Professional Documents
Culture Documents
Alan Breier Et Al - Association of Ketamine-Induced Psychosis With Focal Activation of The Prefrontal Cortex in Healthy Volunteers
Uploaded by
Cortate15gOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Alan Breier Et Al - Association of Ketamine-Induced Psychosis With Focal Activation of The Prefrontal Cortex in Healthy Volunteers
Uploaded by
Cortate15gCopyright:
Available Formats
KETAMINE-INDUCED PSYCHOSIS AND BREIER, Psychiatry 154:6, June 1997 AL.
PREFRONTAL CORTEX Am J MALHOTRA, PINALS, ET
Association of Ketamine-Induced Psychosis With Focal Activation of the Prefrontal Cortex in Healthy Volunteers
Alan Breier, M.D., Anil K. Malhotra, M.D., Debra A. Pinals, M.D., Neil I. Weisenfeld, B.S.E., and David Pickar, M.D.
Objective: Agents that antagonize the N-methyl-D-aspartic acid (NMDA) receptor, such as phencyclidine and ketamine, produce an acute psychotic state in normal individuals that resembles some symptoms of schizophrenia. The aim of this study was to determine which brain regions are involved in NMDA receptor-mediated psychosis. Method: Positron emission tomography with [18F]fluorodeoxyglucose was used to determine cerebral metabolic activity in 17 healthy volunteers while an acute psychotic state was induced simultaneously by the administration of subanesthetic doses of ketamine. Results: Ketamine produced focal increases in metabolic activity in the prefrontal cortex and an acute psychotic state. A change in one psychotic symptom, conceptual disorganization, was significantly related to prefrontal activation. Conclusions: These data suggest that the prefrontal cortex may be involved in mediating NMDA receptor-induced psychosis. (Am J Psychiatry 1997; 154:805811)
hencyclidine (PCP) antagonizes the N-methyl-Daspartic acid (NMDA) receptor (1, 2), a major site of excitatory neurotransmission in the brain, and produces a broad range of cognitive and behavioral disturbances that include psychosis (3, 4). As early as the 1950s, it was noted that in healthy volunteers, PCP and its analogues produced an acute psychotic state that resembled some of the symptoms of schizophrenia, particularly thought disorder, delusions, perceptual alterations, and negative symptoms (58). This led to speculation that PCP might be a useful pharmacologic tool for studying pathophysiologic processes of this illness. Subsequently, it was learned that PCP had longlasting behavioral effects in some individuals and that PCP and other potent NMDA antagonists caused neuropathologic damage in the rat brain (9). Ketamine, on the other hand, is a lower-potency NMDA antagonist and a widely used dissociative anesthetic agent (10). It has a short half-life, and in subanesthetic doses it does not appear to have long-term behavioral effects in healthy volunteers (11). Subanesthetic doses of ketamine produce a range of cognitive and behavioral effects similar to those of PCP, including psychotic
Received Aug. 29, 1996; revisions received Dec. 2, 1996, and Jan. 6, 1997; accepted Jan. 15, 1997. From the Experimental Therapeutics Branch, NIMH. Address reprint requests to Dr. Breier, Experimental Therapeutics Branch, NIMH, Bldg. 10, Rm. 4N212, 9000 Rockville Pike, Bethesda, MD 20892. The authors thank James V. Haxby and Jose M. Maisog for help with data processing and analysis, the staffs of the 4-East inpatient unit and Clinical Center PET Department for personnel and technical support, and Marilyn Duncan for editorial assistance.
symptoms (11, 12). Thus, ketamine has been proposed as a pharmacologic probe of NMDA function for clinical studies and provides a means of studying NMDAmediated psychosis in human subjects (11, 12). Brain regions responsible for NMDA-mediated psychosis have not been established. NMDA receptors are located throughout the mammalian brain, with highest densities in the cerebral cortex, limbic system, and striatum (13). Autoradiographic studies of PCP and ketamine administration in rodents demonstrate activation in limbic and some cortical regions (1417). Low doses tend to focally activate the neocortex and limbic structures, while higher doses cause more homogeneous activation throughout these areas. Deactivation in somatosensory and auditory systems has been reported (1417), and in the case of PCP there is some evidence that acute activation predominates, with deactivation occurring 24 hours later (18). In a [15O]H2O positron emission tomography (PET) study of five patients with schizophrenia (19), ketamine caused an increase in blood flow in the anterior cingulate and a decrease in blood flow in the hippocampus and primary visual cortex. The aim of the present study was to identify brain regions involved in NMDA-induced psychosis in healthy human subjects. We examined cerebral metabolic activity in 17 healthy volunteers, using [18F]fluorodeoxyglucose (FDG) and PET, while simultaneously inducing an acute psychotic state with subanesthetic doses of ketamine. Healthy volunteers, as opposed to patients with neuropsychiatric illnesses, were considered desirable for this study because they are free of the
Am J Psychiatry 154:6, June 1997
805
KETAMINE-INDUCED PSYCHOSIS AND PREFRONTAL CORTEX
FIGURE 1. Adjusted Mean Cerebral Metabolic Activity During Ketamine Infusion After Subtraction of Metabolic Data Obtained During Placebo Infusion in 17 Healthy Volunteers in a PET Studya
aThe
data are displayed as statistical maps overlaid on a single subjects magnetic resonance imaging scan, with each individual transverse slice cut parallel to the anterior-posterior commissural plane according to the brain atlas of Talairach and Tournoux (22). Negative and positive slice numbers are millimeters below and above the anterior-posterior commissural plane. polysubstance abuse and alcohol dependence, as determined from a structured diagnostic interview (20). The subjects participated in two FDG PET studies conducted on separate days (mean number of days between studies=7.8, SD=6.5). On one day, ketamine (a 0.12-mg/kg bolus, followed by a 0.65-mg/kg constant infusion for 1 hour) was administered, and on the other day, placebo (saline) was administered for 1 hour. Ketamine and placebo administration was double-blind and in random order.
effects of prior drug treatment and long-standing pathophysiologic processes. The ketamine dose we used is severalfold lower than the anesthetic dose (10) and was determined on the basis of earlier studies of ketamines cognitive effects at subanesthetic doses in healthy subjects (11, 12) and our own dose-finding studies. We chose the lowest dose that consistently produced psychosis, in order to reduce the likelihood of metabolic effects in regions not involved in this phenomenon.
METHOD
Seventeen healthy volunteers (15 male and two female; mean age=30.4 years, SD=6.8) were recruited through the National Institutes of Health normal volunteer program and participated in the study after giving written informed consent to the protocol, which was approved by the institutional review board. Three subjects had completed high school, eight had a partial college education, five were college graduates, and one had completed graduate school. The groups racial/ethnic composition was 14 white, two black, and one Hispanic. The subjects were in good physical health, as determined by physical examination, ECG, and screening blood work, and had no past or current psychiatric illnesses, including
PET Studies
The PET studies were conducted with a Scanditronix (Uppsala, Sweden) PC 1024-7B tomograph. Four blocks of seven axial images were obtained sequentially as interleaved data sets with 3.5-mm spacing between each of the blocks. In-plane resolution was 5.2 mm, and axial resolution was 10 mm. A thermoplastic mask was fitted for each subject and fixed in place to minimize head movement. Eye patches were fixed to the mask, and lights were dimmed throughout the procedure. Following a transmission scan, the ketamine and placebo infusions commenced. Ten minutes after the initiation of infusions, a single injection of 5 mCi of FDG in 9 cc of normal saline was administered. Serial sampling of warmed, arterialized venous blood was conducted throughout the postinjection and scanning periods. Thirty-five minutes after FDG injection, scanning began. Regional cerebral metabolic rates of glucose utilization were determined on the basis of the Sokoloff model (21). In an attempt to standardize mental activity across subjects and conditions, we asked subjects to per-
806
Am J Psychiatry 154:6, June 1997
BREIER, MALHOTRA, PINALS, ET AL.
form a simple auditory continuous performance task during FDG uptake; this involved indicating discrimination of a low-volume tone by pressing a hand-held button. Scans were rescaled and resliced to produce stereotactically normalized images corresponding to those of the atlas of Talairach and Tournoux (22). Individual images were registered according to the method of Woods et al. (23). Images were then smoothed with Gaussian filters of 20 mm, 20 mm, and 12 mm for the x, y, and z axes, respectively. Differences between the ketamine and placebo conditions were evaluated with the use of the statistical parametric mapping developed by Friston et al. (2426). A pixel-based analysis of covariance produced two metabolic maps (placebo infusion and ketamine infusion) for each subject, normalized to mean global metabolic activity; changes in metabolic activity from placebo data were determined by calculating F ratios for planned comparisons and using a pooled estimate of error variance. The F values were converted to z scores. Clusters of contiguous voxels that exceeded a threshold z score of 3.09 were identified and assessed for significance (p<0.05) by means of the particle analysis method of Friston et al. (27). This method determines the probability that an activation or deactivation of a given spatial extent (i.e., cluster) could occur by chance anywhere in the brain volume under investigation. Each significant cluster is listed with its volume (in centimeters cubed) and probability level. The probability level is determined from the following equation: p(n
max
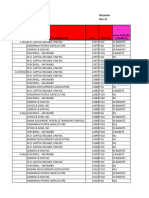
TABLE 1. Local Maxima for Each Area Demonstrating Significantly Increased Metabolic Activity During Ketamine Infusion as Compared to Placebo Infusion in 17 Healthy Volunteers in a PET Study Talairach Coordinate x y z
Area of Significantly Increased Activitya Left inferior, middle, and medial frontal cortex (16.7 cm3, p<0.00001) Inferior (area 45) Middle (area 10) Medial (area 10) Left middle frontal cortex (area 9) (3.0 cm3, p=0.0009) Right middle frontal cortex (area 10) (1.7 cm3, p=0.02)
z Scoreb
42 30 4 42 +26
+28 +50 +54 +8 +52
+4 +12 +20 +44 +4
4.39 4.19 3.73 3.98 4.12
aBrodmanns area for each local maximum is indicated in parentheses. bConversion of F value for planned comparison of effect of ketamine
versus placebo on metabolic activity. cebo) and time as factors was conducted. Drug-by-time interactions are reflected by F and p values. Post hoc Newman-Keuls tests were used to determine significant differences between the drug conditions at the individual time points, and Pearsons correlation coefficients were used to relate the ratings made during drug exposure on the ketamine infusion test day to the regions of interest from the ketamine infusion test day. The data are presented as means and standard deviations, and the comparisons are two-tailed.
k ) = 1 exp ( E m
e k
2D
),
where nmax refers to the maximum number of voxels in any of the clusters found, k is the parameter in the equation, exp and e are the base of the natural logarithm, E is the expected value, m represents the number of clusters, is a parameter that depends on the number of significant clusters and the number of voxels throughout the brain for which the associated z value exceeded the threshold, and D is the dimensionality of the data set (three in this case) (27). Estimated spatial smoothness (full width at half maximum) was 10.99 mm in x, 10.65 mm in y, and 12.74 mm in z (Fristons W=2.72). Local maxima within each cluster were identified as voxels that had a higher z score than any voxel in a 1.81.82-cm space (995 voxels) centered on that voxel. The locations of local maxima are expressed as Talairach and Tournoux coordinates and corresponding Brodmann areas. For correlative analyses with behavioral data, regions of interest were placed on individual unprocessed images before their deformation and registration for pixel-by-pixel analyses. This was done post hoc (i.e., regions of interest were placed on areas corresponding to regions of significant activation that were identified in the pixel-bypixel analyses). The regions of interest were spherical in shape and placed blind to drug administration condition (i.e., ketamine versus placebo), and data were normalized for global activity (region of interest divided by global activity, mg glucose/100 g tissue per minute).
RESULTS
Behavioral Assessments
Behavioral ratings were made from a clinical interview conducted by a research psychiatrist (A.K.M.) blind to ketamine versus placebo administration, using the Brief Psychiatric Rating Scale (BPRS) (28). Ratings were obtained before ketamine and placebo administration (baseline), 10 minutes after commencement of ketamine and placebo administration (during drug exposure), and 30 minutes after the cessation of the infusion (end of the study). Each BPRS item is rated from 1 (not present) to 7 (severe), and scores were based on the content and form of verbal products of the subject. Four symptoms (conceptual disorganization, hallucinatory behavior, unusual thought content, and suspiciousness) were summed as a psychosis cluster, and both the cluster and individual symptoms were examined. The anxiety-depression cluster, composed of three items, was also examined. Although we (11) and others (12) have reported that ketamine induces negative symptoms, these were not included in this study because of the limitations in assessing these symptoms while a subject is actively undergoing a PET scan. The thermoplastic mask and positioning in the scanner prevented adequate visual inspection for appropriately assessing blunted affect and social withdrawal. An analysis of variance with drug condition (ketamine versus pla-
Ketamine produced bilateral increases in metabolic activity in the prefrontal cortex but no significant activation in other areas (figure 1, table 1). Probability levels for each cluster were determined according to the method of Friston et al. (27), as mentioned in the Method section. Two significant clusters of increased activity were found on the left: one large cluster (16.7 cm3) including the inferior, middle, and medial frontal gyrus, and another that was more superiorly located (3.0 cm3) in the middle frontal gyrus (table 1). There was one significant cluster of increased activity on the right (1.7 cm3) in the middle frontal gyrus. There was a very small area of deactivation (1.3 cm3) (p=0.04, N= 17) in the right cerebellum (Brodmanns area 37; Talairach and Tournoux coordinates +14, 61, 16). There were no significant differences in global mean metabolic activity for placebo (11.37 mg glucose/100 g tissue per minute, SD=1.93) and ketamine (11.65 mg glucose/100 g tissue per minute, SD=1.93) (t=0.52, df=16, p=0.61). Similar to our previously reported findings (11), ketamine produced significant increases in psychosis, beginning moments after the bolus injection and persisting throughout the hour-long infusion period (table 2). The individual psychotic symptoms that were significantly affected were conceptual disorganization, unusual thought content, and hallucinatory behavior; suspiciousness was not significantly affected, and there were no significant effects on the anxiety-depression factor (table 2). Regions of interest were placed on the left and right
Am J Psychiatry 154:6, June 1997
807
KETAMINE-INDUCED PSYCHOSIS AND PREFRONTAL CORTEX
TABLE 2. Effects of Ketamine and Placebo on BPRS Scores of 17 Healthy Volunteers in a PET Study Score Baseline Symptoms and Drug Condition Psychosis Placebo Ketamine Conceptual disorganization Placebo Ketamine Unusual thought content Placebo Ketamine Hallucinatory behavior Placebo Ketamine Suspiciousness Placebo Ketamine Anxiety-depression cluster Placebo Ketamine clusterb Mean 4.0 4.2 1.0 1.1 1.0 1.0 1.0 1.0 1.0 1.0 3.2 3.2 SD 0.0 0.5 0.0 0.3 0.0 0.0 0.0 0.0 0.0 0.0 0.4 0.6 During Drug Infusion Mean 4.4 9.2c 1.1 2.7c 1.1 2.7c 1.1 1.5 1.0 1.2 3.2 3.4 SD 1.0 3.2 0.5 1.1 0.5 1.4 0.2 0.9 0.0 0.8 0.4 1.1 Analysisa End of Study Mean 4.0 4.7 1.0 1.2 1.0 1.3 1.0 1.0 1.0 1.0 3.0 3.1 SD 0.0 0.8 26.8 0.0 0.4 16.4 0.0 1.0 3.7 0.0 0.0 1.7 0.0 0.0 0.5 0.0 0.3 0.50 0.20 0.03 F (df=2, 32) 39.3 p <0.0001 <0.0001 <0.0001
aRepeated measures analysis of variance, drug-by-time interaction. bConsists of conceptual disorganization, unusual thought content, hallucinatory behavior, and suspiciousness. cSignificantly different from placebo condition (Newman-Keuls post hoc test, df=32, p<0.001).
middle frontal gyri that appear on three consecutive slices beginning at the anterior-posterior commissural line and extending superiorly approximately 12 mm, which corresponded to bilateral areas of significant activation identified by the statistical parametric mapping. There was a significant relationship between ketamine-induced changes in conceptual disorganization and right and left prefrontal metabolic activity (figure 2). The three other psychotic symptoms, the psychosis cluster, and the anxiety-depression cluster were not related to frontal metabolic activity (range of correlations: r=0.32, p=0.21, to r=0.20, p=0.43; df=16). Age was not significantly related to either left prefrontal metabolic activity (r=0.04, df=16, p=0.90) or right prefrontal metabolic activity (r=0.12, df=16, p=0.60).
DISCUSSION
The results of this study indicate that the prefrontal cortex is focally activated during ketamine-induced psychosis in healthy individuals. Ketamine produced bilateral prefrontal activation, with greater effects on the left side, and an acute psychosis that was characterized by conceptual disorganization, perceptual alterations, and unusual thought content. Conceptual disorganization was found to be specifically correlated with prefrontal metabolic effects, providing support for the hypothesis that the prefrontal cortex may be involved in the mediation of ketamine-induced thought disorder. Although ketamine has effects at other sites, including the receptor, opiate receptor, acetylcholinesterase, and monoamine transporter sites, several lines of evidence indicate that ketamine-induced psy-
chosis is mediated through the PCP site. Ketamines affinity for the PCP site is severalfold greater than for other sites (29, 30), and drug discrimination studies indicate that low doses of NMDA antagonists enhance PCP site selectivity (31). Thus, our low-dose infusion paradigm would favor mediation of effects through the PCP site. Selective agents for , opiate, cholinergic, and monoamine transporters do not block ketamine-induced cognitive effects (32). Moreover, selective agents for these systems produce behavioral states unlike that induced by ketamine, while the ketamine-induced behavioral state is similar to the clinical picture produced by other agents with even higher selectivity for the PCP site than ketamine (such as PCP itself) (58, 11, 12). A striking finding in this study was the focalization of ketamine-related metabolic effects, in that activation was restricted to the prefrontal cortex. Other neocortical and limbic areas are rich in NMDA receptors (13), and studies in rodents have demonstrated ketamine-induced increased glucose utilization in limbic areas (14). The reason for activation of the prefrontal cortex without metabolic effects in other brain regions rich in NMDA receptors may have been the ketamine dose we used; it was sufficient to produce a psychotic state consistently but low enough to minimize activation in brain regions not involved in psychosis. Studies in laboratory animals have demonstrated dose-dependent effects of ketamine and other NMDA antagonists on glucose utilization in the neocortex in which low doses produced a laminar pattern of increased metabolic activity and higher doses produced more homogeneous effects (14, 17, 33). Weissman and colleagues (33) found that low doses of PCP increased glucose utilization in the superficial layers of the frontal cortex, whereas high
808
Am J Psychiatry 154:6, June 1997
BREIER, MALHOTRA, PINALS, ET AL.
FIGURE 2. Relationships Between Ketamine-Induced Effects on Left and Right Prefrontal Metabolism and Ratings of Conceptual Disorganization in 17 Healthy Volunteers in a PET Study
r=0.53, df=16, p=0.03.
r=0.52, df=16, p=0.03.
doses reduced glucose utilization in this region. Studies in rodents have shown that NMDA antagonists produce increased glucose utilization in the limbic cortex, with more marked increases when higher doses were used (14, 17, 33). In addition, the rodent prefrontal cortex is comparatively underdeveloped (34), so there may be poor homology between humans and rats for specific prefrontal cognitive processes. Last, it is also possible that additional regions may have been affected by ketamine but were below the statistical threshold of detection used in this study. In a recently reported study of five neuroleptictreated patients with schizophrenia (19), ketamine caused blood flow increases in the cingulate cortex and decreases in the visual cortex and hippocampus. Several differences between this study and ours make direct comparisons difficult. The differences include subjects (patients versus healthy volunteers), neuroleptic treatment, study group size, ketamine dose and administration (single bolus versus bolus/constant infusion), use of [15O]H2O versus FDG, and study design (preketamine versus postketamine comparisons as opposed to a randomized, placebo-controlled design). Nevertheless, the activation of the anterior cingulate (recently reported) and of the prefrontal cortex (reported here)two regions in close neuroanatomical proximity and functionally interrelated (34)provides support for anterior corticolimbic involvement in ketamine-induced psychosis. We are now examining the effects of ketamine on cerebral metabolic activity in neuroleptic-free and neuroleptic-treated patients with schizophrenia, which will add to the growing body of data relevant to this issue. The prefrontal cortex is of particular interest as a possible site of NMDA-associated psychosis. In addition to having a high density of NMDA receptors (13), it integrates cortical and subcortical information for the exe-
cution of complex cognitive programs (34). Glutamate is a major neurotransmitter in cortical-subcortical and cortical connections (35). Perturbation of normal prefrontal glutamatergic neurotransmission would be expected to disrupt these association functions. In nonhuman primates prefrontal cortical lesions that include association areas cause distractibility, poor concentration, and impaired performance on cognitive tasks that reflect thought integration and processing (36, 37). It is reasonable to hypothesize that disruption in prefrontal association functions could be involved in the pathophysiology of psychosis. In schizophrenic patients, thought disorder has been positively correlated with right frontal blood flow (38), and activation of auditory hallucinations has been associated with increases in left prefrontal blood flow (39)both in regions corresponding to areas activated in this study (i.e., Brodmanns areas 10 and 45, respectively). Several caveats should be considered before interpreting the relevance of these data for the pathophysiology of schizophrenia. First, caution must be used in extrapolating from the effects of an acute pharmacologic challenge to a chronic neuropsychiatric illness. Although the drug administration was double-blind, it was generally apparent when ketamine was given because of its psychotogenic effects. In addition, the behavioral state produced by subanesthetic doses of ketamine bears resemblance to some, but not all, features of schizophrenia (11, 12). Conceptual disorganization, perceptual alterations, and unusual thought content are observed in both conditions, whereas gross temporal and spatial distortions are commonly observed with NMDA antagonists but are relatively rare in schizophrenia. Conceptual disorganization is particularly important, because it is a hallmark psychotic symptom of schizophrenia. Although ketamine-induced conceptual disorganization resembles the thought dis-
Am J Psychiatry 154:6, June 1997
809
KETAMINE-INDUCED PSYCHOSIS AND PREFRONTAL CORTEX
order observed in schizophrenia, the magnitude of ketamines effects is relatively modest, and a single BPRS item does not adequately reflect this complex behavioral state. In several brain imaging studies of subjects with schizophrenia, the prefrontal cortex has not been activated during certain cognitive tasks (4042), a phenomenon called hypofrontality. This literature has been summarized by Andreasen and associates (40). Our data suggest, however, that prefrontal activation may be related to some positive-type symptoms of this illness. Perhaps the acute onset of these symptoms is an energy-demanding state reflected in activation in brain imaging studies, whereas chronic symptoms relate to relative decrements in blood flow and glucose utilization. Support for this hypothesis comes from investigations in schizophrenic patients which have demonstrated that prefrontal activation is associated with the acute onset of specific psychotic symptoms (39, 43) and from studies indicating that chronic symptoms, such as negative symptoms, are related to prefrontal hypofunction (40, 44, 45). In conclusion, our data suggest that subanesthetic doses of ketamine produce focal prefrontal activation and an acute psychotic state in healthy subjects. A component of the psychosis, conceptual disorganization, was related to prefrontal activation. These findings contribute to a growing body of data implicating NMDA/glutamate systems and the prefrontal cortex in the genesis of some forms of psychotic symptoms.
REFERENCES 1. Zukin SR, Zukin RS: Specific [3H]phencyclidine binding in rat central nervous system. Proc Natl Acad Sci USA 1979; 76:5372 5376 2. Vincent JP, Kartalovski B, Geneste P, Kamenka JM, Lazdunski M: Interaction of phencyclidine (angel dust) with a specific receptor in rat brain membranes. Proc Natl Acad Sci USA 1979; 76:46784682 3. Corssen G, Domino EF: Dissociative anesthesia: further pharmacologic studies and first clinical experience with the phencyclidine derivative CI-581. Anesth Analg 1966; 45:2940 4. Meyer JS, Greifenstein F, DeVault M: A new drug causing symptoms of sensory deprivation. J Nerv Ment Dis 1959; 129:5461 5. Bakker CB, Amini FB: Observations on the psychotomimetic effects of Sernyl. Compr Psychiatry 1961; 2:269280 6. Luby ED, Cohen BD, Rosenbaum F, Gottlieb J, Kelley R: Study of a new schizophrenomimetic drug, Sernyl. Arch Neurol Psychiatry 1959; 81:363369 7. Ban TA, Lohrenz JJ, Lehmann HE: Observations on the action of Sernyla new psychotropic drug. Can Psychiatr Assoc J 1961; 6:150156 8. Davis BM, Beech HR: The effect of 1-arylcyclohexylamine (Sernyl) on twelve normal volunteers. J Ment Sci 1960; 106:912 924 9. Olney JW, Labruyere J, Price MT: Pathological changes induced in cerebrocortical neurons by phencyclidine and related drugs. Science 1989; 244:13601362 10. White PF, Way WL, Trevor AJ: Ketamineits pharmacology and therapeutic uses. Anesthesiology 1982; 56:119136 11. Malhotra AK, Pinals DA, Weingartner H, Sirocco K, Missar CD, Pickar D, Breier A: NMDA receptor function and human cognition: the effects of ketamine in healthy volunteers. Neuropsychopharmacology 1996; 14:301307
12. Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD, Heninger GR, Bowers MB Jr, Charney DS: Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans: psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry 1994; 51:199214 13. Monaghan DT, Buller AL: Anatomical, pharmacological, and molecular diversity of native NMDA receptor subtypes, in The NMDA Receptor, 2nd ed. Edited by Collingridge GL, Watkins JC. New York, Oxford University Press, 1995, pp 158176 14. Crosby G, Crane AM, Sokoloff L: Local changes in cerebral glucose utilization during ketamine anesthesia. Anesthesiologist 1982; 56:437443 15. Tamminga CA, Tanimoto K, Kuo S, Chase TN, Contreras PC, Rice KC, Jackson AE, ODonohue TL: PCP-induced alterations in cerebral glucose utilization in rat brain: blockade by metaphit, a PCP-receptor-acylating agent. Synapse 1987; 1:497504 16. Meibach RC, Glick SD, Cox R, Maayani S: Localisation of phencyclidine-induced changes in brain energy metabolism. Nature 1979; 282:625626 17. Hammer RP, Herkenham M: Altered metabolic activity in the cerebral cortex of rats exposed to ketamine. J Comp Neurol 1983; 220:396404 18. Gao XM, Shirakawa O, Du F, Tamminga CA: Delayed regional metabolic actions of phencyclidine. Eur J Pharmacol 1993; 241: 715 19. Lahti AC, Holcomb HH, Medoff DR, Tamminga CA: Ketamine activates psychosis and alters limbic blood flow in schizophrenia. Neuroreport 1995; 6:869872 20. Spitzer RL, Williams JBW, Gibbon M, First MB: Instruction Manual for the Structured Clinical Interview for DSM-III-R (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1989 21. Sokoloff L, Reivich M, Kennedy C: The [14C]deoxyglucose method for the measurement of local cerebral glucose utilization: theory, procedure, and normal values in the conscious and anesthesized albino rat. J Neurochem 1977; 28:897916 22. Talairach J, Tournoux P: Co-Planar Stereotaxic Atlas of the Human Brain. New York, Thieme Medical, 1988 23. Woods RP, Cherry SR, Mazziotta JC: Rapid automated algorithm for aligning and reslicing PET images. J Comput Assist Tomogr 1992; 16:620633 24. Friston KJ, Frith CD, Liddle PF, Lammertsma AA, Dolan RD, Frackowiak RSJ: The relationship between local and global changes in PET scans. J Cereb Blood Flow Metab 1990; 10:458 466 25. Friston KJ, Frith CD, Liddle PF, Frackowiak RSJ: Comparing functional (PET) images: the assessment of significant change. J Cereb Blood Flow Metab 1991; 11:690699 26. Friston KJ, Frith CD, Liddle PF, Frackowiak RSJ: Plastic transformation of PET images. J Comput Assist Tomogr 1991; 15: 634639 27. Friston KJ, Worsley KJ, Frackowiak RSJ, Mazziotta JC, Evans AC: Assessing the significance of focal activations using their spatial extent. Human Brain Mapping 1994; 1:210220 28. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychol Rep 1962; 10:799812 29. Hampton RY, Medzihradsky F, Woods JH, Dahlstrom PJ: Stereospecific binding of 3H phencyclidine in brain membranes. Life Sci 1982; 30:21472154 30. Oye I, Paulsen O, Maruset A: Effects of ketamine on sensory perception: evidence for a role of N-methyl-D-aspartate receptors. J Pharmacol Exp Ther 1992; 260:12091213 31. Javitt DC, Zukin SR: Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry 1991; 148:13011308 32. Byrd LD, Standish LJ, Howell LL: Behavioral effects of phencyclidine and ketamine alone and in combination with other drugs. Eur J Pharmacol 1987; 144:331341 33. Weissman AD, Dam M, London ED: Alterations in local glucose utilization induced by phencyclidine. Brain Res 1987; 435:2940 34. Fuster JM: The Prefrontal Cortex, 2nd ed. New York, Raven Press, 1989 35. Cotman CW, Monaghan DT: Chemistry and anatomy of excita-
810
Am J Psychiatry 154:6, June 1997
BREIER, MALHOTRA, PINALS, ET AL.
36.
37. 38. 39. 40.
tory amino acid systems, in Psychopharmacology: The Third Generation of Progress. Edited by Meltzer HY. New York, Raven Press, 1987, pp 197210 Goldman PS, Rosvold HE, Vest B, Galkin TW: Analysis of the delayed-alternation deficit produced by dorsolateral prefrontal lesions in the rhesus monkey. J Comp Physiol Psychol 1971; 77: 212220 Mishkin M, Manning FJ: Nonspatial memory after selective prefrontal lesions in monkeys. Brain Res 1978; 143:313323 Liddle PF, Friston KJ, Frith CD, Hirsch SR, Jones T, Frackowiak RSJ: Patterns of cerebral blood flow in schizophrenia. Br J Psychiatry 1992; 160:179186 McGuire PK, Shah GM, Murray RM: Increased blood flow in Brocas area during auditory hallucinations in schizophrenia. Lancet 1993; 342:703706 Andreasen NC, Rezai K, Alliger R, Swayze VW II, Flaum M, Kirchner P, Cohen G, OLeary DS: Hypofrontality in neuroleptic-naive patients and in patients with chronic schizophrenia: assessment with xenon 133 single-photon emission computed
41. 42.
43.
44. 45.
tomography and the Tower of London. Arch Gen Psychiatry 1992; 49:943958 Weinberger DR, Berman KF: Speculation on the meaning of cerebral metabolic hypofrontality in schizophrenia. Schizophr Bull 1988; 14:157168 Buchsbaum MS, Haier RJ, Potkin SG, Nuechterlein K, Bracha HS, Katz M, Lohr J, Wu J, Lottenberg S, Jerabek PA, Trenary M, Tafalla R, Reynolds C, Bunney WE Jr: Frontostriatal disorder of cerebral metabolism in never-medicated schizophrenics. Arch Gen Psychiatry 1992; 49:935942 Silbersweig DA, Stern E, Frith C, Cahill C, Holmes A, Grootoonk S, Swaward J, McKenna P, Chua SE, Schnorr L: A functional neuroanatomy of hallucinations in schizophrenia. Nature 1995; 378:176179 Wolkin A, Sanfilipo M, Wolf AP, Angrist B, Brodie JD, Rotrosen J: Negative symptoms and hypofrontality in chronic schizophrenia. Arch Gen Psychiatry 1992; 49:959965 Andreasen NC: Neural mechanisms of negative symptoms. Br J Psychiatry Suppl 1989; 7:9398
Am J Psychiatry 154:6, June 1997
811
You might also like
- Psilocybin Experiments in Altered Perception of 3-D Visual Illusions As A Screening Method For Psychedelic ADocument6 pagesPsilocybin Experiments in Altered Perception of 3-D Visual Illusions As A Screening Method For Psychedelic AIxulescu HaralambieNo ratings yet
- 1034 Full PDFDocument9 pages1034 Full PDFZaki AlloucheNo ratings yet
- Wang Et Al. (1999)Document5 pagesWang Et Al. (1999)Jay CHANNo ratings yet
- Effects of Anti-Obsessional Treatment On Pituitary Volumes in Obsessive-Compulsive DisorderDocument6 pagesEffects of Anti-Obsessional Treatment On Pituitary Volumes in Obsessive-Compulsive DisorderRania Merriane DevinaNo ratings yet
- 3 Parcial An Isela ArticuloDocument11 pages3 Parcial An Isela ArticuloDaisy RomeroNo ratings yet
- Cole 2022 Stanford Neuromodulation Therapy SNDocument10 pagesCole 2022 Stanford Neuromodulation Therapy SNVictor Lopez SueroNo ratings yet
- Journal AphasiaDocument9 pagesJournal AphasiaChintya Anugrah SuhendraNo ratings yet
- Paliperidone in SchizophreniaDocument2 pagesPaliperidone in SchizophreniaTuan AnhNo ratings yet
- M. Balíková Et Al - Kinetic Profiles of Incorporation of Some Psychedelics Into Brain Tissue After Subcutaneous Application To RatsDocument6 pagesM. Balíková Et Al - Kinetic Profiles of Incorporation of Some Psychedelics Into Brain Tissue After Subcutaneous Application To RatsSmokeysamNo ratings yet
- Redlich 2020Document8 pagesRedlich 2020MARIA MONTSERRAT SOMOZA MONCADANo ratings yet
- Appi Ajp 2020 20101481Document10 pagesAppi Ajp 2020 20101481sarahNo ratings yet
- Metabolic StressDocument3 pagesMetabolic StressRoberto MartineNo ratings yet
- MICRODIALIS DE PROPOFOL Y MDZ EN TEC Tanguy2012Document6 pagesMICRODIALIS DE PROPOFOL Y MDZ EN TEC Tanguy2012rodolfo riosNo ratings yet
- Psychedelic Effects of Psilocybin Correlate With Serotonin 2A Receptor Occupancy and Plasma Psilocin LevelsDocument7 pagesPsychedelic Effects of Psilocybin Correlate With Serotonin 2A Receptor Occupancy and Plasma Psilocin LevelsnizmodranpievkaNo ratings yet
- How Psychotherapy Changes the BrainDocument5 pagesHow Psychotherapy Changes the BrainTomas SærmarkNo ratings yet
- Cerebelo en Hiperactividad y Deficit de AtencionDocument7 pagesCerebelo en Hiperactividad y Deficit de AtencionLiliann RiveraNo ratings yet
- Reduction of Motoric Agitation and Restlessness by AF102B and Tacrine in The MacaqueDocument7 pagesReduction of Motoric Agitation and Restlessness by AF102B and Tacrine in The MacaqueNadhirah Mohamad NohNo ratings yet
- BJP BP 111 097634Document9 pagesBJP BP 111 097634Alan EhrichNo ratings yet
- Cuma Abstraknya Aja: TTG Risperidone: Stroke Therapy TreatmentsDocument6 pagesCuma Abstraknya Aja: TTG Risperidone: Stroke Therapy TreatmentsChandz ChanDra ErryandariNo ratings yet
- Abnormal Regional Cerebral Blood Flow in Cognitively Normal Elderly Subjects With HypertensionDocument7 pagesAbnormal Regional Cerebral Blood Flow in Cognitively Normal Elderly Subjects With HypertensionAminarsihNo ratings yet
- Citicoline Improved Cardiac Function in Dysautonomia ModelDocument12 pagesCiticoline Improved Cardiac Function in Dysautonomia ModelShaimaa NasrNo ratings yet
- Dopamina e GagueiraDocument5 pagesDopamina e GagueiraMaisa Tatiana CasarinNo ratings yet
- Circuito de RecompensaDocument7 pagesCircuito de RecompensaColo VoltaNo ratings yet
- Psilocybin Assisted Therapy A Review of A Novel Treatment For Psychiatric DisordersDocument11 pagesPsilocybin Assisted Therapy A Review of A Novel Treatment For Psychiatric DisordersJuanmaNo ratings yet
- Cannabis Analgesia Altered Brain ConnectivityDocument11 pagesCannabis Analgesia Altered Brain ConnectivityMarcus Vinícius SouzaNo ratings yet
- efficassy and safety of tDCSDocument2 pagesefficassy and safety of tDCSlabsoneducationNo ratings yet
- 5 - Aerobic Exercise Alters Brain Function and Structure in Parkinson's Disease A Randomized Controlled TrialDocument14 pages5 - Aerobic Exercise Alters Brain Function and Structure in Parkinson's Disease A Randomized Controlled TrialGabriel NevesNo ratings yet
- Neuromodulation For Addiction 082209Document9 pagesNeuromodulation For Addiction 082209hellno1234100% (1)
- HD Psychiatry 2Document7 pagesHD Psychiatry 2annaNo ratings yet
- Bear&KirkwoodDocument11 pagesBear&KirkwoodswagatarcNo ratings yet
- This Week in The Journal: Cellular/MolecularDocument1 pageThis Week in The Journal: Cellular/Moleculartrilok1508No ratings yet
- Baba Et Al. - 2017 - Longitudinal Study of Cognitive and Cerebral Metabolic Changes in Parkinson's DiseaseDocument6 pagesBaba Et Al. - 2017 - Longitudinal Study of Cognitive and Cerebral Metabolic Changes in Parkinson's DiseaseAleja ToPaNo ratings yet
- Chronic Stress Changes Prepulse Inhibition After Amphetamine Challenge: The Role of The Dopaminergic SystemDocument13 pagesChronic Stress Changes Prepulse Inhibition After Amphetamine Challenge: The Role of The Dopaminergic SystemArlette CárdenasNo ratings yet
- Research Article: Neuroprotective Effects of Cistanches Herba Therapy On Patients With Moderate Alzheimer's DiseaseDocument13 pagesResearch Article: Neuroprotective Effects of Cistanches Herba Therapy On Patients With Moderate Alzheimer's DiseaseVeronica Yosita AnandaNo ratings yet
- Cerebral Correlates of Autonomic Cardiovascular Arousal: A Functional Neuroimaging Investigation in HumansDocument12 pagesCerebral Correlates of Autonomic Cardiovascular Arousal: A Functional Neuroimaging Investigation in Humansbdalcin5512No ratings yet
- NMDA Receptor Hypofunction Produces Concomitant Firing Rate Potentiation and Burst Activity Reduction in The Prefrontal CortexDocument6 pagesNMDA Receptor Hypofunction Produces Concomitant Firing Rate Potentiation and Burst Activity Reduction in The Prefrontal CortexCortate15gNo ratings yet
- Jurnal Yang DigunakanDocument6 pagesJurnal Yang DigunakanTrisna Trisna TrisnaNo ratings yet
- BV2 Publikacja Final Version 06.02.22 for SendingDocument11 pagesBV2 Publikacja Final Version 06.02.22 for SendingEwelina HonkiszNo ratings yet
- Mechanism of Amyloid Removal in Patients With Gantenerumab (Roche Mab) - Oct 2011Document10 pagesMechanism of Amyloid Removal in Patients With Gantenerumab (Roche Mab) - Oct 2011sckeddyNo ratings yet
- 28sici 291097 4547 2819961101 2946 3A3 3C316 3A 3aaid jnr4 3e3.0.co 3B2 NDocument8 pages28sici 291097 4547 2819961101 2946 3A3 3C316 3A 3aaid jnr4 3e3.0.co 3B2 NLata DeshmukhNo ratings yet
- Reduced Daytime Activity in Patients With Acquired Brain Damage and Apathy: A Study With Ambulatory ActigraphyDocument4 pagesReduced Daytime Activity in Patients With Acquired Brain Damage and Apathy: A Study With Ambulatory ActigraphySara GRNo ratings yet
- Esearch Rticle: Requirement of Hippocampal Neurogenesis For The Behavioral Effects of AntidepressantsDocument5 pagesEsearch Rticle: Requirement of Hippocampal Neurogenesis For The Behavioral Effects of AntidepressantsMariana JuncoNo ratings yet
- MaybergetalAJP 99Document8 pagesMaybergetalAJP 99Sharon AdeleNo ratings yet
- Effect of Chronic High-Dose Exogenous Cortisol On Hippocampal Neuronal Number in Aged Nonhuman PrimatesDocument6 pagesEffect of Chronic High-Dose Exogenous Cortisol On Hippocampal Neuronal Number in Aged Nonhuman PrimatesFrontiersNo ratings yet
- Different Effects of Typical and Atypical Antipsychotics on Grey Matter in First Episode Psychosis: the ÆSOP StudyDocument10 pagesDifferent Effects of Typical and Atypical Antipsychotics on Grey Matter in First Episode Psychosis: the ÆSOP StudyVictorson Leonardo ZegaNo ratings yet
- Beauregard Paquette2006Document4 pagesBeauregard Paquette2006felix pastorNo ratings yet
- Advances in Understanding and Treating Mental Illness: Proceedings of The 40th Canadian College of Neuropsychopharmacology Annual Meeting SymposiaDocument6 pagesAdvances in Understanding and Treating Mental Illness: Proceedings of The 40th Canadian College of Neuropsychopharmacology Annual Meeting Symposiareynolds.lauNo ratings yet
- PET Imaging Predicts Future Body Weight and Cocaine PreferenceDocument11 pagesPET Imaging Predicts Future Body Weight and Cocaine PreferenceDaniel DíazNo ratings yet
- Carhart-Harris - Neural Correlates of The Psychedelic State As Determined by fMRI Studies With PsilocybinDocument6 pagesCarhart-Harris - Neural Correlates of The Psychedelic State As Determined by fMRI Studies With PsilocybinEckart ZimmermannNo ratings yet
- Psilocybin For Treatment Resistent DepressionDocument11 pagesPsilocybin For Treatment Resistent DepressionVania M. PatdNo ratings yet
- Parkinson Subtypes Progress Differently PDFDocument8 pagesParkinson Subtypes Progress Differently PDFParisNo ratings yet
- Cannabis Paper 9Document11 pagesCannabis Paper 9Carlos Eduardo Jorquera GonzálezNo ratings yet
- Preller Et Al., 2013Document10 pagesPreller Et Al., 2013Daniel Santos CarrascoNo ratings yet
- Decreased Serotonin 2A Receptor Densities in Neuroleptic-Naive Patients With Schizophrenia: A PET Study Using (F) SetoperoneDocument3 pagesDecreased Serotonin 2A Receptor Densities in Neuroleptic-Naive Patients With Schizophrenia: A PET Study Using (F) SetoperoneCortate15gNo ratings yet
- Mus 61 26Document10 pagesMus 61 26CarlosErnestoBolañosAlmeidaNo ratings yet
- Brem 2020Document15 pagesBrem 2020Bianca Silva PintoNo ratings yet
- 2003 - Melissa Officinalis Extract in The Treatment of Patients With Mild To Moderate AlzheimerDocument4 pages2003 - Melissa Officinalis Extract in The Treatment of Patients With Mild To Moderate AlzheimerVinicius LayatteNo ratings yet
- Out 8Document10 pagesOut 8tofanNo ratings yet
- The Endocannabinoid System: Genetics, Biochemistry, Brain Disorders, and TherapyFrom EverandThe Endocannabinoid System: Genetics, Biochemistry, Brain Disorders, and TherapyNo ratings yet
- Fundamentals and Clinics of Deep Brain Stimulation: An Interdisciplinary ApproachFrom EverandFundamentals and Clinics of Deep Brain Stimulation: An Interdisciplinary ApproachYasin TemelNo ratings yet
- Ivan Izquierdo Et Al - Different Molecular Cascades in Different Sites of The Brain Control Memory ConsolidationDocument10 pagesIvan Izquierdo Et Al - Different Molecular Cascades in Different Sites of The Brain Control Memory ConsolidationCortate15gNo ratings yet
- Daniel O. Kellett Et Al - Memory Consolidation in The Cerebellar CortexDocument13 pagesDaniel O. Kellett Et Al - Memory Consolidation in The Cerebellar CortexCortate15gNo ratings yet
- John D. Heiss Et Al - Image-Guided Convection-Enhanced Delivery of Muscimol To The Primate BrainDocument13 pagesJohn D. Heiss Et Al - Image-Guided Convection-Enhanced Delivery of Muscimol To The Primate BrainCortate15gNo ratings yet
- Justin A. Harris and R. Fred Westbrook - Evidence That GABA Transmission Mediates Context-Specific Extinction of Learned FearDocument11 pagesJustin A. Harris and R. Fred Westbrook - Evidence That GABA Transmission Mediates Context-Specific Extinction of Learned FearCortate15gNo ratings yet
- Doris D.Wang and Arnold R. Kriegstein - Defining The Role of GABA in Cortical DevelopmentDocument7 pagesDoris D.Wang and Arnold R. Kriegstein - Defining The Role of GABA in Cortical DevelopmentCortate15gNo ratings yet
- Inhibitory: Central Effects of Muscimol and Bicuculline The Milk Ejection Reflex The AnaesthetizedDocument15 pagesInhibitory: Central Effects of Muscimol and Bicuculline The Milk Ejection Reflex The AnaesthetizedCortate15gNo ratings yet
- Characterization and Pharmacological Applications of A New TechniqueDocument14 pagesCharacterization and Pharmacological Applications of A New TechniqueCortate15gNo ratings yet
- Ronald A. Ruden - Why Tapping Works: Speculations From The Observable BrainDocument14 pagesRonald A. Ruden - Why Tapping Works: Speculations From The Observable BrainCortate15gNo ratings yet
- Michael Andang Et Al - Histone H2AX-dependent GABA-A Receptor Regulation of Stem Cell ProliferationDocument6 pagesMichael Andang Et Al - Histone H2AX-dependent GABA-A Receptor Regulation of Stem Cell ProliferationCortate15gNo ratings yet
- John D. Heiss Et Al - Local Distribution and Toxicity of Prolonged Hippocampal Infusion of MuscimolDocument11 pagesJohn D. Heiss Et Al - Local Distribution and Toxicity of Prolonged Hippocampal Infusion of MuscimolCortate15gNo ratings yet
- Miller & Urcelay, 2007Document2 pagesMiller & Urcelay, 2007gonurcelayNo ratings yet
- Matthew R. Holahan and Norman M. White - Intra-Amygdala Muscimol Injections Impair Freezing and Place Avoidance in Aversive Contextual ConditioningDocument12 pagesMatthew R. Holahan and Norman M. White - Intra-Amygdala Muscimol Injections Impair Freezing and Place Avoidance in Aversive Contextual ConditioningCortate15gNo ratings yet
- Yoshihiro Matsushima Et Al - Historical Overview of Psychoactive MushroomsDocument12 pagesYoshihiro Matsushima Et Al - Historical Overview of Psychoactive MushroomsCortate15g100% (1)
- Ian D. Tomlinson Et Al - Imaging GABA-c Receptors With Ligand-Conjugated Quantum DotsDocument9 pagesIan D. Tomlinson Et Al - Imaging GABA-c Receptors With Ligand-Conjugated Quantum DotsCortate15gNo ratings yet
- Stephan F. de Borhegyi - Miniature Mushroom Stones From GuatemalaDocument8 pagesStephan F. de Borhegyi - Miniature Mushroom Stones From GuatemalaCortate15gNo ratings yet
- Michael S. Nicholson - Some Spiritualistic Uses of MushroomsDocument2 pagesMichael S. Nicholson - Some Spiritualistic Uses of MushroomsCortate15gNo ratings yet
- Sachidananda Padhy and Santosh Kumar Dash - The Soma Drinker of Ancient India: An Ethno-Botanical RetrospectionDocument7 pagesSachidananda Padhy and Santosh Kumar Dash - The Soma Drinker of Ancient India: An Ethno-Botanical RetrospectionCortate15gNo ratings yet
- Scott Hajicek-Dobberstein - Soma Siddhas and Alchemical Enlightenment: Psychedelic Mushrooms in Buddhist TraditionDocument20 pagesScott Hajicek-Dobberstein - Soma Siddhas and Alchemical Enlightenment: Psychedelic Mushrooms in Buddhist TraditionCortate15gNo ratings yet
- Amanita Muscaria Herb of ImmortalityDocument134 pagesAmanita Muscaria Herb of Immortalitycorbugabriel8448100% (4)
- Binding Pirenzepine Digitonin-Solubilized: The Muscarinic AcetylcholineDocument10 pagesBinding Pirenzepine Digitonin-Solubilized: The Muscarinic AcetylcholineCortate15gNo ratings yet
- Geraline C. Lin and Richard A. Glennon - Hallucinogens: An UpdateDocument317 pagesGeraline C. Lin and Richard A. Glennon - Hallucinogens: An UpdateCortate15gNo ratings yet
- Chi Shing Sum Et Al - Effects of N-Ethylmaleimide On Conformational Equilibria in Purified Cardiac Muscarinic ReceptorsDocument16 pagesChi Shing Sum Et Al - Effects of N-Ethylmaleimide On Conformational Equilibria in Purified Cardiac Muscarinic ReceptorsCortate15gNo ratings yet
- John L. Waddington - Invited Commentaries On: Obstetric Complications and Schizophrenia/affective PsychosesDocument4 pagesJohn L. Waddington - Invited Commentaries On: Obstetric Complications and Schizophrenia/affective PsychosesCortate15gNo ratings yet
- Lilly Research Laboratories, Eli Lilly & Company, Indianapolis, IndianaDocument9 pagesLilly Research Laboratories, Eli Lilly & Company, Indianapolis, IndianaCortate15gNo ratings yet
- Javier Gonzalez-Maeso Et Al - Hallucinogens Recruit Specific Cortical 5-HT2A Receptor-Mediated Signaling Pathways To Affect BehaviorDocument14 pagesJavier Gonzalez-Maeso Et Al - Hallucinogens Recruit Specific Cortical 5-HT2A Receptor-Mediated Signaling Pathways To Affect BehaviorJunmajNo ratings yet
- Ionotropic Glutamate Receptors and Expression of N-Methyl - Aspartate Receptor Subunits in Subregions of Human Hippocampus: Effects of SchizophreniaDocument9 pagesIonotropic Glutamate Receptors and Expression of N-Methyl - Aspartate Receptor Subunits in Subregions of Human Hippocampus: Effects of SchizophreniaCortate15gNo ratings yet
- D.M. Weiner Et Al - 5-Hydroxytryptamine2A Receptor Inverse Agonists As AntipsychoticsDocument9 pagesD.M. Weiner Et Al - 5-Hydroxytryptamine2A Receptor Inverse Agonists As AntipsychoticsCortate15gNo ratings yet
- Javier González-Maeso Et Al - Identification of A Novel Serotonin/Glutamate Receptor Complex Implicated in PsychosisDocument12 pagesJavier González-Maeso Et Al - Identification of A Novel Serotonin/Glutamate Receptor Complex Implicated in PsychosisCortate15gNo ratings yet
- Activation of Medial Prefrontal Cortex by Phencyclidine Is Mediated Via A Hippocampo-Prefrontal PathwayDocument7 pagesActivation of Medial Prefrontal Cortex by Phencyclidine Is Mediated Via A Hippocampo-Prefrontal PathwayCortate15gNo ratings yet
- Activity No. 5 Capacitive Circuit ObjectivesDocument4 pagesActivity No. 5 Capacitive Circuit ObjectivesJohn Paul BaquiranNo ratings yet
- Effect of Bond Administration On Construction Project DeliveryDocument7 pagesEffect of Bond Administration On Construction Project DeliveryOlefile Mark MolokoNo ratings yet
- Connective TissueDocument6 pagesConnective TissuecrtgyhujikNo ratings yet
- Live load and wind pressure on sloping roofsDocument11 pagesLive load and wind pressure on sloping roofsAbel BerhanemeskelNo ratings yet
- 100 People Who Changed History and The WorldDocument400 pages100 People Who Changed History and The WorldManjunath.RNo ratings yet
- Binder Modul WMS 10Document52 pagesBinder Modul WMS 10sandhiakhmadNo ratings yet
- Proportional Chopper Amplifier VB-3A: Min MaxDocument5 pagesProportional Chopper Amplifier VB-3A: Min MaxryujoniNo ratings yet
- Calculation For Short Circuit Current Calculation Using IEC / IEEE StandardDocument11 pagesCalculation For Short Circuit Current Calculation Using IEC / IEEE StandardibmmoizNo ratings yet
- BHEL Turbine ManualDocument58 pagesBHEL Turbine Manualnivasssv75% (4)
- 34a65 PDFDocument33 pages34a65 PDFvinu100% (2)
- Unit 6 - Quantitative Analysis NotesDocument53 pagesUnit 6 - Quantitative Analysis Notesapi-182809945No ratings yet
- Unit - L: List and Explain The Functions of Various Parts of Computer Hardware and SoftwareDocument50 pagesUnit - L: List and Explain The Functions of Various Parts of Computer Hardware and SoftwareMallapuram Sneha RaoNo ratings yet
- NCERT: Why Is Steel More Elastic Than Rubber?Document7 pagesNCERT: Why Is Steel More Elastic Than Rubber?Satyam RaiNo ratings yet
- ETABS Building Structure Analysis and Design ReportDocument84 pagesETABS Building Structure Analysis and Design ReportMd Awesshadab0% (1)
- Nov. AbwDocument50 pagesNov. Abwjbyarkpawolo70No ratings yet
- Analysis of Rack and Pinion Using AnsysDocument21 pagesAnalysis of Rack and Pinion Using AnsysTejas Prakash100% (1)
- Brake SystemDocument19 pagesBrake SystemSudarshan NepalNo ratings yet
- Auditing The Usage of Therapeutic Footwear in Diabetic Foot Patients Through Amit Jain's Extended SCC' Classification For Therapeutic FootwearDocument6 pagesAuditing The Usage of Therapeutic Footwear in Diabetic Foot Patients Through Amit Jain's Extended SCC' Classification For Therapeutic FootwearJosé MorenoNo ratings yet
- Thermocouple Wire Reference Guide: WWW - Omega.co - Uk +44 (0) 161 777 6611 WWW - Omega.co - Uk +44 (0) 161 777 6611Document1 pageThermocouple Wire Reference Guide: WWW - Omega.co - Uk +44 (0) 161 777 6611 WWW - Omega.co - Uk +44 (0) 161 777 6611Mohamed MaltiNo ratings yet
- Flutek Swing MotorDocument2 pagesFlutek Swing Motorsunil0081No ratings yet
- Introduction To Business Statistics: ProbabilityDocument2 pagesIntroduction To Business Statistics: ProbabilityNghĩa PhùngNo ratings yet
- Pioneer Deh-1300 1350 1390mpDocument71 pagesPioneer Deh-1300 1350 1390mpJorge LavezziNo ratings yet
- Debating Deponency: Its Past, Present, and Future in New Testament Greek StudiesDocument32 pagesDebating Deponency: Its Past, Present, and Future in New Testament Greek StudiesSeth BrownNo ratings yet
- QAP - LT Panel PDFDocument8 pagesQAP - LT Panel PDFAkshay Ajay100% (2)
- Essay For Villa Savoye AbstractDocument1 pageEssay For Villa Savoye AbstractFrancis PohNo ratings yet
- Ukur KadasterDocument21 pagesUkur KadasterMuhammad NajmiNo ratings yet
- DebugDocument14 pagesDebugMigui94No ratings yet
- Solution to Tutorials 1-4: Shock Absorber, Crane, SDOF Vibration, Landing GearDocument19 pagesSolution to Tutorials 1-4: Shock Absorber, Crane, SDOF Vibration, Landing GearPearlyn Tiko TeoNo ratings yet
- Water Pinch PresentationDocument14 pagesWater Pinch PresentationDafiMaboNo ratings yet
- Welding Machine CatalogueDocument12 pagesWelding Machine CatalogueRodney LanagNo ratings yet