-AnginalsAudrey Beatrice ReyesNo ratings yet
- HES 005 P2 Coverage and Drug Study GuideDocument4 pagesHES 005 P2 Coverage and Drug Study GuideXander Jake Asturias TangcalaganNo ratings yet
- LECTURE 4 - Major Intra - and Extracellular ElectrolytesDocument66 pagesLECTURE 4 - Major Intra - and Extracellular ElectrolytesGamotkoto PharmacyNo ratings yet
- Ascites Causes Diagnosis and TreatmentDocument24 pagesAscites Causes Diagnosis and TreatmentrifkaNo ratings yet
- A.H DIKKO's COMPLETED PROJECT WORK (Sept. 2019)Document76 pagesA.H DIKKO's COMPLETED PROJECT WORK (Sept. 2019)Abdulmalik DikkoNo ratings yet
- ESRD PathophysiologyDocument2 pagesESRD PathophysiologyMark Ronhel Gallardo PerenalNo ratings yet
- NCERT Solutions For Class 11 Biology Chapter 19: Excretory Products and Their Elimination Class 11Document6 pagesNCERT Solutions For Class 11 Biology Chapter 19: Excretory Products and Their Elimination Class 11AlfaazNo ratings yet
- NCP For HypertensionDocument4 pagesNCP For HypertensionCiariz Charisse83% (6)
- Review FisiologíaDocument112 pagesReview FisiologíaDiego Bustamante HeinsohnNo ratings yet
- Group 3 Cardiovascular System Complete HandoutDocument65 pagesGroup 3 Cardiovascular System Complete HandoutNicole LantinNo ratings yet
- Electrolyte and Acid Base DisordersDocument46 pagesElectrolyte and Acid Base DisordersMia ValdesNo ratings yet
- Water Homeostasis: Benjamin/Cummings Publishing CoDocument11 pagesWater Homeostasis: Benjamin/Cummings Publishing CoDawlat SalamaNo ratings yet
- Biochemistry Basic Science MCQsDocument26 pagesBiochemistry Basic Science MCQsSidharta Chatterjee50% (2)
- Badyal, 2003 - Animal Models of Hypertension and Effect of DrugsDocument14 pagesBadyal, 2003 - Animal Models of Hypertension and Effect of DrugsHo Yoke MeiNo ratings yet
- MSU-IIT student drug study on Tekturna (AliskirenDocument2 pagesMSU-IIT student drug study on Tekturna (AliskirenLIEZEL GRACE VELAYONo ratings yet
- Kent Scientific Whitepaper Explains Benefits of Non-Invasive Blood Pressure MonitoringDocument12 pagesKent Scientific Whitepaper Explains Benefits of Non-Invasive Blood Pressure MonitoringMuhammadSajjadSarwarNo ratings yet
- ABSITE CH 16 Critical CareDocument11 pagesABSITE CH 16 Critical CareJames JosephNo ratings yet
- Endocrine Passmedicine & Onexamination Notes 2016 PDFDocument96 pagesEndocrine Passmedicine & Onexamination Notes 2016 PDFsepan abdullahNo ratings yet
- Mtap421 ElectrolytesDocument9 pagesMtap421 ElectrolytesNhelomar ManlinconNo ratings yet
- Homeostasis and ExcretionDocument35 pagesHomeostasis and ExcretionronaldwepukhuluNo ratings yet
- A CARE STUDY HypertensionDocument48 pagesA CARE STUDY Hypertensionjeff_jj2000209790% (10)
- 9 Nephrology High YieldDocument144 pages9 Nephrology High YieldTawhid ZihadNo ratings yet
- Drugs Affecting Renin-Angiotensin SystemDocument36 pagesDrugs Affecting Renin-Angiotensin SystempradeephdNo ratings yet
- Excretion and Osmoregulation-2Document120 pagesExcretion and Osmoregulation-2S SNo ratings yet
- Recall March 2023Document19 pagesRecall March 2023Kazi Israt JahanNo ratings yet
- ChaptersDocument139 pagesChaptersDark PrincessNo ratings yet
- Blood Pressure Regulation - SlidesDocument35 pagesBlood Pressure Regulation - Slidesمحمد السنجلاويNo ratings yet
- Diabetes Mellitus and Hypertension Management in Clinical PracticesDocument37 pagesDiabetes Mellitus and Hypertension Management in Clinical PracticesSetyo PrabowoNo ratings yet
- 18 TH Course SyllabusDocument1,744 pages18 TH Course SyllabusxtineNo ratings yet
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessFrom Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessRating: 4 out of 5 stars4/5 (33)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionFrom EverandThe Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionRating: 4 out of 5 stars4/5 (811)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Tales from Both Sides of the Brain: A Life in NeuroscienceFrom EverandTales from Both Sides of the Brain: A Life in NeuroscienceRating: 3 out of 5 stars3/5 (18)
- All That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesFrom EverandAll That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesRating: 4.5 out of 5 stars4.5/5 (397)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4.5 out of 5 stars4.5/5 (4)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceFrom EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceRating: 4.5 out of 5 stars4.5/5 (515)
- The Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindFrom EverandThe Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindRating: 4.5 out of 5 stars4.5/5 (93)
- The Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorFrom EverandThe Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorNo ratings yet
- A Series of Fortunate Events: Chance and the Making of the Planet, Life, and YouFrom EverandA Series of Fortunate Events: Chance and the Making of the Planet, Life, and YouRating: 4.5 out of 5 stars4.5/5 (62)
- Who's in Charge?: Free Will and the Science of the BrainFrom EverandWho's in Charge?: Free Will and the Science of the BrainRating: 4 out of 5 stars4/5 (65)
- Wayfinding: The Science and Mystery of How Humans Navigate the WorldFrom EverandWayfinding: The Science and Mystery of How Humans Navigate the WorldRating: 4.5 out of 5 stars4.5/5 (18)
- Undeniable: How Biology Confirms Our Intuition That Life Is DesignedFrom EverandUndeniable: How Biology Confirms Our Intuition That Life Is DesignedRating: 4 out of 5 stars4/5 (11)
- Why We Sleep: Unlocking the Power of Sleep and DreamsFrom EverandWhy We Sleep: Unlocking the Power of Sleep and DreamsRating: 4.5 out of 5 stars4.5/5 (2083)
- Good Without God: What a Billion Nonreligious People Do BelieveFrom EverandGood Without God: What a Billion Nonreligious People Do BelieveRating: 4 out of 5 stars4/5 (66)
- Buddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomFrom EverandBuddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomRating: 4 out of 5 stars4/5 (215)
- Human: The Science Behind What Makes Your Brain UniqueFrom EverandHuman: The Science Behind What Makes Your Brain UniqueRating: 3.5 out of 5 stars3.5/5 (38)
- Fast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperFrom EverandFast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperRating: 4.5 out of 5 stars4.5/5 (15)
- Crypt: Life, Death and Disease in the Middle Ages and BeyondFrom EverandCrypt: Life, Death and Disease in the Middle Ages and BeyondRating: 4 out of 5 stars4/5 (3)
- The Lives of Bees: The Untold Story of the Honey Bee in the WildFrom EverandThe Lives of Bees: The Untold Story of the Honey Bee in the WildRating: 4.5 out of 5 stars4.5/5 (44)
- This Is Your Brain On Parasites: How Tiny Creatures Manipulate Our Behavior and Shape SocietyFrom EverandThis Is Your Brain On Parasites: How Tiny Creatures Manipulate Our Behavior and Shape SocietyRating: 3.5 out of 5 stars3.5/5 (31)
- Lymph & Longevity: The Untapped Secret to HealthFrom EverandLymph & Longevity: The Untapped Secret to HealthRating: 4.5 out of 5 stars4.5/5 (13)
- Inside of a Dog: What Dogs See, Smell, and KnowFrom EverandInside of a Dog: What Dogs See, Smell, and KnowRating: 4 out of 5 stars4/5 (390)