Professional Documents
Culture Documents
Endocrinology of Genitourinary System
Uploaded by
GerardLumCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Endocrinology of Genitourinary System
Uploaded by
GerardLumCopyright:
Available Formats
jslum.
com | Medicine
Endocrinology of Genitourinary System
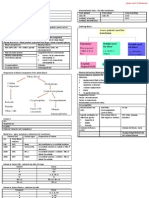
Anatomy Renin
Peptide Hormone
Secreted by Kidney from Granular Cells of Juxtaglomerular Apparatus
Secreted in Response to
↓ Arterial Blood Pressure (↓ in Blood Volume)(Detected by Baroreceptor)
↓ NaCl in Ultra-Filtrate of Nephron
(Flow is Measured by Macula Densa of Juxtaglomerular Apparatus)
Sympathetic Nervous System Activity
(also control BP) (act through β1-Adrenergic Receptors)
Human Renin is Secreted by at least 2 Cellular Pathways
Constitutive Pathway Regulated Pathway
Secretion of Prorenin Secretion of Mature Renin
Processes
↓ BP produce a Baroreceptor Resp onse
(↑ Sympathetic Activity)
↓
Secretes ↑ Renin
↓
Renin → Angiotensinogen → Angiotensin I
↓
(Lungs ) by ACE, Angiotensin I → Angiotensin II
↓
Angiotensin II Produces ↑ Aldosterone
↓
Aldosterone Stimulates Reabsorption of Sodium
(Distal Tubule, Collecting Duct)
↓
Cl- (-ve charge) Follow Na+ (+ve charge) Passively
↓
H2O flows them into Blood (Reabsorption) by Osmosis
Erythropoietin (EPO) (Hematopoietin, Hemopoietin)
Glycoprotein Hormone that Controls Erythropoiesis
Is a Cytokine for Erythrocyte Precursors in Bone Marrow
Produced by Peritubular Capillary Endothelial Cells (in Kidney)
(Peritubular Fibroblasts of Renal Cortex)
Small amounts produced in Liver
Biological Functions
1° - Promoting Red Blood Cell Survival (protecting cells from Apoptosis)
Brain’s Response to Neuronal Injury
Wound Healing Process
Erythropoiesis-Stimulating Agent (ESA)
Exogenous EPO is used as a Performan ce-Enhan cing Drug
Regulation
Feedback Mechanism (measuring Blood Oxygenation)
Hypoxia-Inducible Factors (HIFs) (Transcription Factors for EPO)
Hydroxylated, Proteosomally Digested in Presence of Oxygen
Binds to Erythropoietin Receptor (EpoR) on RBC Surface
Activates JAK2 Cascade
Found in (Activate Intracellular Biological Pathways upon binding with Epo)
• Bone Marrow Cells
• Peripheral, Central Nerve Cells
Cooperates with various Growth Factors
(Involved in Development of Precursor Red Cells)
CFU-E BFU-E
(Colony Forming Unit-Erythroid) (Burst Forming Unit-Erythroid)
Completely dependent on Responsive to Erythropoietin
Erythropoietin
Under Hypoxic Con ditions, Kidney will Produce, Secrete Erythropoietin
(↑ Production of RBC by targeting CFU-E)
Actions
Vasoconstriction-Dependent Hypertension
Stimulate Angiogenesis
Induce Proliferation of Smooth Mus cle Fibers
jslum.com | Medicine
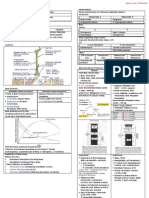
Male
Reproductive System – Gonads, Reproductive Tract, Accessory Sex Glands Reproductive Endocri nology
Reproduction Cells of Leydig in Testis – Secrete Testosterone
Depends on Union of Male, Female Gametes Testosterone is Secreted in Blood, Carried by Plasma Proteins
Female System – Site of Prenatal Development Reaches Target Cells (Numerous Effe cts)
Primary (1°) Reproductive Organs
Male Female Testosterone - 5 Major Effects
Pair of Testis Pair of Ovaries Masculinises Reproductive Tract, External Genitalia (Fetal Testis)
Spermatozoa Ova Growth, Maturation of Reproductive System (onset of Puberty)
Testosterone Estrogen, Progesterone (Essential for Spermatogenesis, Maintain Male Reproductive Tract)
Reproductive Tract + Accessory Organs (found in Either Sex) Development of Sexual Libido
Unique Secondary (2°) Characteristics are found in Each Sex Maintain Sex Drive (in Adult Male)
(Traits include Differences in) Signals Development of Secondary (2°) Sexual Characteristics
Body Configuration Signaling Protein Anabolism
Distribution of Body Hair (Non-Reprodu ctive Functions)
Spermatogenesis
Spermatogonia
Relatively Undifferentiated Primordial Germ Cells
Diploid
In the Outermost Layer in Walls of Seminiferous Tubules
Functional Sperm Cells (near Lumens of Tub ules) (Released)
Proliferate by Mitotic Division (Produce New Primordial Germ Cells)
(Move toward Lumen through Progressive Stages of Spermatogenesis)
Each Sperm-Forming Daughter Cells form 4 Ident ical Primary Spermatocytes
↓
These Dipl oid Cell s Carry out 1s t Me iotic Divi sion
↓
Each Primary Spermatocyte Forms 2 Secondary Spermatocytes
(Haploid, Double-Stranded Chromosome s)
↓
Each Secondary Spermatocytes forms 2 Spermatids
(Haploid, Single-Stranded Chromosome)
Therefore, Each Primary Spermatocyte Forms 4 Spermatids
Spermiogenesis
Packaging (Remodelling) of Spermatids
Differentiation into 4 Parts – Head, Acrosome, Tail, Midpiece
Through Sperm Cell Maturation
Cells are Intimately associated with Sertoli Cells
(cells are in wall of Seminiferous Tubules)
Tight Junctions between Sertoli Cells (form a Blood-Brain Barrier)
Sertoli Cells
Provide Nourishment for Sperm Cells
Carry out Phagocytosis
Secrete a Seminiferous Tubule Fluid into Lumens of Tubules
Site of Action to Control Spermatogenesis (Signalled by Testosterone, FSH)
Hypothalamus-Pituitary-Gonadal Axis (HPG Axis)
Testosterone – Essential for Mitosis, Meiosis of Germ Cells
FSH – Important for Spermatid Remodelling
Estrogen – Male Reproductive Health
Gonadotropin-releasing Hormone Activity ↑ at Puberty
Male Accessory Sex Glands
Seminal Vesicles Prostate Gland Bulbourethral Glands
Fructose for Energy Alkaline Fluid to Mucus Secretion for
Prostaglandin for Neutralize Acidity of Lubrication
Smooth Muscle Female Reproductive
Contraction in Tract Tract
Provide Clotting
Enzymes
Prostaglandins (Locally-Acting Chemical Messengers)(Fatty Acid Derivatives)
• Promote Sperm Transport
• Promote Bronch odilation
• ↑ Renal Blood Flow
• Inhibit HCl from Stomach
• Enhance Cortisol Secretion
jslum.com | Medicine
Female
Reproductive Endocri nology Changes in Uterus
Complex Cycling of Female Sex Hormones Beginning of Menstrual Cycle, there is Sloughing off of Endometrium of Uterus
Ovaries Produce Ova (Due to ↓ Estrogen, Progesterone)
Produce Estrogen, Progesterone Proliferative Phase
Functions of Estrogen In Follicular Phase (↑ Estrogen) cause Thickening in Uterine Lining
Maturation, Maintenance of Female System Uterine Secretory Phase
Establish Female Secondary Sexual Characteristics After Ovulation, Progesterone produce Further Thickening of Uterine Lining
Ova Maturation, Release Suitable for Implantation
Transport of Sperm from Vagina to Site of Fertilization in Oviduct New Ovarian Follicular Phase
Function of Progesterone Degeneration of Corpus Luteum
Prepare a Suitable Environment for Nourishing Developing Embryo, Fetus Menstruation begins
Ovarian Cycle (28 Days) Female Cycle
Cyclical Changes in Cervical Mucous
Fluctuating Estrogen, Progesterone
Puberty changes in Females = Males
GnRH Secretion ↑ (at Onset of Puberty)
GnRH – Stimulate release of Hormones from Anterior Pituitary
Estrogen – Changes in Female Reproductive System, Body Characteristics
Menopause
Mid-Life Hypothalamic Change (cau se Onset of Menopau se)
Characterized by ↑ Irregular Cycles, Dwindling Estrogen Levels
(Has widespread physiological actions)
Hypothalamus-Pituitary-Gonadal Axis (HPG Axis)
Follicular Phase Luteal Phase
1st Half of Cycle Corpus Luteum Left behind in Ovary
Dominated by Maturing Follicles after it loses its sex cell by Ovulation
Granulosa cells of some Primary Corpus Luteum Secretes
Follicles Proliferate • ↑ Progesterone
Oocyte inside each Follicle Enlarges (compared to Follicular Phase)
Theca Cells (in Follicle) • Estrogen
secrete ↑ Estrogen Degenerates after 14 Days of
(Circulate throughout Body) Formation (unless Fertilization,
Rapid Follicular Growth Implantation occur)
↑ FSH signal Ovarian Follicle to If Fertilization, Implantation occur
Secrete ↑ Estrogen Corpus Luteum continue to secrete its
↑ Estrogen Feedback to Inhibit FSH hormones
LH rises (Peaks in Mid-Cycle) (Corpus Luteum of Pregnancy)
Triggers Ovulation Progesterone output Inhibits release
(Estrogen Output ↓) of FSH, LH
(Mature Follicle → Corpus Luteum) With ↓ LH, Corpus Luteum
Degenerates
Ovulation
1 Follicle Grows ↑ Rapidly
Matures about 14 Days after onset of Follicular Development
Follicle Ruptures to release Oocyte (from Ovary)
Released Sex Cell Enters Oviduct (may or may not be Fertilized)
jslum.com | Medicine
Hormones Secreted by Placenta Lactation
hCG
Maintain Corpus Luteum of Pregnancy
Estrogen ↑ Estrogen Secretion Progesterone Prolactin
Stimulate Growth of Myometrium (Strengthen it for Parturition) Promotes Extensive Stimulates Mammary Gland
Progesterone Duct Development in Alveolar-Lobular Development
Suppresses Uterine Contractions Breasts Development
Relaxin Lactation
Softens Cervix to prepare it for Cervical Dilation at Parturition Abrupt ↓ in Estrogen, Progesterone
Placental PTHrp Loss of Placenta
↑ Plasma Ca2+ in Maternal Blood Oxytocin Prolactin
Overall, Maternal Body System respond to ↑ Demands of Gestation Induce Milk Ejection Promotes Milk Secretion
Changes Include Breast Feeding (Advantages)
• Uterine Enlargement Infant Mother
• ↑ Amount of Blood Abundance of I mmune Cells Oxytocin
Many Substances Hastens Involution of Uterus
Parturition (Birth) (eg. Lactoferrin)
During Last Trimester, Uterus becomes More Excitable Weaning (Introdu cing Adult Diet, Withdrawal of Mother’s Milk)
Mild Contraction occur Cessation of Production
Cervix begins to Soften (near Parturition)
Fetus Shifts Downwards (Head Contacting Cervix)
Rhythmic contraction (Begin at Onset of Lab or)
(↑ Estrogen)
Oxytocin
Labor Progresses
Powerful Muscle Stimulant
You might also like
- Thyroid PhysiologyDocument2 pagesThyroid PhysiologyGerardLum100% (2)
- Acute Complications of Diabetes MellitusDocument1 pageAcute Complications of Diabetes MellitusGerardLum100% (1)
- Bam Slam Drug CardDocument4 pagesBam Slam Drug CardLeticia GonzalezNo ratings yet
- Lab Values and Vital SignsDocument4 pagesLab Values and Vital SignsWole Olaluwoye100% (1)
- Hematology summary guideDocument91 pagesHematology summary guidePeter Shirima100% (1)
- Fluid and Electrolyte DisturbancesDocument7 pagesFluid and Electrolyte DisturbancesMarie Antionette MondragonNo ratings yet
- Respiratory PathophysDocument1 pageRespiratory PathophysTori IkeharaNo ratings yet
- UrinalysisDocument9 pagesUrinalysisSukma EffendyNo ratings yet
- Mechanism of Drug Action PDFDocument1 pageMechanism of Drug Action PDFraviomjNo ratings yet
- Blood Erythropoiesis: Ibutnadi Iduyan Ilagan Jarin LopezDocument15 pagesBlood Erythropoiesis: Ibutnadi Iduyan Ilagan Jarin LopezCamille Magdirila100% (1)
- Kidney Function TestDocument21 pagesKidney Function TestVinoantonyNo ratings yet
- Hematologic DisordersDocument32 pagesHematologic DisordersQuolette ConstanteNo ratings yet
- Homeostatic Function of Thyroid and Parathyroid Gland & Calcium HomeostasisDocument15 pagesHomeostatic Function of Thyroid and Parathyroid Gland & Calcium HomeostasisGEETA MOHANNo ratings yet
- Intravenous FluidsDocument19 pagesIntravenous Fluidsblack pink in ur area 21100% (1)
- Physio Reviewer Renal To Acid BaseDocument11 pagesPhysio Reviewer Renal To Acid BaseNicole ChanNo ratings yet
- 1538 Exam 4 Cell Reg & GriefDocument35 pages1538 Exam 4 Cell Reg & GriefJade EdanoNo ratings yet
- Drugclasses Pharmacologypart 1 PDFDocument25 pagesDrugclasses Pharmacologypart 1 PDFSutanya100% (2)
- 3-Major Veins of The BodyDocument26 pages3-Major Veins of The BodyTJPlayz100% (1)
- Pneumonia and BronchiolitisDocument48 pagesPneumonia and Bronchiolitisshashank panwarNo ratings yet
- Calcium Homeostasis: Endocrine Regulation of (Ca)Document4 pagesCalcium Homeostasis: Endocrine Regulation of (Ca)PRANAB KUMAR MUKHERJEENo ratings yet
- Renal Physiology IDocument16 pagesRenal Physiology IJubilee Christiene AngNo ratings yet
- Overview of Fluid and Electrolyte MaintenanceDocument54 pagesOverview of Fluid and Electrolyte MaintenanceIan WongNo ratings yet
- Microcytic Hypochromic AnemiasDocument19 pagesMicrocytic Hypochromic Anemiassaket100% (2)
- Diabetes Management ATIDocument15 pagesDiabetes Management ATIJessica ChirinoNo ratings yet
- Cranial NervesDocument2 pagesCranial NervesakexisNo ratings yet
- Understanding Thalassemia: Causes, Symptoms and TreatmentDocument19 pagesUnderstanding Thalassemia: Causes, Symptoms and TreatmentJayricDepalobosNo ratings yet
- Cholinergic Pharmacology - Drug TableDocument2 pagesCholinergic Pharmacology - Drug TableFNo ratings yet
- AnemiaDocument44 pagesAnemiaAbdulsalam DostNo ratings yet
- Examination of UrineDocument18 pagesExamination of UrineDr. Jayesh PatidarNo ratings yet
- AnaemiaDocument73 pagesAnaemiamedicoprakashNo ratings yet
- (CV2) Pharmacology of AnticoagulantsDocument6 pages(CV2) Pharmacology of AnticoagulantsHanifa Shereen B. AliNo ratings yet
- Abg InterpretationDocument1 pageAbg InterpretationPrincess EspadaNo ratings yet
- I.V Fluid: PathologyDocument7 pagesI.V Fluid: PathologyruchikaNo ratings yet
- Pharm Expansion 17 NDFDocument1 pagePharm Expansion 17 NDFNokz M. Raki-inNo ratings yet
- Burn Injury PathophysiologyDocument1 pageBurn Injury PathophysiologyMonique Ann DanoyNo ratings yet
- DRUG SUMMARY TABLE - Anticoagulantes y AntiagregantesDocument3 pagesDRUG SUMMARY TABLE - Anticoagulantes y AntiagregantesManuel BetancurNo ratings yet
- Causes and Management of Syncope in DentistryDocument27 pagesCauses and Management of Syncope in DentistrySelvarathi KandhaswamyNo ratings yet
- Electrolyte Imbalances Causes: Signs & Symptoms:: Physical Exam: Lab FindingsDocument4 pagesElectrolyte Imbalances Causes: Signs & Symptoms:: Physical Exam: Lab Findingsworleyb83No ratings yet
- InhalDocument33 pagesInhallupeNo ratings yet
- Meds For HypertensionDocument3 pagesMeds For HypertensionZonicsNo ratings yet
- Acid Base Balance PowerpointDocument12 pagesAcid Base Balance PowerpointRoshani Patel100% (2)
- Heart Failure: Signs, Causes, TreatmentsDocument1 pageHeart Failure: Signs, Causes, TreatmentsTrisha VergaraNo ratings yet
- Nephrotic Syndrome - Armando HasudunganDocument18 pagesNephrotic Syndrome - Armando HasudunganzahraaNo ratings yet
- Ecg Crit - CareDocument55 pagesEcg Crit - CarekrismatactayNo ratings yet
- Measuring and Understanding Blood PressureDocument44 pagesMeasuring and Understanding Blood PressureFarwaNo ratings yet
- Urinalysis PDFDocument56 pagesUrinalysis PDFTio AjhaNo ratings yet
- FIBRINOLYTICS, ANTIPLATELETS AND ANTIFIBRINOLYTICSDocument46 pagesFIBRINOLYTICS, ANTIPLATELETS AND ANTIFIBRINOLYTICSBidyut BanerjeeNo ratings yet
- GastrointestinalDocument23 pagesGastrointestinalArvee Caezar F. VizcarraNo ratings yet
- Pharm Fall Cardiovascular Pharmacology Study Guide-106Document47 pagesPharm Fall Cardiovascular Pharmacology Study Guide-106sean liyanageNo ratings yet
- The Urinary System: Renal Physiology and Glomerular FiltrationDocument16 pagesThe Urinary System: Renal Physiology and Glomerular FiltrationRaja Amiruddin100% (1)
- Lesch Nyhan SyndromeDocument25 pagesLesch Nyhan SyndromeDNNo ratings yet
- CVS Lect 6 Blood Pressure, PathophysiologyDocument13 pagesCVS Lect 6 Blood Pressure, PathophysiologySherwan R Shal100% (5)
- Physiology of Vomiting: A Guide to the PathophysiologyDocument24 pagesPhysiology of Vomiting: A Guide to the PathophysiologyKingWayne Tagatac BajoNo ratings yet
- Anti Hypertensive Drugs - ACE InhibitorDocument16 pagesAnti Hypertensive Drugs - ACE InhibitorApurba Sarker Apu100% (1)
- HypertensionDocument12 pagesHypertensionDr. PARMINDER NAINNo ratings yet
- Hierarchy of O2 Delivery SystemsDocument1 pageHierarchy of O2 Delivery SystemsRevNo ratings yet
- Colloids and CrystalooidsDocument42 pagesColloids and Crystalooidsلؤي زعيترNo ratings yet
- Pharmacology - Use of Beta-Blockers & Arbs in Cardiovascular Disease Treating HypertensionDocument5 pagesPharmacology - Use of Beta-Blockers & Arbs in Cardiovascular Disease Treating HypertensionDana20SNo ratings yet
- The Urinary System: Kidneys Form Urine and Regulate Blood PressureDocument2 pagesThe Urinary System: Kidneys Form Urine and Regulate Blood PressureVineila meNo ratings yet
- Pathophysiology of Diabetes Mellitus Type 2Document4 pagesPathophysiology of Diabetes Mellitus Type 2jo_annamae4413100% (3)
- Vesico Ureteral RefluxDocument1 pageVesico Ureteral RefluxGerardLumNo ratings yet
- Urinary Tract Infections in ChildrenDocument1 pageUrinary Tract Infections in ChildrenGerardLumNo ratings yet
- Soft Tissue InfectionsDocument3 pagesSoft Tissue InfectionsGerardLum100% (1)
- Renal Function in Disease StateDocument2 pagesRenal Function in Disease Statedamai140390No ratings yet
- ThrombophiliaDocument3 pagesThrombophiliaGerardLum100% (1)
- Prostate GlandsDocument3 pagesProstate GlandsDragan PetrovicNo ratings yet
- ThalassaemiaDocument4 pagesThalassaemiaGerardLum100% (4)
- Urinary Tract InfectionDocument4 pagesUrinary Tract InfectionGerardLum100% (2)
- Soft Tissue TumoursDocument8 pagesSoft Tissue TumoursGerardLum100% (2)
- Sexually Transmitted DiseasesDocument6 pagesSexually Transmitted DiseasesGerardLum100% (3)
- Skeletal Muscle RelaxantsDocument1 pageSkeletal Muscle RelaxantsGerardLum100% (2)
- Principles of Blood TransfusionDocument2 pagesPrinciples of Blood TransfusionGerardLum100% (3)
- Renal Excretion of DrugsDocument3 pagesRenal Excretion of DrugsGerardLum100% (3)
- Pituitary DysfunctionDocument2 pagesPituitary DysfunctionGerardLum0% (1)
- Pituitary Gland PathologyDocument4 pagesPituitary Gland PathologyGerardLumNo ratings yet
- Pathophysiology of Nerve InjuryDocument2 pagesPathophysiology of Nerve InjuryGerardLum100% (1)
- Posterior Pituitary SyndromeDocument1 pagePosterior Pituitary SyndromeGerardLumNo ratings yet
- Pathophysiology of Calcium, Phosphate HomeostasisDocument5 pagesPathophysiology of Calcium, Phosphate HomeostasisGerardLum100% (1)
- Pathology of Thyroid DiseasesDocument5 pagesPathology of Thyroid DiseasesGerardLum100% (2)
- Pathogenesis Chronic Complications DiabetesDocument5 pagesPathogenesis Chronic Complications DiabetesGerardLum100% (1)
- Pathology of TestesDocument4 pagesPathology of TestesGerardLum100% (1)
- Overview of AnaemiaDocument2 pagesOverview of AnaemiaGerardLumNo ratings yet
- Pathology of DiabetesDocument4 pagesPathology of DiabetesGerardLum100% (4)
- Pathogenesis Bleeding DisordersDocument4 pagesPathogenesis Bleeding DisordersGerardLumNo ratings yet
- Nocturnal EnuresisDocument1 pageNocturnal EnuresisGerardLumNo ratings yet
- Pathology GlomerulonephritisDocument4 pagesPathology GlomerulonephritisGerardLum100% (2)
- Paediatrics OrthopaedicsDocument5 pagesPaediatrics OrthopaedicsGerardLumNo ratings yet
- Obstructive UropathyDocument3 pagesObstructive UropathyGerardLum100% (1)
- Nsaids DrugsDocument2 pagesNsaids DrugsIrene Zae MwandotoNo ratings yet
- Self-Learning Home Task (SLHT)Document9 pagesSelf-Learning Home Task (SLHT)GraceEstoleCaloNo ratings yet
- Female Reproductive System Structures and FunctionsDocument9 pagesFemale Reproductive System Structures and FunctionsReign SaplacoNo ratings yet
- Equine Reproductive Physiology, Breeding, and Stud ManagementDocument383 pagesEquine Reproductive Physiology, Breeding, and Stud Managementfrancisco_aguiar_22100% (2)
- Female Reproductive System: Organs and FunctionsDocument57 pagesFemale Reproductive System: Organs and FunctionsShaira UntalanNo ratings yet
- Steroids From Physiology To Clinical MedicineDocument220 pagesSteroids From Physiology To Clinical MedicineRenan FernandesNo ratings yet
- Your Hormone Levels (Estrogen and Progesterone) Usually Change Throughout The Menstrual Cycle and Can Cause Menstrual SymptomsDocument14 pagesYour Hormone Levels (Estrogen and Progesterone) Usually Change Throughout The Menstrual Cycle and Can Cause Menstrual SymptomsBeverly DatuNo ratings yet
- Lesson Plan: Female Hormonal CyclesDocument9 pagesLesson Plan: Female Hormonal CyclesGunaNo ratings yet
- BIO - SPM 2020 Model Answers - Predicted QuestionsDocument33 pagesBIO - SPM 2020 Model Answers - Predicted QuestionskumarantuitionNo ratings yet
- 004 Grade 10 - SCIENCE - 3rd Quarter Updated VersionDocument43 pages004 Grade 10 - SCIENCE - 3rd Quarter Updated VersionVinz Jegan GalitNo ratings yet
- Justisse MethodDocument64 pagesJustisse Methodtiiandi100% (3)
- Ovarian CystDocument26 pagesOvarian CystAlmyr RimandoNo ratings yet
- Maternal Ob NotesDocument103 pagesMaternal Ob NotesBoris OrbetaNo ratings yet
- ANS3319 FemaleReproductiveAnatomySpring2011Document23 pagesANS3319 FemaleReproductiveAnatomySpring2011Andreea CaticiNo ratings yet
- Lupin Project CompatibleDocument97 pagesLupin Project CompatibleNitish SinghNo ratings yet
- Lipids Properties IdentificationDocument13 pagesLipids Properties IdentificationWnwixiejwis Usisjdx8xjwiNo ratings yet
- Human Reproductive System To BirthDocument11 pagesHuman Reproductive System To BirthDEEBANNo ratings yet
- Mandatory Journal Ovacare Rina AgrawalDocument7 pagesMandatory Journal Ovacare Rina AgrawalChristine LilyanaNo ratings yet
- 24 Lecture PPT - Reproductive SystemDocument47 pages24 Lecture PPT - Reproductive Systemjohnjay3110100% (2)
- Fisiologi HaidDocument3 pagesFisiologi HaidAndi Farid ANo ratings yet
- Pastillas Anticonceptivas y No Profesionales de Voz. Análisis Acústicos.Document14 pagesPastillas Anticonceptivas y No Profesionales de Voz. Análisis Acústicos.Estefani Romero ArriagadaNo ratings yet
- The Female Reproductive System Is Designed To Carry Out Several FunctionsDocument2 pagesThe Female Reproductive System Is Designed To Carry Out Several FunctionsArdie MingayNo ratings yet
- All Obgyn Osce (2) Good Book For OsceDocument75 pagesAll Obgyn Osce (2) Good Book For OsceMohamed Hassan91% (47)
- MCHN OutlineDocument15 pagesMCHN OutlineAngel Strauss KmpsnNo ratings yet
- Feedback Mechanisms in the Female Reproductive SystemDocument11 pagesFeedback Mechanisms in the Female Reproductive SystemHazel Kim Balacy100% (1)
- Care of Patient with Ovarian CystDocument39 pagesCare of Patient with Ovarian CystLuayon FrancisNo ratings yet
- Science Module For Grade 10: Guagua National Colleges, Inc. Guagua, PampangaDocument62 pagesScience Module For Grade 10: Guagua National Colleges, Inc. Guagua, PampangaNorman Punla SantosNo ratings yet
- RATHNADocument30 pagesRATHNAhaisuresh100% (1)
- Care of The Mother and The Fetus During The Perinatal PeriodDocument22 pagesCare of The Mother and The Fetus During The Perinatal PeriodRoshin Tejero100% (1)
- Human Embryology StagesDocument9 pagesHuman Embryology StagesAdvin BurkeNo ratings yet
- Vaginal Bleeding During PregnancyDocument67 pagesVaginal Bleeding During PregnancyLunaLureNo ratings yet