Professional Documents
Culture Documents
Palliative Care AAO-HNS Crse
Uploaded by
api-3698533Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Palliative Care AAO-HNS Crse
Uploaded by
api-3698533Copyright:
Available Formats
Palliative Care in
Otolaryngology
Kenneth M. Grundfast, MD, FACS
Wednesday September 3, 2008
Palliative Care in Otolaryngology 1
Questions:
1. What is palliative care?
2. What is palliative care in
otolaryngology?
3. Why should we discuss
palliative care?
Palliative Care in Otolaryngology 2
Palliative
Adjective
Moderating pain or sorrow by making it easier to
bear.
Noun
Remedy that alleviates pain without curing.
Source: WordNet 1.7.1 Copyright © 2001 by
Princeton University. All rights reserved.
Date "palliative" was first used in popular
English literature: sometime before 1657
Palliative Care in Otolaryngology 3
Palliative Care
Relieving symptoms without attempting to
cure the disease; often refers to treatment
of terminal disease
Often linked with hospice care; American
Academy of Hospice and Palliative
Medicine (AAHPM)
Can have an expanded scope – all care
that is not directed toward complete cure
Palliative Care in Otolaryngology 4
Palliative Medicine
• A new ABMS medical specialty
• Many specialists were hospitalists,
oncologists, some intensivists,
pulmonologists, psychiatrists, a pediatric
otolaryngologist
• Hospitals are developing palliative care
teams
• Can request a consult from a palliative
care team
Palliative Care in Otolaryngology 5
When to request a palliative
medicine consult.
Current therapeutic regimen no longer
effective
Cannot control disease
Cannot alleviate symptoms
Patient’s suffering cannot be alleviated
Patient, family, physician having difficulty
coping
Need advice, expertise in dealing with
issues of death and dying
Palliative Care in Otolaryngology 6
Palliative Care for Surgeons
American College of Surgeons has developed principles of palliative
care
Principles Guiding Care at End of Life
Statement of Principles of Palliative Care was endorsed when it
was recognized that palliative care is equally appropriate to
patients earlier in the course of illness, including those receiving
life-prolonging treatments.
American College of Surgeons: Principles Guiding Care at End
of Life. Bulletin of the American College of Surgeons
1998;83:46.
ACS Statement of Principles of Palliative Care. Bulletin of the
American College of Surgeons: 2005;90(8):34-35.
Palliative Care in Otolaryngology 7
ACS Principles of Palliative
Care
Respect the dignity and autonomy of patients, patients'
surrogates, and caregivers.
Honor the right of the competent patient or surrogate to
choose among treatments, including those that may or
may not prolong life.
Communicate effectively and empathically with patients,
their families, and caregivers.
Identify the primary goals of care from the patient's
perspective, and address how the surgeon's care can
achieve the patient's objectives.
Strive to alleviate pain and other burdensome physical
and nonphysical symptoms
Palliative Care in Otolaryngology 8
ACS Principles of Palliative
Care
Recognize, assess, discuss, and offer access to services
for psychological, social, and spiritual issues.
Provide access to therapeutic support, encompassing
the spectrum from life-prolonging treatments through
hospice care, when they can realistically be expected to
improve the quality of life as perceived by the patient.
Recognize the physician's responsibility to discourage
treatments that are unlikely to achieve the patient's
goals, and encourage patients and families to consider
hospice care when the prognosis for survival is likely to
be less than a half-year.
Palliative Care in Otolaryngology 9
ACS Principles of Palliative
Care
Arrange for continuity of care by the
patient's primary and/or specialist
physician, alleviating the sense of
abandonment patients may feel when
"curative" therapies are no longer useful.
Maintain a collegial and supportive attitude
toward others entrusted with care of the
patient.
Palliative Care in Otolaryngology 10
Core Competencies for Surgical
Palliative Care = Patient Care
Possess the capacity to guide the transition from curative and
palliative goals of treatment to palliative goals alone based on patient
information and preferences, scientific and outcomes evidence, and
sound clinical judgment
Perform an assessment and gather essential clinical information
about symptoms, pain, and suffering
Perform palliative procedures competently and with sound judgment
to meet patient goals of care at the end of life
Provide management of pain and other symptoms to alleviate
suffering.
Communicate effectively and compassionately bad news and poor
prognoses
Conduct a patient and family meeting regarding advance directives
and end-of-life decisions
Exercise sound clinical judgment and skill in the withdrawal and
withholding of life support Care in Otolaryngology
Palliative 11
Core Competencies for Surgical
Palliative Care = Medical Knowledge
Acute and chronic pain management
Non-pain symptom management
Ethical and legal basis for advance directives,
informed consent, withdrawal and withholding of
life support, and futility
Grief and bereavement in surgical illness
Quality of life outcomes and prognostication
Role of spirituality at the end of life
Palliative Care in Otolaryngology 12
Core Competencies for Surgical
Palliative Care = Practice Based Learning
Recognize quality of life and quality of death and
dying outcomes as important components of the
morbidity and mortality review process
Understand their measurement and integration
into peer review process and quality
improvement of practice
Be skilled in the use of introspection and self
monitoring for practice improvement
Palliative Care in Otolaryngology 13
Core Competencies for Surgical
Palliative Care = Professionalism
Surgeons must maintain professional
commitment to ethical and empathic care, which
is patient focused, with equal attention to relief of
suffering along with curative therapy.
Respect and compassion for cultural diversity,
gender, and disability is particularly important
around rituals and bereavement at the end of life.
Maintenance of ethical standards in the
withholding and withdrawal of life support is
essential.
Palliative Care in Otolaryngology 14
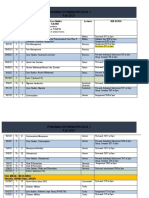
Karnofsky Performance Scale
Palliative Care in Otolaryngology 15
Palliative Performance Scale
% Ambulation Activity and Self-Care Intake Conscious
Evidence of Level
Disease
100 Full Normal Activity Full Normal Full
No Evidence of
Disease
90 Full Normal Activity Full Normal Full
Some Evidence of
Disease
80 Full Normal Activity Full Normal Full
with Effort or
Some Evidence of Reduc
Disease ed
70 Reduced Unable Normal Job Full Normal Full
/ Work or
Some Evidence of Reduc
Disease ed
60 Reduced Unable Hobby / Occasional Normal Full or
House Work Assistance or Confusion
Significant Disease Necessary Reduc
ed
50 Mainly Unable to Do Any Considerable Normal Full or
Sit/Lie Work Assistance or Confusion
ExtensivePalliative
Disease Care in Otolaryngology
Necessary Reduc 16
ed
Palliative Performance Scale
40 Mainly As Above Mainly Norm Full or
in Bed Assistance a Drowsy
or or
Reduc Confusio
30 Totally As Above Total Care Reduc
ed Full
n or
Bed ed Drowsy
Bound or
20 As As Above Total Care Minim Confusio
Full or
Above al n
Drowsy
Sips or
10 As As Above Total Care Mouth Confusio
Drowsy
Above Care n
or
Only Coma
0 Death - - - -
Palliative Care in Otolaryngology 17
Why discuss palliative care in
otolaryngology ?
Palliative Care in Otolaryngology 18
Why discuss palliative care in
otolaryngology ?
Approximately 75% of patients seen in an
otolaryngology practice need no surgery;
usually, 4 office patients seen for every one that
needs a surgical procedure done
Some conditions within the scope of an
otolaryngology practice have no known cure or
usual treatment is a mode of management
known to be only partially effective
Cancer and benign tumors cannot always be
totally excised; surgery can cause dysfunction
Palliative Care in Otolaryngology 19
Why discuss palliative care in
otolaryngology ?
Advancements Advancements
in Otolaryngology in Palliative Care
What we need to
learn and know
Palliative Care in Otolaryngology 20
Palliative Care in
Otolaryngology
Otology-neurotology
Hearing loss, tinnitus
Head and neck oncology
Cancer
Laryngology
Voice, swallowing
Rhinology and allergy
Intractable chronic rhinosinusitis
Palliative Care in Otolaryngology 21
Concepts of cure
Total cure
Eradicate the condition / assure that the condition
does not recur = back to normal
Partial cure
Improve the condition / get better but not back to
normal
Unattainable cure
Medical and/or surgical management will not alter the
course of the condition or disease
Palliative Care in Otolaryngology 22
Patient Expectations
Alleviate symptoms
Preserve function
Preserve life
Cope with the condition
and the situation
Palliative Care in Otolaryngology 23
Surgeon’s Options
Observe, explain, reassure, but
not actively intervene =
observation, watchful waiting
Intervene with medical
management
Intervene with surgical
management
Palliative Care in Otolaryngology 24
What can an otolaryngologist
do for the patient if unable to
cure the condition that the
patient has?
Palliative Care in Otolaryngology 25
57 year old
Vietnamese
man admitted to
Boston Medical
Center
September 8,
2007
Palliative Care in Otolaryngology 26
Past history and exam
PMH: Was seen initially in our clinic in May 2007
with two week history of lower right neck mass
that was non-tender, associated with change in
voice, seven pound weight loss in previous
month
Smoked ½ pack cigarettes per day x 40 years + 2
beers per day
Exam:
Right supraclavicular 4.5x4.5 cm. Level 4 fixed mass
Flexible laryngoscopy – normal cords, cord motion
Palliative Care in Otolaryngology 27
Studies done in 2007
CT thorax: “extensive bulky conglomerate
lymphadenopathy throughout the mediastinum
and right hilum and a parenchymal or
peribronchovascular mass in the medial aspect
of the right upper lobe.”
CT of the neck with contrast: “Right
supraclavicular and anterior mediastinal nodal
conglomerates intimately associated with the
right brachiocephalic and proximal common
carotid arteries.”
Palliative Care in Otolaryngology 28
Studies done in 2007
PET scan: “mutifocal increased FDG-uptake
corresponding to the bulky supraclavicular,
mediastinal and hilar nodes as well as the right
upper lobe mass noted on CT scan. Additional
foci of increased FDG-uptake were present in a
small prevascular node and within the left lung
hilum, possibly indicating contralateral node
spread.”
MRI scan: confirmed the presence of metastatic
disease in the brain.
Palliative Care in Otolaryngology 29
Diagnosis and management
in 2007
Fine Needle Aspiration of the supraclavicular node was
positive for metastatic moderately differentiated
adrenocarcinoma. The cytological changes and
immunohistochemical profile were consistent with a
primary lung tumor.
Patient was diagnosed with stage IV non-small cell lung
cancer involving the neck and brain. He was referred to
Radiation Oncology and Medical Oncology for treatment
and was told to follow up with Otolaryngology if and
when the need arose.
Had XRT and chemotherapy
Palliative Care in Otolaryngology 30
Patient returns in
September 2008
Chief complaint: sore throat, dysphagia, increasing
hoarseness, progressively worsening difficulty breathing
ROS: cough, wheezing
Exam:
Cachectic, multiple enlarged cervical nodes both
sides of the neck; nodular thyroid
NPL: bilateral immobile vocal cords with 2-3 mm
glottic opening
Now biopsies demonstrate that he has metastases to
brain, thyroid, and inguinal lymph nodes
Palliative Care in Otolaryngology 31
Consult Palliative Care Team
Assist delivering bad news
Experience comprehending patient’s cultural
beliefs
Experience with family meeting, interpreting
family dynamics; healthy care proxy
Deciding on limits of care
Proceed to tracheotomy
Supportive care, pain management,
hospice
Palliative Care in Otolaryngology 32
Palliative Care in Otolaryngology
Otolaryngology Clinics of North America
Grundfast Kenneth M, Dunn Geoffrey P
February 2009
Palliative Care in Otolaryngology 33
Tracheotomy near the end of life
Important interface between palliative care
team and otolaryngologists
Decision making far more complex and
difficult than the surgical procedure
Specific indications and risks to be
considered in the patient who is near
death
Palliative Care in Otolaryngology 34
Tracheotomy in Palliative Care
T.Chan + A. Devaiah
Tracheotomy facilitates assisted ventilation in
patients with progressive neuromuscular
disorder such as ALS
Provides comfort and ability to speak when
patient has been intubated for a long time and
likely will need continued assisted ventilation
Helps in management of chronic aspiration,
improves pulmonary toilet
A difficult choice near the end of life
Palliative Care in Otolaryngology 35
Why would the patient who is
near death need to have a
tracheotomy?
Palliative Care in Otolaryngology 36
Why would the patient who is near
death need to have a tracheotomy?
NOT A GOOD IDEA MAYBE A GOOD IDEA
No need to intervene Avoid death from
when interventions are suffocation
being curtailed Avoid larynx
Risks inherent in complications if life is
anesthetizing and prolonged
operating on morbidly ill Provide increased
patient comfort
Taking away a natural Allows patient to speak
way to die with family members and
Potentially limits options loved ones before dying
for further care and Facilitate care and
placement / disposition placement
Palliative Care in Otolaryngology 37
Rehabilitation after Cranial Base
Surgery – S. Jalisi + J. Netterville
Cranial nerve 1: Permanent anosmia, caution not
to use cooking gas at home; noxious gas
detectors at home
Cranial nerve 2: If orbital exenteration, then
prosthesis, depend on vision other eye
Cranial nerve 3: If ptosis, levator muscle
tightening, insert weights in eyelid
Cranial nerve 4: Visual training, eye muscle surg.
Cranial nerve 5: Oral training for mastication,
movement food bolus, swallowing
Cranial nerve 6: Yse refractive prisms
Palliative Care in Otolaryngology 38
Rehabilitation after Cranial Base
Surgery – S. Jalisi + J. Netterville
Cranial nerve 7: hypoglossal to facial
anastamosis; temporalis or masseter muscle
transposition; gracilis free tissue transplant
Cranial nerve 8: BAHA, CROS hearing aid
Cranial nerve 9: assist with swallowing;
pharyngeal flap for V-P incompetence
Cranial nerve 10: Swallowing therapy,
cricopharyngeal myotomy, phonosurgery
Palliative Care in Otolaryngology 39
Rehabilitation after Cranial Base
Surgery – S. Jalisi + J. Netterville
Cranial nerve 11: Physical therapy
Cranial nerve 12: Swallowing therapy
----------------------------------------------------
Patients need to know prior to surgery the
functional impairments that are likely to occur
following surgery
Total excision versus de-bulking of tumors
All surgery today versus some surgery today
and more surgery later
Palliative Care in Otolaryngology 40
When the tumor recurs after surgical
excision: S. Jalisi + A Elackattu
Chemotherapy / radiation therapy
De-bulking for symptom relief
Management of fungating lesion, wound care ---
debridelment, dressings
Microvascular free flap
Mucositis – oral hygiene, oral care products
Xerostomia - Vitamin C, saliva substitutes
Cachexia – nutrition
Hospice care, end of life orders
Palliative Care in Otolaryngology 41
Refractory Chronic Rhinosinusitis
E. Mahoney + R. Metson
Subset of patients with CRS continue to have
troublesome symptoms despite medical and
then surgical management
“Sinusitis spectrum”: local disease and anatomic
factors versus systemic factors; the
“intermediates”
Patients who fail initial medical/surgical therapy
need extensive medical assessment
Palliative Care in Otolaryngology 42
Tips on Management of
Refractory Chronic Rhinosinusitis
Neurology evaluation – rule out migraine, other
disorders
Immuno-modulatory therapy – IVIG infusion
Leukotriene inhibitors
Aspirin de-sensitization
Saline irrigations
Longterm antibiotic therapy
Topically administered antibiotic
Antifungal therapy
Discussions about changing expectations to
treatment
Palliative Care in Otolaryngology 43
Recurrent Respiratory Papillomatosis
K. Johnson + Craig Derkay
By definition, the disorder recurs
Goal is airway and voice preservation
Mainstay is repetitive surgical procedures
Antiviral therapy
Treat extra-esophageal reflux
Immuno-therapy
Birth canal, HPV vaccines
Psychosocial considerations, family dynamics
Palliative Care in Otolaryngology 44
Disorders of Swallowing
S. Langmore, G. Grillone, A. Elackattu, M. Walsh
Surgical options – crico-myotomy,
tracheo-esophageal diversion, laryngeal
suspension, glottic closure
Botox to control sialorrhea
Change texture of feedings
Enteral feeding
Electrical stimulation, neural implant
Palliative Care in Otolaryngology 45
Disorders of Swallowing
S. Langmore, G. Grillone, A. Elackattu, M. Walsh
In consultation with the patient and caregivers,
determine what his/her priorities and wishes are
regarding prolonging life versus maximizing quality of
life. Is a feeding tube a viable option? Is aspiration-
preventing surgery an option? Is preventing aspiration a
high priority?
Refer to a speech pathologist who specializes in
swallowing disorders for behavioral and dietary therapy.
Be sure that the speech pathologist understands the
patient's priorities in terms of quality of life, health, and
preventing aspiration.
Palliative Care in Otolaryngology 46
Disorders of Swallowing
S. Langmore, G. Grillone, A. Elackattu, M. Walsh
Continue to work with a speech pathologist as the
disease/condition worsens as long as the patient is
eating anything orally or has hopes of eating anything
orally. Rehabilitative techniques will evolve toward
compensatory techniques as the patient’s condition
worsens
Feeding tubes and tracheostomy tubes are not always
maximally helpful for intractible dysphagia. They may
help or worsen the swallowing problem and may not
entirely avoid the risk of developing pneumonia. They
should be considered 'last resorts' not the first solutions.
Palliative Care in Otolaryngology 47
Dysphonia and Dysarthria
S. Cohen, A. Elackattu, P. Noordzij,
M. Walsh, S. Langmore
Voice, speech therapy
Alaryngeal speech / TE speech
Phonosurgery
Presbyphonia:
Voice therapy
Bilateral medialization laryngoplasty
Palliative Care in Otolaryngology 48
Tinnitus
A. Shulman + B.Goldstein
“Tinnitology”, a new discipline
Wide range in severity and ability to cope
T T T= tinnitus targeted therapy = combination of
medication + instrumentation such as tinnitus masker
MATP= medical audiologic tinnitus patient protocol;
Feldman masking curves
Transcortical magnetic stimulation
Surgery for otosclerosis
Medication: Klonopin + / - Neurontin
Alternative therapies: Ginko, acupuncture, etc
Palliative Care in Otolaryngology 49
Anosmia
D. Lafreniere + N. Mann
Occurs in the elderly, like presbycusis, can
be associated with Alzheimer’s Disease,
Parkinson’s Disease
No specific treatment; zinc and alpha
lipoic acid have been tried
Need to counsel patient – take steps to
avoid asphyxiation from carbon monoxide
or other noxious gases
Palliative Care in Otolaryngology 50
Chronic Subjective Dizziness (CSD)
M. Ruckenstein + J.P. Staab
1. Persistence > 3 months of symptoms including
one or more of the following:
Chronic lightheadedness
Heavy-headedness
Subjective imbalance frequently not apparent to others
Feeling that “inside of the head” is spinning with
absence of perception of movement in the visual
surround
Feeling that the floor is moving underneath
Feeling of being detached from one’s environment
Palliative Care in Otolaryngology 51
Chronic Subjective Dizziness (CSD)
M. Ruckenstein + J.P. Staab
1. Chronic hypersensitivity to one’s own
motion and/or to movement of objects in
the environment
2. Exacerbation of symptoms in settings
with complex visual fields such as
grocery stores or shopping malls or
when performing precision visual tasks
such as working at a computer
Palliative Care in Otolaryngology 52
CSD Association with other disorders
Anxiety
Migraine
Traumatic brain injury
Treatment of CSD
Psycho-education
Medications: SSRI’s
Behavioral interventions
Palliative Care in Otolaryngology 53
Tips on Management of CSD
Educate to the patient about how malfunction
within the brain can cause symptoms
Address any underlying anxiety disorder with
psychotherapy, medications including
antidepressants and anxietolytics, either alone or
in combination with each other
Teach patient how to access information using
the internet. Vestibular Disorders Association
Let the patient know that you and your team are
and will be easily accessible to provide support
Palliative Care in Otolaryngology 54
Vestibular Rehabilitation
C.D. Hall + L. Clarke Cox
Goal: reduce subjective symptoms, improve gaze and
postural stability particularly during head movements
Mechanisms:
Habituation – long lasting attenuation of a response to
a provocative stimulus
Adaptation – remaining vestibular system adjusts
output according to demands placed on it
Substitution – substitute alternative strategies for
missing vestibular function; visual clues instead of
vestibular input
Palliative Care in Otolaryngology 55
Progressive hearing loss
A. Kozak + K. Grundfast
Progressive hearing loss can be frightening
Some medical treatments but none are reliably
effective; no diagnostic test for AIED, try steroids
= steroid responsiveness methotrexate
BAHA, CROS hearing aid, assisted listening
devices, pocket talker, cochlear implant
Career counseling, family counseling, assisting
with life changes
Preserve hearing in the unaffected ear
Palliative Care in Otolaryngology 56
Managing Intractable Head and Neck Pain
Abdel-Kader MehioM.D., Swapneel K. Shah,M.D.
DERMATOMES
Palliative Care in Otolaryngology 57
Palliative Care in Otolaryngology 58
Palliative Care in Otolaryngology 59
Palliative Care in Otolaryngology 60
Palliative Care in Otolaryngology 61
Tips on Managing Head and Neck Pain
Abdel-Kader Mehio M.D., Swapneel K. Shah,M.D.
Stepwise progression:
Anti-inflammatory meds (steroids) > pulsed
radiofrequency> ablative procedures
“Intravenous rescue” = lidocaine infusion,
magnesium infusion, metoclopramine infusion
Regional blocks
Physical therapy, acupuncture
Refer to Pain Management Team
Palliative Care in Otolaryngology 62
Keep this in mind:
Hippocrates said:
“A physician should aim to cure, heal
as often as possible, but comfort
always”
Palliative Care in Otolaryngology 63
Conclusions
Palliative Medicine is a newly approved
medical specialty
Growing numbers of hospitals are now
developing palliative care teams
Principles of palliative care are applicable
to the practice of otolaryngology
Palliative care is not only for the dying
patient at the end of life
Palliative Care in Otolaryngology 64
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- PP CLUES PDF Latest Pass PDFDocument38 pagesPP CLUES PDF Latest Pass PDFbrightlin misbaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Light Pollution ImpactsDocument7 pagesLight Pollution ImpactsIqra Qazi100% (1)
- Compounded Sterile Products Stability Compendium-AntineoplasticsDocument0 pagesCompounded Sterile Products Stability Compendium-AntineoplasticsRahmalia 'lia Cudby' PrihanantoNo ratings yet
- Odontogenic Tumours - (2) L5Document28 pagesOdontogenic Tumours - (2) L5nooraaaNo ratings yet
- Niosomes PPT ClassDocument34 pagesNiosomes PPT ClassRohan Aggarwal100% (1)
- Lilium Tigrinum: Niki Taylor Lic. ISH IS HomDocument8 pagesLilium Tigrinum: Niki Taylor Lic. ISH IS HomNiki Taylor Lic ISH IS HOM100% (1)
- Chemical Resistance Chart GlovesDocument8 pagesChemical Resistance Chart Glovesjitendertalwar1603No ratings yet
- Makalah Analytical ExpotitionDocument12 pagesMakalah Analytical Expotitionsendal jepit100% (2)
- Breast MCQ Questions on Pathology Findings, Risk Factors and Treatment OptionsDocument55 pagesBreast MCQ Questions on Pathology Findings, Risk Factors and Treatment OptionsAhmad Adel Qaqour94% (16)
- Pancreatic Pseudo Cyst Case - Rachel FlorendoDocument122 pagesPancreatic Pseudo Cyst Case - Rachel FlorendoKM100% (2)
- 2.High-Resolution CT of The Lung EDITIA A-3-A.Document736 pages2.High-Resolution CT of The Lung EDITIA A-3-A.RamonataleNo ratings yet
- 3 Coupled Differential Equations: Mathematical Representation of The Clearance TubeDocument1 page3 Coupled Differential Equations: Mathematical Representation of The Clearance Tubeapi-3698533No ratings yet
- Slide 6Document1 pageSlide 6api-3698533No ratings yet
- Slide 20Document1 pageSlide 20api-3698533No ratings yet
- Slide 18Document1 pageSlide 18api-3698533No ratings yet
- Slide 23Document1 pageSlide 23api-3698533No ratings yet
- Slide 19Document1 pageSlide 19api-3698533No ratings yet
- Slide 21Document1 pageSlide 21api-3698533No ratings yet
- Slide 7Document1 pageSlide 7api-3698533No ratings yet
- Slide 11Document1 pageSlide 11api-3698533No ratings yet
- Slide 17Document1 pageSlide 17api-3698533No ratings yet
- Slide 10Document1 pageSlide 10api-3698533No ratings yet
- Slide 9Document1 pageSlide 9api-3698533No ratings yet
- Slide 24Document1 pageSlide 24api-3698533No ratings yet
- Slide 15Document1 pageSlide 15api-3698533No ratings yet
- Slide 22Document1 pageSlide 22api-3698533No ratings yet
- 3 Coupled Differential Equations: Mathematical Representation of The Clearance TubeDocument1 page3 Coupled Differential Equations: Mathematical Representation of The Clearance Tubeapi-3698533No ratings yet
- Slide 26Document1 pageSlide 26api-3698533No ratings yet
- 07 Annual Report CoverDocument2 pages07 Annual Report Coverapi-3698533No ratings yet
- Annual Report BlurbDocument14 pagesAnnual Report Blurbapi-3698533No ratings yet
- Video Screens ProofDocument14 pagesVideo Screens Proofapi-3698533No ratings yet
- 09 10 08 - Cash Emily 15977 Poster2 RevDocument1 page09 10 08 - Cash Emily 15977 Poster2 Revapi-3698533No ratings yet
- Amaryl M PI - May 2018marylDocument11 pagesAmaryl M PI - May 2018marylvicky upretiNo ratings yet
- Programmed Appropriation and Obligation by Object of ExpenditureDocument7 pagesProgrammed Appropriation and Obligation by Object of ExpenditureKristin Villaseñor-MercadoNo ratings yet
- MCN Lab WRDocument101 pagesMCN Lab WRMaui TabuzoNo ratings yet
- Pharmacological evidence of Hibiscus extractsDocument10 pagesPharmacological evidence of Hibiscus extractsAna TorrealbaNo ratings yet
- Journal of EnterologyDocument139 pagesJournal of EnterologyLenuţa SzakacsNo ratings yet
- Life Expectancy FactorsDocument3 pagesLife Expectancy FactorsRizza GonzagaNo ratings yet
- Selling Sickness: How The World'S Biggest Pharmaceutical Companies Are Turning Us All Into PatientsDocument19 pagesSelling Sickness: How The World'S Biggest Pharmaceutical Companies Are Turning Us All Into PatientsTashi SamdupNo ratings yet
- Buter t1 Case Studies CalendarDocument4 pagesButer t1 Case Studies Calendarapi-602288180No ratings yet
- 14 Meron Mehari Kifle 2016 Knowledge and Practice of Breast Self Examination Among Female College Students in EritreaDocument6 pages14 Meron Mehari Kifle 2016 Knowledge and Practice of Breast Self Examination Among Female College Students in EritreaArick Frendi AndriyanNo ratings yet
- Ovarian CancerDocument3 pagesOvarian CancerKaija PouporeNo ratings yet
- Jurnal Prognosis Radiologi 1Document9 pagesJurnal Prognosis Radiologi 1Henry WijayaNo ratings yet
- Simple GoitreDocument13 pagesSimple GoitreEmad WalyNo ratings yet
- Kerala Uiversity Bhms PapersDocument31 pagesKerala Uiversity Bhms PapersKarthikNo ratings yet
- Pigmented Purpuric Dermatoses: PathophysiologyDocument5 pagesPigmented Purpuric Dermatoses: PathophysiologyrohitNo ratings yet
- Adult T-Cell Leukemia Lymphoma (Atll) A Rare Case Associated With Human T-Cell Virus (Htlv-1)Document19 pagesAdult T-Cell Leukemia Lymphoma (Atll) A Rare Case Associated With Human T-Cell Virus (Htlv-1)Priya ChandakNo ratings yet
- QIMP14 AppendixDocument12 pagesQIMP14 AppendixShahriar MostafaNo ratings yet
- Mbbs Pathology QuestionsDocument11 pagesMbbs Pathology QuestionsAli KhanNo ratings yet
- Kenya Medical Training College - Nyamira End of Year Three Semester One Examination March 2015 KRCHN Class (Pre-Service)Document4 pagesKenya Medical Training College - Nyamira End of Year Three Semester One Examination March 2015 KRCHN Class (Pre-Service)Mursal RashidNo ratings yet
- 5 - RenalDocument5 pages5 - RenalMaLiha SuLtanaNo ratings yet