Professional Documents
Culture Documents
Articulo Ingles Osteomielitis
Uploaded by
caballonskiOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Articulo Ingles Osteomielitis
Uploaded by
caballonskiCopyright:
Available Formats
Commentary & Perspective
Evidence-Based Medicine and Surgical Decision-Making: MRSA and MSSA Osteomyelitis in Children
Commentary on an article by Kevin L. Ju, MD, et al.: Differentiating Between Methicillin-Resistant and Methicillin-Sensitive Staphylococcus
aureus Osteomyelitis in Children. An Evidence-Based Clinical Prediction Algorithm
David J. Zaleske, MD
Louis Pasteur observed that chance favors only the mind that is prepared. Acup-half-lled corollary is that we all have opportunities
for preparation or improvement, continuously. By successive iterations of retrospective analysis and prospective testing, we, as
physicians and surgeons, can identify best practices for helping patients. To add direction and scientic rigor to this process, the
level of evidence for assertions that are added to the literature is also categorized. We now have the ability to search the literature
rapidly and extensively via the Internet, adding appropriate screens or qualiers to avoid data overload. With use of electronic
health records, we can readily track the adoption of an algorithm (a pathway or guideline) and assess whether it is achieving its
desired effect. Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making
decisions about the care of individual patients.
1
In their article, Differentiating Between Methicillin-Resistant and Methicillin-Sensitive Staphylococcus aureus Osteomy-
elitis in Children, Drs. Ju, Zurakowski, and Kocher have given us the evidence-based process by which they have arrived at a
clinical prediction rule for this common entity in pediatric orthopedics. They have done the heavy lifting for us. In their
retrospective review of 129 children with Staphylococcus aureus osteomyelitis, they found that if the patient had a temperature of
>38C, a hematocrit of <34%, a white blood-cell count of >12,000/mL, and a C-reactive protein level of >13 mg/L, there was a
92% chance that the osteomyelitis was caused by methicillin-resistant Staphylococcus aureus (MRSA). On the basis of such data,
they advanced a treatment protocol for the administration of an antibiotic while culture and sensitivity data were pendingi.e.,
either an antibiotic to which both MRSA and methicillin-sensitive Staphylococcus aureus (MSSA) would be sensitive (vanco-
mycin) or an antibiotic to which only MSSAwould be sensitive. The customary recommendation that cultures be obtained prior
to the administration of any antibiotic remains. Is the result by Ju et al. signicantstatistically and also clinically? The results in
their series were statistically signicant, according to their very methodical analysis. The clinical signicance of their results is
subject to several caveats that the authors themselves note in the Discussion. First, the number of MRSA cases was relatively small
(eleven of the 129 cases of osteomyelitis). Second, the study was not designed to establish whether all of the MRSA was of a single
genotype, so the organisms could have changed during the study period. The ability of Staphylococcus aureus to adapt to its host makes
it a formidable and protean pathogen
2
. Another issue not specically discussed by the authors is that their study was not, in the strictest
sense, designed for surgical decision-making. Decisions regarding surgical drainage may be best directed by imaging, at the present
time by magnetic resonance imaging. The decision regarding antibiotics may be best made in close communication with an Infectious
Disease Service. The predictors identied in this retrospective study will need to be tested prospectively. Even with these cautionary
notes, however, the authors have described a process that can be discussed and tested scientically, as this same group has already done
with septic arthritis.
Nevertheless, the possibility that the entire cup of evidence-based medicine is half-empty should at least be considered. A
recent New England Journal of Medicine (April 14, 2011, Vol. 364, No. 15) included two articles regarding protocols to diminish the
transmission of hospital-based MRSA. The conclusions of the articles were opposite
3,4
. In a commentary on those articles, what
would seem to be the appropriate perspective was added: It will be necessary to change the culture of clinical care.
5
Our general
surgical colleagues are embracing these cultural changes with encouraging results. By changing behaviors as directed by new data,
they have improved operative morbidity for high-risk surgery
6
. Therefore, the cup of evidence-based medicine is at least half-lled
for surgery and surgical decision-making.
Drs. Ju, Zurakowski, and Kocher are to be congratulated for embracing this conscientious approach to decision-making in
orthopaedics. It is a journey, not a destination. Patients and surgeons should all benet from high-quality evidence that we
accumulate, improve on, and apply along the way.
e109(1)
COPYRIGHT 2011 BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED
J Bone Joint Surg Am. 2011;93:e109(1-2) d http://dx.doi.org/10.2106/JBJS.K.00785
Downloaded From: http://jbjs.org/ on 11/04/2013
David J. Zaleske, MD*
Orthopedic Service, Gillette Childrens
Specialty Healthcare and Childrens Hospitals
and Clinics of Minnesota, Minneapolis, Minnesota
*The author received no payments or services, either directly or indirectly (i.e., via his institution), from a third party in support of any aspect of this work. Neither
the author nor his institution has had any nancial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that
could be perceived to inuence or have the potential to inuence what is written in this work. Also, the author has not had any other relationships, or engaged in any
other activities, that could be perceived to inuence or have the potential to inuence what is written in this work. The complete Disclosures of Potential Conicts of
Interest submitted by authors are always provided with the online version of the article.
References
1. Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isnt. BMJ. 1996;312:71-2.
2. Lowy FD. How Staphylococcus aureus adapts to its host. N Engl J Med. 2011;364:1987-90.
3. Huskins WC, Huckabee CM, OGrady NP, Murray P, Kopetskie H, Zimmer L, Walker ME, Sinkowitz-Cochran RL, Jernigan JA, Samore M, Wallace D, Goldmann DA; STAR*ICU
Trial Investigators. Intervention to reduce transmission of resistant bacteria in intensive care. N Engl J Med. 2011;364:1407-18.
4. Jain R, Kralovic SM, Evans ME, Ambrose M, Simbartl LA, Obrosky DS, Render ML, Freyberg RW, Jernigan JA, Muder RR, Miller LJ, Roselle GA. Veterans Affairs initiative to
prevent methicillin-resistant Staphylococcus aureus infections. N Engl J Med. 2011;364:1419-30.
5. Platt R. Time for a culture change? New Engl J Med. 2011;364:1464-5.
6. Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:2128-37.
e109(2)
THE J OURNAL OF BONE & J OI NT SURGERY
d
J BJ S . ORG
VOLUME 93-A
d
NUMBER 18
d
SEPTEMBER 21, 2011
COMMENTARY & PERSPECTI VE
Downloaded From: http://jbjs.org/ on 11/04/2013
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- TA in PsychotherapyDocument37 pagesTA in PsychotherapyJesús RiveraNo ratings yet
- Language Dysfunction - Continnum - 2015Document19 pagesLanguage Dysfunction - Continnum - 2015Carolina Posada OrtizNo ratings yet
- 6-Cross Training As A Motivational and ProblemDocument3 pages6-Cross Training As A Motivational and Problemakositabon100% (1)
- Cot 2021 Cleaning and SanitizingDocument3 pagesCot 2021 Cleaning and SanitizingChema Paciones100% (2)
- World War Two Unit PlanDocument22 pagesWorld War Two Unit Planapi-280689729100% (1)
- Epidemiology Kept Simple An Introduction To Traditional and Modern Epidemiology 3rd Edition Chapter 1 Epidemiology Past and PresentDocument35 pagesEpidemiology Kept Simple An Introduction To Traditional and Modern Epidemiology 3rd Edition Chapter 1 Epidemiology Past and PresentDeni HerdianaNo ratings yet
- 102322641, Amanda Wetherall, EDU10024Document7 pages102322641, Amanda Wetherall, EDU10024Amanda100% (1)
- A Natural Approach To Second Language Acquisition PDFDocument14 pagesA Natural Approach To Second Language Acquisition PDFchaitali choudhuryNo ratings yet
- Wim Coca L1Document8 pagesWim Coca L1Abdul Shahfi DahalanNo ratings yet
- Field Quality Services Engineer in Houston TX Resume Nanut Panpreuk GreenDocument1 pageField Quality Services Engineer in Houston TX Resume Nanut Panpreuk GreenNanutPanpreukGreenNo ratings yet
- Risk and Protective Factors in Schizophrenia: Heinz Hafner (Editor)Document322 pagesRisk and Protective Factors in Schizophrenia: Heinz Hafner (Editor)Eva CastanheiraNo ratings yet
- Your Best Chance For: International OffersDocument9 pagesYour Best Chance For: International Offersumesh kumarNo ratings yet
- Application Questions To PonderDocument5 pagesApplication Questions To PonderJasmin KumarNo ratings yet
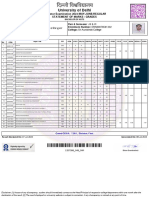
- University of Delhi: Semester Examination 2023-MAY-JUNE:REGULAR Statement of Marks / GradesDocument2 pagesUniversity of Delhi: Semester Examination 2023-MAY-JUNE:REGULAR Statement of Marks / GradesFit CollegeNo ratings yet
- Prasad S Ambalkar ResumeDocument2 pagesPrasad S Ambalkar Resumep1440666No ratings yet
- Business Book Review of Lion TamingDocument8 pagesBusiness Book Review of Lion Tamingjwod_chickNo ratings yet
- Unit 6 Lesson Plan 1 2Document9 pagesUnit 6 Lesson Plan 1 2Thuy Quynh BuiNo ratings yet
- LAB NOTES NW PDFDocument10 pagesLAB NOTES NW PDFAnsha NasarNo ratings yet
- Perdev 2qDocument1 pagePerdev 2qGrace Mary Tedlos BoocNo ratings yet
- STS Report TopicDocument2 pagesSTS Report TopicJunel SildoNo ratings yet
- Fern Smith's Classroom IdeasDocument24 pagesFern Smith's Classroom IdeasSandra Viviana BayonaNo ratings yet
- Exam Steps and Process - Read FirstDocument3 pagesExam Steps and Process - Read FirstDeejaay2010No ratings yet
- 1UR0 4F Que 20201107Document8 pages1UR0 4F Que 20201107Muhammad SaleemNo ratings yet
- YPD Guide Executive Summary PDFDocument2 pagesYPD Guide Executive Summary PDFAlex FarrowNo ratings yet
- JD BD (India) BooksyDocument1 pageJD BD (India) BooksyytrNo ratings yet
- Reading Activity Number 1.Document4 pagesReading Activity Number 1.IVAN ARTURO RODRIGUEZ CASTILLONo ratings yet
- Effective Teaching Methods and Strategies in The EFL Classroom To Facilitate Students' Vocabulary Development 2020Document29 pagesEffective Teaching Methods and Strategies in The EFL Classroom To Facilitate Students' Vocabulary Development 2020Amara PutriNo ratings yet
- SHRM ReviewDocument18 pagesSHRM ReviewjirnalNo ratings yet
- Module: Ergonomics & Facilities Planning in The Hospitality IndustrDocument13 pagesModule: Ergonomics & Facilities Planning in The Hospitality IndustrJUN GERONANo ratings yet
- HOSTEL FEE PAYMENT PROCEDURE FOR SY To FINAL YEARDocument2 pagesHOSTEL FEE PAYMENT PROCEDURE FOR SY To FINAL YEARAbhishek PawarNo ratings yet