Professional Documents
Culture Documents
Pelvis and Perineum Clinical Correlation
Uploaded by
Keesha Mariel AlimonCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pelvis and Perineum Clinical Correlation
Uploaded by
Keesha Mariel AlimonCopyright:
Available Formats
PELVIS & PERINEUM CLINICAL CORRELATIONS | 3B
CACAO | CIONELO | GONZALES | ICARO | JIMENEZ | SARILE | TARROBAL | TENORIO
BONY PELVIS VS PELVIC GIRDLE
BONY PELVIS
Composed of four bones namely the sacrum, coccyx and two innominate bones (fusion of the ilium, ischium and pubis) Joined by sacroiliac synchondroses to the sacrum and to one another at the symphysis pubis -
PELVIC GIRDLE
Contains the coxial bone containing the ischium, pubis and their relative components The pelvis contains both coxal bone components and sacrum and coccyx Serves as an attachment of the lower limbs to the axial skeleton
BOUNDARIES OF PELVIC INLET AND PELVIC OUTLET
PELVIC INLET
ANTERIOR: Pubic Crest of Pubic Symphysis POSTERIOR: anterior margin of the base of the sacrum (or the Ala of thesacrum) and sacrovertebral angle (or sacral promontory) LATERAL: iliopectineal line (Arcuate line + Pecten Pubis)
PELVIC OUTLET
ANTERIOR: Pubic Arch LATERAL: Ischial Tuberosities POSTEROLATERAL: inferior margin of the sacrotuberous ligament POSTERIOR: tip of the Coccyx
FALSE PELVIS VS TRUE PELVIS
FALSE PELVIS
Aka Greater Pelvis Expanded portion above and in front of pelvic brim - Above the pelvic inlet - has ilia on the side - incomplete in the front, with a wide interval between anterior borders of ilia - bounded by vertebra posteriorly - supports abdominal contents - after first trimester, supports gravid uterus (in females)
TRUE PELVIS
- aka Lesser Pelvis - below and behind the pelvic brim - between the pelvic inlet and pelvic outlet bones are more complete compared to false pelvis - bounded by ischium and pubis, laterally and anteriorly - bounded by sacrum and coccyx posteriorly - internal borders are solid and immobile - posterior wall is twice the anterior wall
PELVIMETRY
the process of measuring the dimensions and capacity of the pelvis, especially of the adult female pelvis the diameter of the osseous birth canal are compared with that of the infants head to determine whether the pelvis is of sufficient diameter to allow normal vaginal delivery - used in leading the decision of natural, operative vaginal delivery or conducting a Caesarean section
PERINEUM
- area of tissue that marks externally the approximate boundary of the outlet of the pelvis and gives passage to the urogenital ducts and rectum - area between the anus and the posterior part of the external genitalia - diamond shaped region demarcated by four angles: anteriorly by the symphysis pubis, posteriorly by the tip of the coccyx and laterally by the two ischial tuberosities - divided into two triangles by a line joining the two ischial tuberosities, these are the urogenital triangle anteriorly and anorectal triangle posteriorly
BORDERS OF THE UROGENITAL AND ANAL TRIANGLE
UROGENITAL TRIANGLE
ANTERIORLY Pubic Symphysis POSTERIORLY line joining the ischial tuberosities and perineal body LATERALLY Pubic Arch
ANAL TRIANGLE
ANTERIORLY - Perineal membrabe POSTEROLATERALLY Sacrotuberous membrabe
PERINEAL BODY
- central tendon of the perineum - pyramidal fibromuscular mass situated in the middle of the junction of urogenital triangle and anal triangle - In males, it is found between the bulb of the penis and the anus, while in females, it is found between the vagina and the anus. - essential for the integrity of the pelvic floor, especially in females. It provides attachment to the following muscles: - External anal sphincter muscle - Bulbospongiosus muscle - Superficial transverse perineal muscle - Levator ani muscle (anterior fibers) - External urinary sphincter - Deep transverse perineal muscle
ANORECTAL FISTULA AND GOODSALLS RULE
Anorectal Fistula - Also known as fistula-in-ano, this is an abnormal communication between the anus and the perianal skin, thus creating a passageway for spread of infection from the surrounding anal glands into the intramuscular spaces. It can occur spontaneously, or secondary to perianal or perirectal abscess. It may also be secondary to trauma, Crohns disease, anal fissures, carcinoma, radiation therapy, actinomycoses, or chlamydial infections. Types 1. Transsphincteric fistulae are the result of ischiorectal abscesses, with extension of the tract through the external sphincter. Account for about 25% of all fistulae. 2. Intersphincteric fistulae are confined to the intersphincteric space and internal sphincter. They result from perianal abscesses. Account for about 70% of all fistulae.
3. Suprasphincteric fistulae are the result of supralevator abscesses. They pass through the levator ani muscle, over the top of the puborectalis muscle, and into the intersphincteric space. Account for about 5% of all fistulae.
4. Extrasphincteric fistulae bypass the anal canal and sphincter mechanism, passing through the ischiorectal fossa and levator ani muscle, and open high in the rectum. Accounts for about only 1% of all fistulae. Goodsalls Rule - This rule is used to predict the direction of the extent of the fistula based on its origin. If the patient is in lithotomy position, it states that: If the external opening is anterior to an imaginary line drawn horizontally through the anal canal, the fistula usually runs directly into the anal canal. If the external opening is posterior to the line, the fistula usually curves to the posterior midline of the anal canal. However, it must be noted that: the further away the external opening is from the anus, the less reliable Goodsall's rule becomes. Additionally, the trajectory of a complex fistula is unpredictable.
CALDWELL-MOLLOY PELVIC CLASSIFICATION OF PELVIS
PELVIS TYPE
-
DESCRIPTION
Appears in 50% of the population It is the normal female type. Inlet is slightly transverse oval. Sacrum is wide with average concavity and inclination. Side walls are straight with blunt ischial spines. Sacro-sciatic notch is wide. Subpubic angle is 90-100 25% occurrence It is ape-like type. All anteroposterior diameters are long. All transverse diameters are short. Sacrum is long and narrow. Sacro-sciatic notch is wide. Subpubic angle is narrow. 20% occurence It is a male type. Inlet is triangular or heartshaped with anterior narrow apex. Side walls are converging (funnel pelvis) with projecting ischial spines. Sacro-sciatic notch is narrow. Subpubic angle is narrow <90 Least common type (5%) It is a flat female type. All anteroposterior diameters are short. All transverse diameters are long. Sacro-sciatic notch is narrow. Subpubic angle is wide.
IMAGE
GYNECOID PELVIS
ANTHROPOID PELVIS
ANDROID PELVIS
PLATYPELLOID PELVIS
PELVIC DIAMETERS AND CONJUGATES
Pelvic Diameters Normal Values
(AP) Anatomic (AP)Obstetric (AP)Diagonal Transverse Oblique 11.0 cm 10.0 cm 12.0 cm 13.0 cm 13.0 cm
INLET
Pelvic Diameters
Normal Values
AP Transverse AP Transverse (Bispinous) 12.75 cm 12.5 cm 12.0 cm 9.5-10.0 cm
MIDPLANE OUTLET
Parameters
Ischial Spines Pelvic Side Walls Concavity of Sacrum Sacrosciatic Notch Biischial Diameter of Outlet
Greatest Dimension Least Dimension
Pelvic Diameters
(AP) Anatomic (AP) Obstetric Transverse (Biischial)
Normal Values
9.5-11.5 cm 11.5 cm 11.0 cm
PARAMETERS IN CLINICAL ASSESSMENT OF THE MIDPELVIS
Normal
Blunt Divergent Concave/Deep Wide >8cm
Contracted
Prominent Convergent Shallow/Flat Narrow <8cm
You might also like
- Abdominal Wall, Omentum, Mesentery, Retroperitoneum Anatomy and ConditionsDocument6 pagesAbdominal Wall, Omentum, Mesentery, Retroperitoneum Anatomy and ConditionsMon Ordona De GuzmanNo ratings yet
- Essential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsDocument5 pagesEssential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsRika Ariyanti SaputriNo ratings yet
- SYPHYLISDocument1 pageSYPHYLISkhadzxNo ratings yet
- NSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saDocument19 pagesNSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saAhmed HossamNo ratings yet
- Chronic Inflammatory Dermatoses Inflammatory Blistering DisordersDocument4 pagesChronic Inflammatory Dermatoses Inflammatory Blistering DisordersspringdingNo ratings yet
- MCB 252 Final Exam Study GuideDocument62 pagesMCB 252 Final Exam Study GuideJay ZNo ratings yet
- NephroticDocument8 pagesNephroticsangheetaNo ratings yet
- Skin Structure and Function GuideDocument10 pagesSkin Structure and Function GuideyassrmarwaNo ratings yet
- Patho CA - Acute PancreatitisDocument1 pagePatho CA - Acute PancreatitisKNo ratings yet
- Non-Pathogenic Intestinal Amoebae Cyst MorphologyDocument2 pagesNon-Pathogenic Intestinal Amoebae Cyst MorphologyCoy NuñezNo ratings yet
- Renal SyndromeDocument13 pagesRenal SyndromeAndreas KristianNo ratings yet
- Nephrotic Syndrome WikipediaDocument10 pagesNephrotic Syndrome WikipediaJohn KevlarNo ratings yet
- Goljan Notes on Oxygen Transport and Tissue HypoxiaDocument5 pagesGoljan Notes on Oxygen Transport and Tissue HypoxiaDaniyal AzmatNo ratings yet
- Histo Review 2Document13 pagesHisto Review 2Coy NuñezNo ratings yet
- Identify viscus from histological featuresDocument1 pageIdentify viscus from histological featuresNaser Hamdi ZalloumNo ratings yet
- Inguinal CanalDocument4 pagesInguinal CanalspiraldaoNo ratings yet
- Anatomy Formative Preview of Thorax and BackDocument22 pagesAnatomy Formative Preview of Thorax and Backmvs hardhikNo ratings yet
- 5 Cyto AbnormalDocument9 pages5 Cyto AbnormalMerli Ann Joyce CalditoNo ratings yet
- Kidney Physiology (Q & A)Document28 pagesKidney Physiology (Q & A)ramadan100% (1)
- Upper and Lower Limb NervesDocument6 pagesUpper and Lower Limb NervesTaimoor DogarNo ratings yet
- 1 Ana Intro Finals September 16 LaygoDocument3 pages1 Ana Intro Finals September 16 LaygombdelenaNo ratings yet
- Abdominal Pain ExplainedDocument4 pagesAbdominal Pain ExplainedNazmun LailahNo ratings yet
- Cytogenetics Basics: Chromosomes, Analysis & AbnormalitiesDocument11 pagesCytogenetics Basics: Chromosomes, Analysis & Abnormalitiesjo_jo_mania100% (1)
- VQ - O2 GradientDocument27 pagesVQ - O2 GradientIkbal NurNo ratings yet
- PancreasDocument35 pagesPancreasPaskalisNo ratings yet
- Cytogenetics Note PDFDocument14 pagesCytogenetics Note PDFMerjema Bahtanović100% (1)
- Actinic Keratosis: (Aka Bowen's Disease)Document5 pagesActinic Keratosis: (Aka Bowen's Disease)fadoNo ratings yet
- Cytogenetics Course Module at AMYA Polytechnic CollegeDocument29 pagesCytogenetics Course Module at AMYA Polytechnic Collegeanonymous squashNo ratings yet
- Anterior Abdominal Wall Surgery InsightsDocument5 pagesAnterior Abdominal Wall Surgery InsightsAnonymous 2TzM1ZNo ratings yet
- Pathology B - Gastrointestinal Tract (Esguerra, 2015)Document18 pagesPathology B - Gastrointestinal Tract (Esguerra, 2015)Ars MoriendiNo ratings yet
- Kidney NewDocument4 pagesKidney NewParth BhayanaNo ratings yet
- 2011 07 Microbiology Mycobacterium Skin InfectionDocument6 pages2011 07 Microbiology Mycobacterium Skin InfectionCristinaConcepcionNo ratings yet
- General Features of The Immune SystemDocument6 pagesGeneral Features of The Immune SystemMinerva Bautista RoseteNo ratings yet
- Respiratory Notes (Chris Andersen, ICUPrimaryPrep - Com)Document14 pagesRespiratory Notes (Chris Andersen, ICUPrimaryPrep - Com)PkernNo ratings yet
- Cycle CellDocument16 pagesCycle CellRohingya EnglishNo ratings yet
- Abdominal OrgansDocument28 pagesAbdominal OrgansRS BuenavistaNo ratings yet
- Diaphragm Gross AnatomyDocument3 pagesDiaphragm Gross AnatomyCoy NuñezNo ratings yet
- Respiratory Drugs: An Overview of Medications for Lung ConditionsDocument117 pagesRespiratory Drugs: An Overview of Medications for Lung ConditionsjavibruinNo ratings yet
- Anastomosis Left Anterior Cerebral Artery BlockageDocument5 pagesAnastomosis Left Anterior Cerebral Artery BlockagemcwnotesNo ratings yet
- Pathology B - Gastrointestinal Tract (Esguerra, 2015) PDFDocument18 pagesPathology B - Gastrointestinal Tract (Esguerra, 2015) PDFJem QuintoNo ratings yet
- Nephrotic Nephritic SyndromsDocument4 pagesNephrotic Nephritic SyndromsKimiwari100% (2)
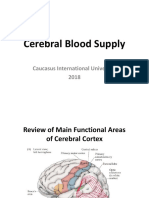
- Cerebral Blood FlowDocument39 pagesCerebral Blood FlowRajat ThakurNo ratings yet
- Handouts Integumentary Sys Sp11 B201Document7 pagesHandouts Integumentary Sys Sp11 B201Kelly TrainorNo ratings yet
- Thorax and LungsDocument2 pagesThorax and LungsHNo ratings yet
- Structural Biology of HIVDocument31 pagesStructural Biology of HIVLaura TapiaNo ratings yet
- Anat 6.3 GSA Appendix - EsguerraDocument4 pagesAnat 6.3 GSA Appendix - Esguerralovelots1234No ratings yet
- The Immune System DefencesDocument6 pagesThe Immune System DefencesKa-Shun Leung100% (1)
- Nose & Paranasal Sinuses 2018Document63 pagesNose & Paranasal Sinuses 2018yasrul izadNo ratings yet
- Brainstem NucleiDocument9 pagesBrainstem Nucleiankur_1No ratings yet
- Cardio Block 3Document62 pagesCardio Block 3Maya LaPradeNo ratings yet
- Arterial Blood Gas Workshop Dr. Lanzona 12.06.07: Lala 3C-Med-09 1Document4 pagesArterial Blood Gas Workshop Dr. Lanzona 12.06.07: Lala 3C-Med-09 1pramastutiNo ratings yet
- GI Anatomy & EmbryoDocument19 pagesGI Anatomy & EmbryoMaya LaPradeNo ratings yet
- CerebellumDocument14 pagesCerebellumapi-508474347No ratings yet
- Immune System Review QuestionsDocument2 pagesImmune System Review Questionsapi-521773978No ratings yet
- Normal Anatomy and Physiology of Female PelvisDocument58 pagesNormal Anatomy and Physiology of Female PelvisVic RobovskiNo ratings yet
- Assignment5 - Female PelvisDocument8 pagesAssignment5 - Female PelvisMahenurNo ratings yet
- Anatomy of The Female Reproductive SystemDocument41 pagesAnatomy of The Female Reproductive SystemMahad Maxamed AxmedNo ratings yet
- RA Y2 NotesDocument156 pagesRA Y2 NotesharshaNo ratings yet
- Inguinal Hernias: Trix M. Asuncion M.D. General SurgeryDocument55 pagesInguinal Hernias: Trix M. Asuncion M.D. General Surgeryjitendra magarNo ratings yet
- The female pelvis and fetal skull dimensionsDocument36 pagesThe female pelvis and fetal skull dimensionsHayder MuthanaNo ratings yet
- Histo Urinary SystemDocument10 pagesHisto Urinary SystemKeesha Mariel AlimonNo ratings yet
- Gross Lab ReproDocument8 pagesGross Lab ReproKeesha Mariel AlimonNo ratings yet
- FIADocument2 pagesFIAKeesha Mariel AlimonNo ratings yet
- HL7Document1 pageHL7Keesha Mariel AlimonNo ratings yet
- BUBUT ManuscriptDocument17 pagesBUBUT ManuscriptKeesha Mariel AlimonNo ratings yet
- What Is CopdDocument3 pagesWhat Is CopdReyna Marie EsuerteNo ratings yet
- HospiceDocument19 pagesHospiceKeesha Mariel AlimonNo ratings yet
- AMEE 2023 Final Programme OverviewDocument2 pagesAMEE 2023 Final Programme OverviewMohamed IshagNo ratings yet
- MASTER Unannounced Inspection ChecklistDocument13 pagesMASTER Unannounced Inspection ChecklistM Zeeshan AnsariNo ratings yet
- Unit 4 BacteriologyDocument51 pagesUnit 4 BacteriologySharmila LamisharNo ratings yet
- LearnEnglish Reading B2 A Plastic Ocean A Film ReviewDocument5 pagesLearnEnglish Reading B2 A Plastic Ocean A Film ReviewSerly FimasariNo ratings yet
- Vanessa Tarot BookletDocument36 pagesVanessa Tarot BookletClassic Bobby100% (2)
- KOICA-Yonsei Master's Program in Infectious Disease ControlDocument28 pagesKOICA-Yonsei Master's Program in Infectious Disease ControlBIDAN KSANo ratings yet
- Guideline Mood Australia New Zeland PDFDocument120 pagesGuideline Mood Australia New Zeland PDFFábio C NetoNo ratings yet
- Catheterization ChecklistDocument3 pagesCatheterization ChecklistAlthea Aubrey AgbayaniNo ratings yet
- Verification of Conformity Safety Consideration For Radio Equipment DirectiveDocument1 pageVerification of Conformity Safety Consideration For Radio Equipment DirectiveThắng CòiNo ratings yet
- ImplantsDocument11 pagesImplantsraheelNo ratings yet
- Definition of Sexual Abuse of ChildrenDocument2 pagesDefinition of Sexual Abuse of ChildrenRadhika RathoreNo ratings yet
- Coping Strategies of Athletes for Competitive AnxietyDocument13 pagesCoping Strategies of Athletes for Competitive AnxietyHONEY JEAN ESPENORIONo ratings yet
- The ABO Blood Groups: Phenotypes GenotypesDocument2 pagesThe ABO Blood Groups: Phenotypes GenotypesSheila Mae CabahugNo ratings yet
- Cardiac MarkersDocument23 pagesCardiac MarkersAsmaaYLNo ratings yet
- Grade 7 (TLE) Week 1Document12 pagesGrade 7 (TLE) Week 1RoswlleNo ratings yet
- Ingles: Estudiante Harold Andrés Bonett SánchezDocument8 pagesIngles: Estudiante Harold Andrés Bonett SánchezAndrès BonettNo ratings yet
- "Classic" Technique Guide: Niti Rotary Instrumentation SystemDocument12 pages"Classic" Technique Guide: Niti Rotary Instrumentation SystemdrnikhilbobadeNo ratings yet
- Acetabular and Hip FractureDocument133 pagesAcetabular and Hip FractureJuanita HenryNo ratings yet
- AA PamphletDocument52 pagesAA PamphletCarmen UleiaNo ratings yet
- Planning and Design of A Cell and Tissue Culture Laboratory: Christopher B. MorrisDocument2 pagesPlanning and Design of A Cell and Tissue Culture Laboratory: Christopher B. MorrisSubaNo ratings yet
- Single/ Exam Zone Centre DetailsDocument5 pagesSingle/ Exam Zone Centre DetailsHarsh AroraNo ratings yet
- Argumentative Essay (Yasmin Claire T. Navarro)Document2 pagesArgumentative Essay (Yasmin Claire T. Navarro)Yasmin Claire NavarroNo ratings yet
- Analytical Exposition Text Corona Should Be Against Surround UsDocument2 pagesAnalytical Exposition Text Corona Should Be Against Surround UsRifkyNo ratings yet
- Middle Childhood Physical Development (6-11 YearsDocument13 pagesMiddle Childhood Physical Development (6-11 YearsAngela YlaganNo ratings yet
- PALLIATIVE CARE SYMPTOM MANAGEMENTDocument153 pagesPALLIATIVE CARE SYMPTOM MANAGEMENTrlinao100% (3)
- Diuretics MOA, Examples, Effects, and Nursing ConsiderationsDocument1 pageDiuretics MOA, Examples, Effects, and Nursing ConsiderationsGrace ButlerNo ratings yet
- SolidtumorsinchildrenDocument24 pagesSolidtumorsinchildrenPriyaNo ratings yet
- Grade 4 WINS OrientationDocument2 pagesGrade 4 WINS OrientationChristine FranciscoNo ratings yet
- Aiapget 2020 QPDocument29 pagesAiapget 2020 QPGanesh RadhakrishnanNo ratings yet
- Slide PPT PrismaDocument31 pagesSlide PPT PrismaUlul Azmi AdnanNo ratings yet
- You Can't Joke About That: Why Everything Is Funny, Nothing Is Sacred, and We're All in This TogetherFrom EverandYou Can't Joke About That: Why Everything Is Funny, Nothing Is Sacred, and We're All in This TogetherNo ratings yet
- Other People's Dirt: A Housecleaner's Curious AdventuresFrom EverandOther People's Dirt: A Housecleaner's Curious AdventuresRating: 3.5 out of 5 stars3.5/5 (104)
- The Importance of Being Earnest: Classic Tales EditionFrom EverandThe Importance of Being Earnest: Classic Tales EditionRating: 4.5 out of 5 stars4.5/5 (43)
- The House at Pooh Corner - Winnie-the-Pooh Book #4 - UnabridgedFrom EverandThe House at Pooh Corner - Winnie-the-Pooh Book #4 - UnabridgedRating: 4.5 out of 5 stars4.5/5 (5)
- The Asshole Survival Guide: How to Deal with People Who Treat You Like DirtFrom EverandThe Asshole Survival Guide: How to Deal with People Who Treat You Like DirtRating: 4 out of 5 stars4/5 (60)
- Welcome to the United States of Anxiety: Observations from a Reforming NeuroticFrom EverandWelcome to the United States of Anxiety: Observations from a Reforming NeuroticRating: 3.5 out of 5 stars3.5/5 (10)
- The Inimitable Jeeves [Classic Tales Edition]From EverandThe Inimitable Jeeves [Classic Tales Edition]Rating: 5 out of 5 stars5/5 (3)
- The Best Joke Book (Period): Hundreds of the Funniest, Silliest, Most Ridiculous Jokes EverFrom EverandThe Best Joke Book (Period): Hundreds of the Funniest, Silliest, Most Ridiculous Jokes EverRating: 3.5 out of 5 stars3.5/5 (4)
- Sexual Bloopers: An Outrageous, Uncensored Collection of People's Most Embarrassing X-Rated FumblesFrom EverandSexual Bloopers: An Outrageous, Uncensored Collection of People's Most Embarrassing X-Rated FumblesRating: 3.5 out of 5 stars3.5/5 (7)
- The Book of Bad:: Stuff You Should Know Unless You’re a PussyFrom EverandThe Book of Bad:: Stuff You Should Know Unless You’re a PussyRating: 3.5 out of 5 stars3.5/5 (3)
- Killing the Guys Who Killed the Guy Who Killed Lincoln: A Nutty Story About Edwin Booth and Boston CorbettFrom EverandKilling the Guys Who Killed the Guy Who Killed Lincoln: A Nutty Story About Edwin Booth and Boston CorbettRating: 4.5 out of 5 stars4.5/5 (339)
- Humorous American Short Stories: Selections from Mark Twain, O. Henry, James Thurber, Kurt Vonnegut, Jr. and moreFrom EverandHumorous American Short Stories: Selections from Mark Twain, O. Henry, James Thurber, Kurt Vonnegut, Jr. and moreNo ratings yet
- 100 Bible Verses Everyone Should Know by HeartFrom Everand100 Bible Verses Everyone Should Know by HeartRating: 4.5 out of 5 stars4.5/5 (20)
- Tidy the F*ck Up: The American Art of Organizing Your Sh*tFrom EverandTidy the F*ck Up: The American Art of Organizing Your Sh*tRating: 4.5 out of 5 stars4.5/5 (99)











































































































![The Inimitable Jeeves [Classic Tales Edition]](https://imgv2-1-f.scribdassets.com/img/audiobook_square_badge/711420909/198x198/ba98be6b93/1712018618?v=1)