Professional Documents
Culture Documents
Volume 13, Issue 2, August 2012 - Helicobacter Pylori Infection in Superficial Gastritis, Erosive Gastritis and Gastric Ulcer
Uploaded by
mzdanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Volume 13, Issue 2, August 2012 - Helicobacter Pylori Infection in Superficial Gastritis, Erosive Gastritis and Gastric Ulcer
Uploaded by
mzdanCopyright:
Available Formats
The Indonesian Journal of Gastroenterology, Hepatology and Digestive Endoscopy 74
ORIGINAL ARTICLE
Helicobacter pylori Infection in Superfcial
Gastritis, Erosive Gastritis and Gastric Ulcer
Jacobus Albertus*, Abdul Aziz Rani**, Marcellus Simadibrata**
Murdani Abdullah**, Ari Fahrial Syam**
*Department of Internal Medicine, Tugurejo District General Hospital, Semarang
**Division of Gastroenterology, Department of Internal Medicine, Faculty of Medicine
University of Indonesia/Dr. Cipto Mangunkusumo General National Hospital, Jakarta
ABSTRACT
Background: Helicobacter pylori (H. pylori) infection leads to infammation of the gastric mucosa.
It damages the gastric epithelium and related to the risk of developing gastric cancer. Over time, it may develop into
the development of glandular atrophy and intestinal metaplasia. This study was aimed to evaluate the histological
features of gastric mucosa, including H. pylori infection in patients with endoscopically found superfcial gastritis,
erosive gastritis and gastric ulcer.
Method: Subjects with abdominal complaints who underwent consecutive upper gastrointestinal endoscopy
were prospectively selected at Tugurejo Hospital between November 2004 and December 2010. Eligible subjects
were those with endoscopic diagnosis of superfcial gastritis, erosive gastritis or gastric ulcer. The biopsy
specimens were taken from the corpus, angulus and antrum of all the patients. Giemsa and hematoxylin-eosin
staining were used for the histological diagnosis H. pylori and gastric mucosa infammation.
Results: The overall prevalence of H. pylori infection in superficial gastritis, erosive gastritis
and gastric ulcer were 24.3%. There was significant difference between H. pylori infection rate in
antrum of patients with superficial gastritis 19.4%, erosive gastritis 26.3%, and gastric ulcer 34.7%.
The positivity rate of glandular atrophy and intestinal metaplasia of superfcial gastritis with H. pylori-positivity
was 12.5%, 14.0%; erosive gastritis 26.3%, 16.6%; and of gastric ulcer 38.9%, 29.3%; respectively. However,
there was no signifcant difference.
Conclusion: Patients with gastric ulcer have H. pylori infection, atrophic gastritis and metaplasia intestinal
more than superfcial gastritis and erosive gastritis. Progression of the gastric ulcer to atrophic gastritis and
intestinal metaplasia is related to H. pylori infection.
Keywords: Helicobacter pylori infection, superfcial gastritis, erosion and ulcer
ABSTRAK
Latar belakang: Infeksi Helicobacter pylori (H. pylori) dapat menyebabkan terjadinya peradangan pada
mukosa lambung. Hal tersebut dapat merusak epitel lambung dan menjadi risiko terkena kanker lambung. Seiring
dengan berjalannya waktu, atropi kelenjar lambung dan metaplasia intestinal dapat berkembang menjadi kanker
lambung. Penelitian ini bertujuan untuk mengevaluasi histologi dari mukosa lambung meliputi infeksi H. pylori
pada pasien dengan temuan endoskopi sebagai penyebab gastritis ringan, gastritis erosif dan ulkus lambung.
Metode: Pengumpulan data dilakukan secara prospektif dengan rancangan penelitian potong lintang. Subjek
penelitian adalah semua pasien yang menjalani prosedur esofagogastroduodenoskopi secara konsekutif di Rumah
Sakit Tugurejo Semarang pada November 2004-Desember 2010 dengan keluhan pada saluran cerna bagian
atas dan ditemukan sebagai gastritis ringan, gastritis erosif atau ulkus lambung. Pengambilan biopsi dilakukan
pada korpus, angulus dan antrum. Pewarnaan Giemsa dan Hematoxyllin Eosin dilakukan untuk mendiagnosis
infeksi H. pylori dan infamasi pada mukosa lambung.
Volume 13, Number 2, August 2012 75
Helicobacter pylori Infection in Superficial Gastritis, Erosive Gastritis and Gastric Ulcer
Hasil: Secara keseluruhan diketahui prevalensi infeksi H. pylori sejumlah 24,3%. Terdapat perbedaan
bermakna secara statistik untuk infeksi H. pylori di antrum pada gastritis superfsial 19,4%, gastritis erosif
26,3%, dan ulkus lambung 34,7%. Infeksi H. pylori pada atropi kelenjar dan metaplasia intestinal masing-
masing ditemukan pada gastritis superfsial sebesar 12,5% dan 14,0%, pada gastritis erosif 26,3% dan 16,6%;
dan ulkus lambung sebesar 38,9% dan 29,3%, namun secara statistik tidak terdapat perbedaan bermakna.
Simpulan: Pasien dengan ulkus lambung mempunyai infeksi H. pylori, atropi dan metaplasia yang lebih
banyak dibandingkan dengan gastritis superfsial dan gastritis erosif. Infeksi H. pylori dapat mempercepat
perkembangan ulkus menjadi atropi dan metaplasia intestinal.
Kata kunci: infeksi Helicobacter pylori, gastritis superfsial, erosi dan ulkus
INTRODUCTION
In the early 20
th
century, the pathogenesis of acid-
peptic disease was believed to be related to stress and
dietary factors. Later on, other factors such as gastric
secretions, age, sex, smoking and alcohol consumption
were held responsible as the cause.
1
Warren and
Marshall in 1982 discovered a spiral, flagellated
gram-negative organism known as Helicobacter pylori
(H. pylori) which has been implicated in the etiology
of these diseases.
2
While the prevalence of H. pylori
is decreasing in the Western world, it still constitutes
a signifcant medical burden in less industrialized
countries, with constant higher infection rates and a
more widespread distribution.
3
The challenge now is
to fll in the remaining gaps in our knowledge such as
transmission routes as well as genetic preconditions,
as antibiotic resistance increases, develop preventative
strategies including improved hygiene conditions and
vaccination.
4-7
Infection with H. pylori is a co-factor in the
development of duodenal or gastric ulcers (reported to
develop in 1 to 10% of infected patients), gastric cancer
(0.1 to 3%) and gastric mucosa associated lymphoid
tissue (MALT) lymphoma (< 0.01%).
8,9
Infection
with H. pylori may lead to infammation of the gastric
mucosa with subsequent ulceration.
9
Infection is
a major cause of chronic gastritis, a condition that
initiates the pathogenic sequence of events leading
to atrophic gastritis, intestinal metaplasia, dysplasia
and subsequently cancer.
8,10-14
While the bacterium is
not a direct cause of cancer, its presence and resultant
reduction in acid production are necessary factors
in causation.
8,15
The risk of these disease outcomes
in infected patients varies widely among different
populations and the great majority of patients with
H. pylori will not have any clinically significant
complications.
16-18
Diagnosis of H. pylori infection is done either by
rapid urease test in biopsy specimen or microscopic
examination and culture of the specimen or by
other non-endoscopic methods like urea breath test,
H. pylori stool antigen assay or anti-H. pylori
antibodies in the serum.
8,19
H. pylori eradication has
been recommended by various consensus conferences
and its eradication has led to marked reduction in
peptic ulcer disease and need for further therapy.
19,20-22
H. pylori infection has worldwide distribution and
is found to be prevalent and strongly associated
with peptic ulcer disease and gastritis in Pakistani
population.
23
Data of H. pylori infection in superfcial
gastritis and ulcer disease in Indonesia was limited. This
study was aimed to evaluate the histological features
of gastric mucosa, including H. pylori infection, in
patients with endoscopically found superfcial gastritis,
erosive gastritis and gastric ulcer.
METHOD
A cross-sectional study was conducted. All patients
were prospectively selected from subjects with
abdominal complaints who underwent consecutive
upper gastrointestinal endoscopy at Tugurejo Hospital
Semarang between November 2004 and December
2010. The inclusion criteria were subjects with
endoscopic diagnosis of superfcial gastritis, erosive
gastritis and gastric ulcer. Subjects were excluded
from the study if they had history of receiving anti-
ulcer agents or antibiotics during two weeks before
endoscopy or had previous history of duodenal
ulcers, or gastric surgery. All patients have given their
informed consent prior to endoscopy.
Biopsy specimens for histological diagnosis were
obtained endoscopically from the greater curvature of
the lower, the upper corpus and the lesser curvature of
the lower corpus of the stomach, according to the triple-site
gastric biopsy method. The specimens were fxed overnight
in buffered formalin, embedded in paraffn, cut into three
m thickness, and stained with hematoxylin-eosin
The Indonesian Journal of Gastroenterology, Hepatology and Digestive Endoscopy 76
Jacobus Albertus, Abdul Aziz Rani, Marcellus Simadibrata, Murdani Abdullah, Ari Fahrial Syam
The grades of mononuclear cell and polymorpho-
nuclear cell infltration, mucosal glandular atrophy and
intestinal metaplasia in patients are shown in Table 3
and 4. The grades of mononuclear cell infltration and
polymorphonuclear cell infltration in gastric ulcer
were higher than that in superfcial gastritis patients
and erosive gastritis, but it was not significantly
different.
The positivity rate of mucosa glandular atrophy and
intestinal metaplasia of superfcial gastritis, erosive
gastritis, and gastric ulcer patients with H. pylori
positivity was signifcantly higher in gastric ulcer than
superfcial gastritis (Table 5).
staining. In accordance with the Updated Sydney
System, the degree of gastric mucosal infammation
(mononuclear and poly-morphonuclear cell infltration),
glandular atrophy, and intestinal metaplasia were
classified into four grades as follows: 0 = none,
1 = mild, 2 = moderate and 3 = severe.
14
Histologically,
H. pylori infection was considered negative if
H. pylori were absent from all biopsy sites stained
with hematoxylin-eosin staining. H. pylori infection
was considered positive if at least one of the histology
tests was positive.
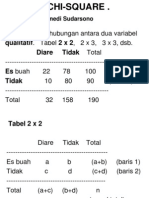
The prevalence of H. pylori infection, rates of
gastric mucosal infammation, polymorphonuclear cell
infltration, glandular atrophy and intestinal metaplasia
were compared using the chi-square test for 4-fold
table. The difference in grades of mononuclear cell
infiltration, polymorphonuclear cell infiltration,
glandular atrophy and intestinal metaplasia between
diseases was compared by Mann-Whitney test.
If p < 0.05 was considered statistically signifcant.
RESULTS
Two hundred and sixteen patients were enrolled
in this study consisted of 72 patients with superfcial
gastritis aged from 38 to 68 years (mean age 56.3
9.9); 72 patients with erosive gastritis aged from 38
to 66 years (mean age 65.3 10.4); 72 patients with
gastric ulcer aged from 38 to 70 years (mean age 65.7
10.8).
Predominant sites of lesions based on endoscopical
diagnosis are shown in Table 1. The positivity rates
for H. pylori infection in studied patients are shown in
Table 1. Endoscopical diagnosis and predominant sites of lesion
Endoscopical
diagnosis
Predominant site of location lesion
n (%)
Corpus Antrum
Corpus and
antrum
Superfcial gastritis 3 (4.16) 37 (51.38) 30 (41.67)
Erosive gastritis 19 (26.39) 51 (70.83) 2 (2 .78)
Gastric ulcer 16 (22.22) 47 (65.28) 9 (12.5)
Table 2. Helicobacter pylori infection identifed in antrum and
associated diseases
Endoscopical diagnosis H. pylori infective rate (%) p*
Superfcial gastritis 19.4
0.042 Erosive gastritis 26.3
Gastric ulcer 34.7
*Chi-square test
Table 3. The grade of gastric mucosal infammation in patients
Diagnosis
Mononuclear (%) Polymorphonuclear (%)
p*
0 1 2 3 0 1 2 3
Superfcial gastritis 44.3 30.9 10.1 14.7 72.7 3.5 4.5 19.2
0.091 Erosive gastritis 3.8 27.0 23.0 43.4 36.7 3.8 10.1 52.1
Gastric ulcer 4.2 11.3 17.0 67.5 17.8 3.1 17.5 61.5
0: none; 1: mild; 2: moderate; 3: severe; *Mann-Whitney test
Table 4. The grade of glandular atrophy and intestinal metaplasia in patients
Diagnosis
Atrophy Intestinal metaplasia
p*
0 1 2 3 0 1 2 3
Superfcial gastritis 77.6 18.7 2.2 1.5 85.3 4.2 4.9 5.6
0.087 Erosive gastritis 62.3 13.1 10.5 14.1 81.7 8.5 3.4 6.4
Gastric ulcer 56.2 10.7 11.8 21.3 71.7 6.7 8.1 13.5
0: none; 1: mild; 2: moderate; 3: severe; *Mann-Whitney test
Table 2. There was no data of H. pylori at angulus sites
since the pathologist had not evaluated H. pylori from
the antrum and angulus. The prevalence of H. pylori
infection in gastric ulcer was signifcantly higher than
that of superfcial gastritis and erosive gastritis.
Table 5. Glandular atrophy and intestinal metaplasia in patients with Helicobacter pylori
infection and associated disease
Diagnosis
Glandular atrophy Intestinal metaplasia
p*
H. pylori + (%) H. pylori + (%)
Superfcial gastritis 12.5 14.0
0.038 Erosive gastritis 23.6 16.6
Gastric ulcer 38.9 29.3
*Chi-square
Volume 13, Number 2, August 2012 77
Helicobacter pylori Infection in Superficial Gastritis, Erosive Gastritis and Gastric Ulcer
DISCUSSION
H. pylori infections tend to be initiated at the antrum
and extend proximally into the corpus along the lesser
curvature. This study showed antrum-predominant
gastritis. Such result is similar to the results of studies
in Asian countries, including China, Vietnam, Thailand
and Myanmar.
24
In Japanese patients, H. pylori infection
and chronic active gastritis progress to the corpus
with advancing age, resulting in corpus-predominant
gastritis. In constant, antrum gastritis will not develop
into corpus gastritis in the Nepalese like other Asian
populations.
24
The difference of mucosal changes
induced by H. pylori infection between the Japanese
and other Asian populations may be correlated with the
different incidences of gastric cancer in the Japanese
and other Asian populations.
24
Uemura et al, reported
that among H. pylori infected Japanese patients,
those with severe atrophy accompanying intestinal
metaplasia, corpus-predominant gastritis or both, are
particularly high risk.
25
Epidemiological evidence indicates that H. pylori
infections are much more prevalent in developing
countries than in developed nations such as the United
States. It has been estimated that 3040% of the
United States population is infected with H. pylori.
9,26
H. pylori remains one of the most common worldwide
human infections and is associated with a number
of important upper gastrointestinal (GI) conditions
including chronic gastritis, peptic ulcer disease, and
gastric malignancy.
26
The prevalence of H. pylori in this study is 24.3%,
which is lower than study reports by Elseweidy et al,
in Egypt (84%), Hashemi et al, in Iran (67.4%), and
Khan et al, in Pakistan (85%).
23,27,28
In India, H. pylori
is positive in 38 (56.7%) asymptomatic individuals
and in 49 (61.3%) symptomatic individuals.
29
In Jordan, H. pylori is frequent in 82% of 197 study
subjects.
30
Prevalence of H. pylori in Indonesia
reported by Albertus et al, using polymerase chain
reaction (PCR) to detect H. pylori is 46.7%,
31
Syam
AF et al, using rapid urea test (Pronto Dry) found
10.2% of prevalence.
32
Previous studies have shown
that the prevalence of H. pylori infections is affected
by several factors, including living conditions, income,
ethnicity, socio-economic status, especially infection
in childhood, availability of public water supplies and
sewers, the number of family support organizations,
and the number of rooms in the home.
1-3
The reasons
for erratic rates of H. pylori infection may be reported
from the country.
In comparison between H. pylori- positive and
H. pylori-negative patients, mononuclear cell
infiltration was more severe in H. pylori-positive
patients with superfcial gastritis, erosive gastritis
and gastric ulcer than H. pylori-negative patients.
We assume that it was related with the grade of
mononuclear cell infiltration, polymorphonuclear
cell infltration and the grade of H. pylori infection.
More intense bacterial infection and more severe
polymorphonuclear cell infltration may contribute
more to DNA damage and promote carcinogenesis
in patients with gastric cancer. Furthermore, chronic
H. pylori infection is also associated with increased
gastric cell turnover, probably of importance in
malignant transformation.
33-37
Glandular atrophy and intestinal metaplasia were
found in more than half of H. pylori negative patients
but were remarkably low in the H. pylori-positive
patients. However, there was no signifcant difference
between H. pylori-positive and negative patients.
Glandular atrophy scores and intestinal metaplasia
scores of all sites in H. pylori-infected Japanese
patients was signifcantly higher compared to this
study.
24,38
Zhang and Yamada reported that there was a tight
link between atrophic gastritis and intestinal metaplasia
in stomachs of Japanese patients with early gastric
cancer.
39
Occasionally, glandular atrophy and intestinal
metaplasia tissues were found in H. pylori-negative
patients; while in the tissues without glandular atrophy
or intestinal metaplasia, we may found H. pylori
positive. These fndings suggest that most patients
with intestinal metaplasia and glandular atrophy have
been infected with H. pylori at some stage. H. pylori
infection may provide the proper environment for
atrophic gastritis and intestinal metaplasia to occur.
At the fnal stage of the disease, gastric atrophy with
intestinal metaplasia is not a hospitable environment
for H. pylori. It may also associated with a dramatic
reduction or even disappearance of the organism.
40-43
This study did not explore H. pylori strains and
(interleukin) IL-1 polymorphisms because there is
no facility for culture. Several H. pylori virulence
and associated genes have been found in Western
populations to be correlated to an increased risk of
gastric cancer and pre-cancerous lesions.
34
Moreover,
it has been confirmed that IL-1 polymorphisms
contributes to the gastric acid secretory response,
facilitating H. pylori infection and subsequently
developing clinical sequelae.
43
The Indonesian Journal of Gastroenterology, Hepatology and Digestive Endoscopy 78
Jacobus Albertus, Abdul Aziz Rani, Marcellus Simadibrata, Murdani Abdullah, Ari Fahrial Syam
CONCLUSION
Patients presenting with gastric ulcer have H. pylori
infection, atrophic gastritis and metaplasia intestinal
more than superfcial gastritis and erosive gastritis.
Progression of the gastric ulcer to atrophic gastritis and
intestinal metaplasia is related to H. pylori infection.
REFERENCES
1. Tan V, Wong B. Helicobacter pylori and gastritis: untangling
a complex relationship 27 years on. J Gastroenterol Hepatol
2011;26:42-5.
2. Suerbaum S, Michetti P. Helicobacter pylori infections.
N Engl J Med 2002;347:1175-86.
3. Bauer B, Meyer TF. The human gastric pathogen Helicobacter
pylori and its association with gastric cancer and ulcer disease.
Ulcer 2011;2011:3-26.
4. Talley NJ. Gastric cancer consensus conference recommends
Helicobacter pylori screening and treatment in asymptomatic
persons from high-risk populations to prevent gastric cancer.
Am J Gastroenterol 2008;103:51021.
5. Rozen P. Cancer of the gastrointestinal tract: early detection
or early prevention? Eur J Cancer Prev 2004;13:71-5.
6. OKeefe J, Moran AP. Conventional, regulatory and
unconventional T cells in the immunologic respon to
Helicobacter pylori. Helicobacter 2008;13:1-19.
7. EL-Zimaity HM, Recent advances in the histopathology of
gastritis. Curr Diagn Pathol 2007;13:340-8.
8. Lopes J. Helicobacter pylori infection: update on diagnosis and
management. J Am Acad Physic Assistants 2010;23:2037.
9. McColl KE. Helicobacter pylori infection. N Eng J Med
2010;362:1597-604.
10. Amiri M, Janssen F, Kunst A. The decline in stomach cancer
mortality: exploration of future trends in seven European
countries. Eur J Epidemiol 2011;26:23-8.
11. Capelle L, de Vries A, Looman C. Gastric MALT lymphoma:
epidemiology and high adenocarcinoma risk in a nation-wide
study. Europ J Cancer 2008;44:2470-6.
12. Take S, Mizuno M, Ishiki K, Yoshida T, Ohara N, Yokota
K, et al. The long-term risk of gastric cancer after the
successful eradication of Helicobacter pylori. J Gastroenterol
2011;46:318-24.
13. Caruso ML, Fucci L. Histological identification of
Helicobacter pylori in early and advanced gastric cancer.
J Clin Gastroenterol 1990;12:601-2.
14. Dixon MF, Genta RM, Yardley JH, Correa P. Classifcation and
grading of gastritis. The updated Sydney system. International
workshop on the histopathology of gastritis, Houston 1994.
Am J Surg Pathol 1996;20:1161-81.
15. Luminari S, Cesaretti M, Marcheselli L. Decreasing incidence
of gastric MALT lymphomas in the era of anti-Helicobacter
pylori interventions: results from a population based study
on extranodal marginal zone lymphomas. Annals Oncol
2009;21:8559.
16. Cheung TK, Wong CY. Treatment of Helicobacter pylori and
prevention of gastric cancer. J Dig Dis 2008;9:8-13.
17. Alsolaiman MM, Bakis G, Nazeer T, MacDermott RP, Balint
JA. Five years of complete remission of gastric diffuse large
B cell lymphoma after eradication of Helicobacter pylori
infection. Gut 2003;52:507-9.
18. Bornschein J, Rokkas T, Selgrad M, Malfertheiner P.
Helicobacter pylori and clinical aspects of gastric cancer.
Helicobacter 2009;14:41-5.
19. Yeomans N. The ulcer sleuths: the search for the cause of
peptic ulcers. J Gastroenterol Hepatol 2011;26:35-41.
20. OConnor A, Gisbert J, McNamara D, OMorain C. Treatment
of Helicobacter pylori infection 2010. Helicobacter
2010;15:46-52.
21. Welin M, Holmgren NM, Nilsson P, Enroth H. Statistical
model of the interactions between Helicobacter pylori
infection and gastric cancer development. Helicobacter
2003;8:728.
22. Kabir S. Effect of Helicobacter pylori eradication on
incidence of gastric cancer in human and animal models:
underlying biochemical and molecular events. Helicobacter
2009;14:159-71.
23. Khan SS, Zulfqar A, Danish KF. Prevalence of H. pylori
infection in patients with gastroduodenal disease in Pakistan.
Rawal Med J 2008;33:8890.
24. Matsuhisa T, Miki M, Yamada N, Sharma SK, Shrestha BM.
Helicobacter pylori infection, glandular atrophy, intestinal
metaplasia and topography of chronic active gastritis in
the Nepalese and Japanese population: the age, gender and
endoscopic diagnosis matched study. Kathmandu Univ Med
J 2007;5:295-301.
25. Uemura N, Okamoto S, Yamamoto S, Matsumura N,
Yamaguchi S, Yamakido M, et al. Helicobacter pylori
infection and the development of gastric cancer. N Engl J
Med 345;2001:784-9.
26. Chey WD, Wong BC, and the Practice Parameters Committee
of the American College of Gastroenterology. Guideline
on the management of Helicobacter pylori infection. Am J
Gastroenterol 2007;102:180825.
27. Elseweidy M, Taha MM, Younis NN, Khadiga S, Hamouda
HA, Eldosouky MA, et al. Pattern of gastritis as manipulated
by current state of Helicobacter pylori infection. Intern J
Biol Biomed Enginer 2010;4:12-21.
28. Hashemi MR, Rahnavardi M, Bikdeli B, Zahedani MD.
H. pylori infection among 1,000 Southern Iranian dyspeptic
patients. World J Gastroenterol 2006;12:5479-82.
29. Singh V, Trikha B, Nain CK, Singh K, Vaiphei K. Epidemiology
of Helicobacter pylori and peptic ulcer in India. J Gastroenterol
Hepatol 2002;17:659-665.
30. Abu-Ahmad NM, Odeh JA and Sallal AKJ. Prevalence of
Helicobacter pylori gastritis at the North of Jordan. Jordan J
Biol Sci 2011;4:71-6.
31. Albertus J, Rani AA, Simadibrata M, Abdullah M, Syam AF,
Gani RA. Mucus thickness of the gastric mucosa and H. pylori
infection in dyspeptic patient with or without diabetic symptom.
Indones J Gastroenterol Hepatol Digest Endosc 2010;11:112-20.
32. Syam AF, Murdani A, Rani A, Nurdjanah H, Adi P, Jumhana
A, et al. Evaluation of the use of rapid urea test: pronto dry to
detect H. pylori in patient with dyspepsia in several cities in
Indonesia. World J Gastroenterol 2006;2:6316-8.
33. Testoni PA, Bonassi U, Bagnolo F, Colombo E, Scelsi R.
In diffuse atrophic gastritis, routine histology underestimates
Helicobacter pylori infection. J Clin Gastroenterol
2002;35:234-9.
34. Welin M, Holmgren NM, Nilsson P, Enroth H. Statistical
model of the interactions between Helicobacter pylori
infection and gastric cancer development. Helicobacter
2003;8:72-8.
Volume 13, Number 2, August 2012 79
Helicobacter pylori Infection in Superficial Gastritis, Erosive Gastritis and Gastric Ulcer
35. Kim JJ, Tao H, Carloni E, Leung WK, Graham DY, Sepulveda
AR. Helicobacter pylori impairs DNA mismatch repair in
gastric epithelial cells. Gastroenterology 2002;123:542-53.
36. Tahara T, Shibata T, Nakamura M, Yoshioka D, Okubo M,
Arisawa T, et al. Gastric mucosal pattern by using magnifying
narrow-band imaging endoscopy clearly distinguishes
histological and serological severity of chronic gastritis.
Gastrointest Endosc 2009;70:246-53.
37. Peek RM, Crabtree JE. Helicobacter infection and gastric
neoplasia. J Pathol 2006;208:23348.
38. Rugge M, Correa P, Dixon MF, Fiocca R, Hattori T, Lechago
J, et al. Gastric mucosal atrophy: interobserver consistency
using new criteria for classifcation and grading. Aliment
Pharmacol Ther 2002;16:1249-59.
39. Zhang C, Yamada N. Helicobacter pylori infection, glandular
atrophy and intestinal metaplasia in superfcial gastritis, gastric
erosion, erosive gastritis, gastric ulcer and early gastric cancer.
World J Gastroenterol 2005;11:791-6.
40. Kapadia CR. Gastric atrophy, metaplasia, and dysplasia:
a clinical perspective. J Clin Gastroenterol 2003;36:S29-36.
41. Kabir S. Effect of Helicobacter pylori eradication on
incidence of gastric cancer in human and animal models:
underlying biochemical and molecular events. Helicobacter
2009;14:159-171.
42. Lauwers GY, Srivastava A. Gastric preneoplastic lesions
and epithelial dysplasia. Gastroenterol Clin North Am
2007;36:813-29.
43. Figueiredo C, Machado JC, Pharoah P, Seruca R, Sousa
S, Carvalho R, et al. Helicobacter pylori and interleukin 1
genotyping: an opportunity to identify high risk individuals
for gastric carcinoma. J Natl Cancer Inst 2002;94:1680-7.
Correspondence:
Jacobus Albertus
Department of Internal Medicine
Tugurejo District General Hospital
Jl. Raya Tugurejo Semarang 50185 Indonesia
Phone/facsimile: +62-24-7605578
E-mail: bert_smg@yahoo.co.id
You might also like
- Helicobacter Pylori Infection in Gastritis and UlcersDocument25 pagesHelicobacter Pylori Infection in Gastritis and UlcersAri AldopiNo ratings yet
- The Association Between Metaplasia and Gastric Malignancy With Helicobater Pylori InfectionDocument4 pagesThe Association Between Metaplasia and Gastric Malignancy With Helicobater Pylori InfectionEnvhy AmaliaNo ratings yet
- Helicobacter Pylori InfectionDocument8 pagesHelicobacter Pylori InfectionNovitaNo ratings yet
- H. Pylori Gastritis Diagnosis and TreatmentDocument27 pagesH. Pylori Gastritis Diagnosis and TreatmentHeersh Raof100% (1)
- Helicobacter Pylori Infection and Peptic Ulcer Disease: in Patients With Liver CirrhosisDocument12 pagesHelicobacter Pylori Infection and Peptic Ulcer Disease: in Patients With Liver CirrhosisHalik Alif HayaNo ratings yet
- En V27n4a02Document6 pagesEn V27n4a02Humberto Liu BejaranoNo ratings yet
- Helicobacter PyloriDocument3 pagesHelicobacter Pyloriursula_ursulaNo ratings yet
- Duodenal Ulcer - StatPearls - NCBI BookshelfDocument6 pagesDuodenal Ulcer - StatPearls - NCBI Bookshelfimehap033No ratings yet
- 37poflee EtalDocument3 pages37poflee EtaleditorijmrhsNo ratings yet
- Corpus GastritisDocument5 pagesCorpus Gastritisameer143No ratings yet
- Kavitt Robert T Diagnosis and Treatment of Peptic 2019Document10 pagesKavitt Robert T Diagnosis and Treatment of Peptic 2019Nix Santos100% (1)
- With Chronic Tonsillitis and Laryngopharyngeal RefluxDocument6 pagesWith Chronic Tonsillitis and Laryngopharyngeal RefluxRamaSumualNo ratings yet
- Gastritis and Gastropathy Perspectives From The EndoscopistDocument4 pagesGastritis and Gastropathy Perspectives From The Endoscopisthenrique.uouNo ratings yet
- IntroductionDocument2 pagesIntroductionapi-3718174No ratings yet
- Practical Approach To Diagnosis of GastritisDocument9 pagesPractical Approach To Diagnosis of GastritisYao RaNo ratings yet
- KJG074 01 04 PDFDocument13 pagesKJG074 01 04 PDFNovita AfsariNo ratings yet
- Helicobacter Pylori and Gastric MalignancyDocument6 pagesHelicobacter Pylori and Gastric Malignancyabangku4164No ratings yet
- Dr. Dhinesh Babu.K, Prof Dr. M .BhaskarDocument6 pagesDr. Dhinesh Babu.K, Prof Dr. M .BhaskarIOSRjournalNo ratings yet
- Pediatric Helicobacter Pylori Infection MedscapeDocument6 pagesPediatric Helicobacter Pylori Infection MedscapeRismawati AcenkNo ratings yet
- Update Sydney SystemDocument16 pagesUpdate Sydney SystemMohammad IrfanNo ratings yet
- Abdominal TuberculosisDocument9 pagesAbdominal TuberculosisImmanuelNo ratings yet
- Chronic Gastritis in Dermatitis Herpetiformis: A Controlled StudyDocument11 pagesChronic Gastritis in Dermatitis Herpetiformis: A Controlled StudyArdikaNo ratings yet
- Research Journal of Pharmaceutical, Biological and Chemical SciencesDocument6 pagesResearch Journal of Pharmaceutical, Biological and Chemical SciencesSurajit SahaNo ratings yet
- Article 929452-PrintDocument18 pagesArticle 929452-PrintLupu DianaNo ratings yet
- Gastritis - Facts and Doubts: Original PaperDocument10 pagesGastritis - Facts and Doubts: Original Paperindah setiyaniNo ratings yet
- Helicobacter Pylori Infection: Old and NewDocument6 pagesHelicobacter Pylori Infection: Old and NewLika GinantiNo ratings yet
- Akiko S. - Patgen and Therapy of Gastric and Duodenal Ulcer DiseaseDocument20 pagesAkiko S. - Patgen and Therapy of Gastric and Duodenal Ulcer DiseaseRevalitha PutriNo ratings yet
- Morbid AnatomyDocument46 pagesMorbid AnatomyStephanie AndersonNo ratings yet
- Peptic Ulcer Disease: Kalyanakrishnan Ramakrishnan, MD, Frcse, and Robert C. Salinas, MDDocument8 pagesPeptic Ulcer Disease: Kalyanakrishnan Ramakrishnan, MD, Frcse, and Robert C. Salinas, MDMonika WerdiningsihNo ratings yet
- Outcomes of H. pylori Patients After Sleeve GastrectomyDocument4 pagesOutcomes of H. pylori Patients After Sleeve GastrectomyAndrei SarmientoNo ratings yet
- Jurnal TB AbdomenDocument4 pagesJurnal TB AbdomenbelaNo ratings yet
- GastritisDocument13 pagesGastritisDewi RosalindaNo ratings yet
- Hematemesis Melena Due To Helicobacter Pylori Infection in Duodenal Ulcer: A Case Report and Literature ReviewDocument6 pagesHematemesis Melena Due To Helicobacter Pylori Infection in Duodenal Ulcer: A Case Report and Literature ReviewWahyu Agung PribadiNo ratings yet
- Acute and Chronic Gastritis Due To Helicobacter PyloriDocument8 pagesAcute and Chronic Gastritis Due To Helicobacter PyloriCarla HolandNo ratings yet
- Helicobacter and Stomach CancerDocument7 pagesHelicobacter and Stomach CancerRolando AgustianNo ratings yet
- Egypt J Med Microbiol 2009 18 4 165 178Document14 pagesEgypt J Med Microbiol 2009 18 4 165 178Cristina RaduleaNo ratings yet
- Studiu 3 Partea SpecialaDocument5 pagesStudiu 3 Partea SpecialaMara HincuNo ratings yet
- Gastritis - Etiology and Diagnosis - UpToDateDocument8 pagesGastritis - Etiology and Diagnosis - UpToDateMatheus AzevedoNo ratings yet
- Helicobacter Pylori: Infection and Gastric CancerDocument8 pagesHelicobacter Pylori: Infection and Gastric CancerKhánh NguyễnNo ratings yet
- Clinical Biochemistry of The Gastrointestinal TractDocument4 pagesClinical Biochemistry of The Gastrointestinal TractReuben JosephNo ratings yet
- American College of Gastroenterology Guideline On The Management of Helicobacter Pylori InfectionDocument18 pagesAmerican College of Gastroenterology Guideline On The Management of Helicobacter Pylori InfectionShinichi Ferry RoferdiNo ratings yet
- An Alternate Natural Remedy For Symptomatic Relief of Helicobacter Pylori Dyspepsia 2327 5146 1000200Document5 pagesAn Alternate Natural Remedy For Symptomatic Relief of Helicobacter Pylori Dyspepsia 2327 5146 1000200gomitadelimonNo ratings yet
- Abdominal Tuberculosis Research ReviewDocument12 pagesAbdominal Tuberculosis Research ReviewrikarikaNo ratings yet
- H. pylori gastritis and ulcer diseaseDocument6 pagesH. pylori gastritis and ulcer diseasetambamanuellaNo ratings yet
- Jurnal Ayank IKMDocument6 pagesJurnal Ayank IKMpouralNo ratings yet
- Gastritis - Etiology and Diagnosis - UpToDateDocument10 pagesGastritis - Etiology and Diagnosis - UpToDateLizbeth Navarrete SierraNo ratings yet
- Gastritis - Etiology and Diagnosis - UpToDateDocument10 pagesGastritis - Etiology and Diagnosis - UpToDateLizbeth Navarrete SierraNo ratings yet
- Peptic Ulcer Disease - EMEDICINE.2020Document47 pagesPeptic Ulcer Disease - EMEDICINE.2020qayyum consultantfpsc100% (1)
- Helicobacterpylori Manuscript 2020 PDFDocument20 pagesHelicobacterpylori Manuscript 2020 PDFMiryam ParandukNo ratings yet
- Jurnal DigestifDocument19 pagesJurnal DigestifDianaarlyNo ratings yet
- Renu PandeyDocument6 pagesRenu PandeyRenu PandeyNo ratings yet
- Helicobacter Pylori Infection - Recent Developments in DiagnosisDocument16 pagesHelicobacter Pylori Infection - Recent Developments in DiagnosisRima Carolina Bahsas ZakyNo ratings yet
- Pylori 7Document12 pagesPylori 7fprasasyaaNo ratings yet
- Helicobacter Pylori ProtocolsDocument270 pagesHelicobacter Pylori Protocolsenglish-exactlyNo ratings yet
- Colitis: A Practical Approach to Colon and Ileum Biopsy InterpretationFrom EverandColitis: A Practical Approach to Colon and Ileum Biopsy InterpretationAnne Jouret-MourinNo ratings yet
- Diseases 09 00066 v2Document19 pagesDiseases 09 00066 v2BBD BBDNo ratings yet
- CarcinogénesisDocument14 pagesCarcinogénesisLuis Adolfo BermudezNo ratings yet
- The Fear of Gastric Cancer in Patients With Dyspepsia: Challenge in Specialist Care GastroenterologyDocument8 pagesThe Fear of Gastric Cancer in Patients With Dyspepsia: Challenge in Specialist Care GastroenterologyAhana MukherjeeNo ratings yet
- Atlas of Inflammatory Bowel DiseasesFrom EverandAtlas of Inflammatory Bowel DiseasesWon Ho KimNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- JOURNAL Breast CancerDocument10 pagesJOURNAL Breast CancerAndy SelvianNo ratings yet
- BAB 12345 BenerDocument2 pagesBAB 12345 BenerAndy SelvianNo ratings yet
- EBM Diagnosis JurnalDocument7 pagesEBM Diagnosis JurnalAndy SelvianNo ratings yet
- EBM Diagnosis JurnalDocument7 pagesEBM Diagnosis JurnalAndy SelvianNo ratings yet
- Lecnote Block Neoplasia 2011Document28 pagesLecnote Block Neoplasia 2011Andy SelvianNo ratings yet
- Tumor SinusDocument37 pagesTumor SinusAndy SelvianNo ratings yet
- Benign TumorsDocument19 pagesBenign TumorsAndy SelvianNo ratings yet
- Blok NEOPL S Haematobium11Document15 pagesBlok NEOPL S Haematobium11Andy SelvianNo ratings yet
- Oncogene and Tumor Suppressor Gene Lecture NotesDocument43 pagesOncogene and Tumor Suppressor Gene Lecture NotesAndy SelvianNo ratings yet
- (C) Chi-Square 2 X 2Document10 pages(C) Chi-Square 2 X 2Andy SelvianNo ratings yet
- Biosynthesis of HemoglobinDocument41 pagesBiosynthesis of HemoglobinPeri HidayatNo ratings yet
- Plasma and It's ProteinsDocument48 pagesPlasma and It's ProteinsAndy SelvianNo ratings yet
- Endocrine System: Harliansyah, PH.D Dept Biochemistry, FK-UYDocument21 pagesEndocrine System: Harliansyah, PH.D Dept Biochemistry, FK-UYAndy SelvianNo ratings yet
- Struma: Diffusa NodusaDocument10 pagesStruma: Diffusa NodusaAndy SelvianNo ratings yet
- ACID-BASE BALANCEDocument78 pagesACID-BASE BALANCEAndy SelvianNo ratings yet
- Kuliah Asam Basa-InedDocument35 pagesKuliah Asam Basa-InedAndy SelvianNo ratings yet
- Indian Standard: Pla Ing and Design of Drainage IN Irrigation Projects - GuidelinesDocument7 pagesIndian Standard: Pla Ing and Design of Drainage IN Irrigation Projects - GuidelinesGolak PattanaikNo ratings yet
- Dell Compellent Sc4020 Deploy GuideDocument184 pagesDell Compellent Sc4020 Deploy Guidetar_py100% (1)
- USDA Guide To CanningDocument7 pagesUSDA Guide To CanningWindage and Elevation0% (1)
- Civil Service Exam Clerical Operations QuestionsDocument5 pagesCivil Service Exam Clerical Operations QuestionsJeniGatelaGatillo100% (3)
- Production of Sodium Chlorite PDFDocument13 pagesProduction of Sodium Chlorite PDFangelofgloryNo ratings yet
- ISO 13485-2016 - DR - Pack - Control of Non Conforming ProductsDocument4 pagesISO 13485-2016 - DR - Pack - Control of Non Conforming ProductskmasanNo ratings yet
- Methods to estimate stakeholder views of sustainabilityDocument7 pagesMethods to estimate stakeholder views of sustainabilityAlireza FatemiNo ratings yet
- Peran Dan Tugas Receptionist Pada Pt. Serim Indonesia: Disadur Oleh: Dra. Nani Nuraini Sarah MsiDocument19 pagesPeran Dan Tugas Receptionist Pada Pt. Serim Indonesia: Disadur Oleh: Dra. Nani Nuraini Sarah MsiCynthia HtbNo ratings yet
- 2021 Impact of Change Forecast Highlights: COVID-19 Recovery and Impact On Future UtilizationDocument17 pages2021 Impact of Change Forecast Highlights: COVID-19 Recovery and Impact On Future UtilizationwahidNo ratings yet
- October 2009 Centeral Aucland, Royal Forest and Bird Protecton Society NewsletterDocument8 pagesOctober 2009 Centeral Aucland, Royal Forest and Bird Protecton Society NewsletterRoyal Forest and Bird Protecton SocietyNo ratings yet
- Chapter 4 DeterminantsDocument3 pagesChapter 4 Determinantssraj68No ratings yet
- Mounting InstructionDocument1 pageMounting InstructionAkshay GargNo ratings yet
- Job Order Costing: Patrick Louie E. Reyes, CTT, Micb, Rca, CpaDocument45 pagesJob Order Costing: Patrick Louie E. Reyes, CTT, Micb, Rca, CpaClaudette Clemente100% (1)
- Chromate Free CoatingsDocument16 pagesChromate Free CoatingsbaanaadiNo ratings yet
- Desana Texts and ContextsDocument601 pagesDesana Texts and ContextsdavidizanagiNo ratings yet
- A Reconfigurable Wing For Biomimetic AircraftDocument12 pagesA Reconfigurable Wing For Biomimetic AircraftMoses DevaprasannaNo ratings yet
- Consumers ' Usage and Adoption of E-Pharmacy in India: Mallika SrivastavaDocument16 pagesConsumers ' Usage and Adoption of E-Pharmacy in India: Mallika SrivastavaSundaravel ElangovanNo ratings yet
- MQC Lab Manual 2021-2022-AutonomyDocument39 pagesMQC Lab Manual 2021-2022-AutonomyAniket YadavNo ratings yet
- Kathy Davis - Dancing Tango - Passionate Encounters in A Globalizing World-New York University Press (2015)Document236 pagesKathy Davis - Dancing Tango - Passionate Encounters in A Globalizing World-New York University Press (2015)Csongor KicsiNo ratings yet
- 2020 Global Finance Business Management Analyst Program - IIMDocument4 pages2020 Global Finance Business Management Analyst Program - IIMrishabhaaaNo ratings yet
- Advantages of Using Mobile ApplicationsDocument30 pagesAdvantages of Using Mobile ApplicationsGian Carlo LajarcaNo ratings yet
- Prac Res Q2 Module 1Document14 pagesPrac Res Q2 Module 1oea aoueoNo ratings yet
- Efaverenz p1Document4 pagesEfaverenz p1Pragat KumarNo ratings yet
- Essential Rendering BookDocument314 pagesEssential Rendering BookHelton OliveiraNo ratings yet
- Journals OREF Vs ORIF D3rd RadiusDocument9 pagesJournals OREF Vs ORIF D3rd RadiusironNo ratings yet
- Uniform-Section Disk Spring AnalysisDocument10 pagesUniform-Section Disk Spring Analysischristos032No ratings yet
- Case Study IndieDocument6 pagesCase Study IndieDaniel YohannesNo ratings yet
- Kaydon Dry Gas SealDocument12 pagesKaydon Dry Gas Sealxsi666No ratings yet
- Factors of Active Citizenship EducationDocument2 pagesFactors of Active Citizenship EducationmauïNo ratings yet
- SOP-for RecallDocument3 pagesSOP-for RecallNilove PervezNo ratings yet