Professional Documents
Culture Documents
66 69
Uploaded by
Islam ElmahdiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
66 69
Uploaded by
Islam ElmahdiCopyright:
Available Formats
Journal of Nepal Dental Association (2010), Vol. 11, No. 1, Jan.-Jun.
, 66-69
Case Note
Unicystic ameloblastoma: Mimicking a cyst
Dandekar RC1, Shankar AA2
1
Professor & Head, 2Post Graduate Student, Department of Oral Pathology & Microbiology, M. A. Rangoonwala Dental College, 2390-B, K. B. Hidayatullah Road, Azam Campus, Camp, Pune
Abstract A 17 year old patient reported with a swelling in the left posterior mandibular region since 3 months. On clinical examination, the swelling was well-circumscribed and extended from the ala-tragus line to lower border of the mandible on the left side. It was hard and tender on palpation. Radiographic examination revealed a unilocular appearance and was suggestive of a cyst or tumour. An aspirate of the uid was obtained, and protein analysis revealed 4.3 gm/dl, suggesting a keratinizing cyst/tumor. The entire lesion was excised leaving the condyle in position, upto the mental foramen. An iliac crest graft, 10cm in length, was placed, and the mandible reconstructed. The nal histopathological diagnosis was given as Unicystic Ameloblastoma. Key words: Ameloblastoma, Vicker and Gorlin
Introduction Ameloblastoma is usually unicentric, nonfunctional, intermittent in growth, anatomically benign and clinically persistent1. It is a true neoplasm of the enamel organ type tissue, but does not undergo differentiation upto the point of enamel formation2. There are various varieties of ameloblastoma, viz. follicular, plexiform, acanthomatous, granular and unicentric. The follicular, plexiform and unicentric variety are the most common varieties, and may co-exist in the same specimen. The usual presenting age of an ameloblastoma is considered to be in the 3rd and 4th decades with a predilection for Asian population. The unicystic ameloblastoma is a well-dened, often large monocystic cavity with a lining, focally but rarely entirely composed of odontogenic epithelium3. It is histopathologically divided into intracystic, luminal or intraluminal unicystic ameloblastoma. Also, tumours associated with an unerupted tooth are considered to be the dentigerous variant, whereas those lacking an association with an unerupted tooth were considered to be the nondentigerous variant. The dentigerous variety is known to occur in younger patients.
Case report A 17 year old male presented with pain and discomfort in the left posterior mandibular region. A swelling present in the lower left region, extending from the left ala-tragus line to the lower border of mandible was noted (Fig 1), and was found to be hard on palpation. Disgurement and asymmetry of the face were evident. Intraoral examination revealed a missing lower left second molar tooth (Fig 2). The radiographic ndings showed a multilocular radiolucency extending from the molar to the condyle region (Fig 3). The inferior border of the mandible could not be traced well. A computed tomography scan revealed a tooth in association with the lesion (Fig 4). The entire tumor was removed in toto. A gross examination of the lesion showed a smooth cyst wall, without any perforations (Fig 5). A tooth was noted in association with the lesion, but did not seem to be part of the lesion (Fig 6). A detailed histopathological examination was carried out. The slides were stained with routine H&E stain. The
Correspondence Dr. Akhil A. Shankar, Post Graduate Student, Department of Oral Pathology & Microbiology, M. A. Rangoonwala Dental College, 2390-B, K. B. Hidayatullah Road, Azam Campus, Camp, Pune - 411001, E-mail: akhil1904@hotmail.com
J. Nepal Dent. Assoc. (2010), Vol. 11, No. 1
66
histopathology showed a cystic lining with the basal cells displaying a palisading appearance. Hyalinization of the subjacent connective tissue capsule was noted at places (Fig 7). A higher magnication showed hyperchromatic nuclei in cuboidal to columnar basal cells. The supercial epithelium showed prominent intracellular spacing, creating a stellate reticulum like appearance (Fig 8 & Fig 9). The above features in relation to the radiographic ndings were suggestive of a Unicystic Ameloblastoma type 1.2.
Table 1: Histologic Unicystic Ameloblastoma Subgrouping by Ackermann et al Subgroup Interpretation 1 1.2 1.2.3 1.3 Luminal UA Luminal and Intraluminal UA Luminal, Intraluminal, and Intramural UA Luminal and Intraluminal UA
Fig 2: Absence of lower left second molar
Fig 1: Swelling of the mandible on the left side (arrows)
Fig 3: OPG image showing a multilocular radiolucency
Fig 4: CT shows tooth in association with lesion (arrow)
67
J. Nepal Dent. Assoc. (2010), Vol. 11, No. 1
Fig 5: Gross specimen smooth cystic walls
Fig 6: Impacted tooth, outside the lesion
Fig 7: Palisaded basal cells and hyalinization of the subjacent connective tissue
Fig 8: Hyperchromatic nuclei in basal columnar cells
Fig 9: Stellate reticulum like appearance of supercial cells
Fig 10: Types of growth in Unicystic Ameloblastoma 1. Luminal, 2. Intraluminal, 3. Intramural
Discussion The ameloblastoma is the second most commonly occurring odontogenic tumor after the odontoma2, and 80 per cent of all cases occur in the molar-ramus region. The term Ameloblastoma was suggested by Churchill in 1934. It is known to occur equally in both sexes and aficts patients mainly in the 3rd to 5th decade. There are almost upto fteen different types of this tumour
recorded till date3. The most commonly occurring varieties of this tumour histologically are follicular, plexiform, granular, desmoplastic, basal cell, unicystic and the lesser occurring peripheral variant. The other variants of the tumour are acanthomatous, clear cell, keratoameloblastoma, mucous cell differentiation and hemangiomatous. The surgical management of these
J. Nepal Dent. Assoc. (2010), Vol. 11, No. 1
68
tumours essentially remains the same and primarily differs for the Unicystic variety. The unicystic ameloblastoma was rst dened as Robinson and Martinez in 19774. The frequency of these tumours is reported to be between 5% and 22% of all types of ameloblastomas5. An age old debate for the pathogenesis of this lesion still prevails. Three mechanisms have been proposed for the development of the unicystic ameloblastoma6: 1. The reduced enamel epithelium associated with a developing tooth undergoes ameloblastic transformation with subsequent cystic development 2. Ameloblastomas arise in dentigerous or other types of odontogenic cysts in which the neoplastic ameloblastic epithelium is preceded temporarily by a non-neoplastic stratied squamous epithelial lining 3. A solid ameloblastoma undergoes cystic degeneration of ameloblastic islands with subsequent fusion of multiple microcysts and develops into a cystic lesion. The fact that the PCNA-positive cells are signicantly higher as compared to that of the dentigerous cyst linings suggests that this tumor arises de novo. One complication known to arise from dentigerous cysts is its transformation to ameloblastomas. Although a highly argued topic, yet as given by Vicker and Gorlin7, the following points are used to distinguish UA from any other cystic lesion: 1. Epithelial lining parts may show transformation to cuboidal or columnar basal cells with hyperchromatic nuclei 2. Nuclear palisading with polarization 3. Cytoplasmic vacuolation with intercellular spacing 4. Subepithelial hyalinization The above mentioned ndings conrmed with those seen in our case.
Ackermann et al8 have provided a histological subgrouping of the Unicystic Ameloblastoma as shown in Table 1 and a diagrammatic representation of the same shown in Fig. 10. Based on the above classication, our case was given a subgroup of 1.2. From a surgical aspect, the tumour under the subgroup class 1 can be enucleated and the jawbone salvaged, provided it is salvageable. A higher subgroup requires the surgery as always performed for any other ameloblastoma, which might vary from segmental resection to hemimandibulectomy, depending on the size of the lesion, and also the amount of bone remaining. A hemimandibulectomy with reconstruction was carried out in this case. References
1. Robinson HBG. Proceedings of the Fifth Annual Meeting of the American Academy of Oral Pathology. Oral Surg 1952;5:177-8. R Rajendran, B Sivapathasundharam. Shafers Textbook of Oral Pathology. 5th Edn. Elsevier. New Delhi. 2007. pp 381-390. Reichart PA, Philipsen HP. Odontogenic Tumours and Allied Lesions. 1st Edn. Quintessance Publishing. New Delhi. 2004. pp 77-86. Robinson L, Martinez MG. Unicystic Ameloblastoma. A prognostically distince entity. Cancer 1977;40:22782285. Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: Biological prole of 3677 cases. Eur J Cancer B Oral Oncol 31B:86-99. 1995. Leider AS, Eversole LR, Barkin ME. Cystic Ameloblastoma. Oral Surg Oral Med Oral Pathol 1985;60:624-630. Vickers RA, Gorlin RJ. Ameloblastoma: Delineation of early histopathological features of neoplasia. Cancer 1970;26:699-710. Ackermann GL, Altini M, Shear M. The unicystic ameloblastoma: A clinicopathologic study of 57 cases. J Oral Pathol 1988;17:541-546.
2.
3.
4.
5.
6. 7.
8.
69
J. Nepal Dent. Assoc. (2010), Vol. 11, No. 1
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
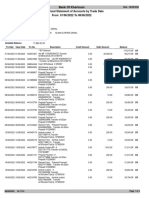
- Summarized Statement of Accounts by Trade Date From 01/06/2022 To 08/08/2022Document6 pagesSummarized Statement of Accounts by Trade Date From 01/06/2022 To 08/08/2022Islam ElmahdiNo ratings yet
- Manual 000004058Document7 pagesManual 000004058Islam ElmahdiNo ratings yet
- Manual 000004058Document7 pagesManual 000004058Islam ElmahdiNo ratings yet
- Dental Home FinalDocument2 pagesDental Home FinalIslam ElmahdiNo ratings yet
- How To Receive and Give FeedbackDocument4 pagesHow To Receive and Give FeedbackIslam ElmahdiNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Aacra Draft Preliminary Report PDFDocument385 pagesAacra Draft Preliminary Report PDFBeselam SeyedNo ratings yet
- JK Paper Q4FY11 Earnings Call TranscriptDocument10 pagesJK Paper Q4FY11 Earnings Call TranscriptkallllllooooNo ratings yet
- Life of A Landfill PumpDocument50 pagesLife of A Landfill PumpumidNo ratings yet
- Pitch Manual SpecializedDocument20 pagesPitch Manual SpecializedRoberto Gomez100% (1)
- Reinforced Concrete Beam DesignDocument13 pagesReinforced Concrete Beam Designmike smithNo ratings yet
- Maintenance Handbook On Compressors (Of Under Slung AC Coaches) PDFDocument39 pagesMaintenance Handbook On Compressors (Of Under Slung AC Coaches) PDFSandeepNo ratings yet
- Henry Stevens - Hitler's Flying Saucers - A Guide To German Flying Discs of The Second World War New Edition (2013, Adventures Unlimited Press) - Libgen - lc-116-120Document5 pagesHenry Stevens - Hitler's Flying Saucers - A Guide To German Flying Discs of The Second World War New Edition (2013, Adventures Unlimited Press) - Libgen - lc-116-120sejoh34456No ratings yet
- Acuity Assessment in Obstetrical TriageDocument9 pagesAcuity Assessment in Obstetrical TriageFikriNo ratings yet
- Laser Surface Treatment ProcessesDocument63 pagesLaser Surface Treatment ProcessesDIPAK VINAYAK SHIRBHATENo ratings yet
- CIRC 314-AN 178 INP EN EDENPROD 195309 v1Document34 pagesCIRC 314-AN 178 INP EN EDENPROD 195309 v1xloriki_100% (1)
- 2 - Soil-Only Landfill CoversDocument13 pages2 - Soil-Only Landfill Covers齐左No ratings yet
- O2 Orthodontic Lab Catalog PDFDocument20 pagesO2 Orthodontic Lab Catalog PDFplayer osamaNo ratings yet
- Emerson EPC48150 1800 FA1EPC48300 3200 FA1 V PDFDocument26 pagesEmerson EPC48150 1800 FA1EPC48300 3200 FA1 V PDFRicardo Andrés Soto Salinas RassNo ratings yet
- 07.03.09 Chest Physiotherapy PDFDocument9 pages07.03.09 Chest Physiotherapy PDFRakesh KumarNo ratings yet
- Pharmacokinetics and Drug EffectsDocument11 pagesPharmacokinetics and Drug Effectsmanilyn dacoNo ratings yet
- House Designs, QHC, 1950Document50 pagesHouse Designs, QHC, 1950House Histories100% (8)
- Evolutionary PsychologyDocument10 pagesEvolutionary PsychologyShreya MadheswaranNo ratings yet
- 1"a Study On Employee Retention in Amara Raja Power Systems LTDDocument81 pages1"a Study On Employee Retention in Amara Raja Power Systems LTDJerome Samuel100% (1)
- Chapter 16 - Energy Transfers: I) Answer The FollowingDocument3 pagesChapter 16 - Energy Transfers: I) Answer The FollowingPauline Kezia P Gr 6 B1No ratings yet
- KINETIC THEORY OF GASES TUTORIALDocument6 pagesKINETIC THEORY OF GASES TUTORIALMat SyafiqNo ratings yet
- Interactive Architecture Adaptive WorldDocument177 pagesInteractive Architecture Adaptive Worldhoma massihaNo ratings yet
- Organizing Small Items with Glass Bottle OrganizersDocument70 pagesOrganizing Small Items with Glass Bottle OrganizersDy SaiNo ratings yet
- Telco XPOL MIMO Industrial Class Solid Dish AntennaDocument4 pagesTelco XPOL MIMO Industrial Class Solid Dish AntennaOmar PerezNo ratings yet
- Flowing Gas Material BalanceDocument4 pagesFlowing Gas Material BalanceVladimir PriescuNo ratings yet
- Virchow TriadDocument6 pagesVirchow Triadarif 2006No ratings yet
- Railway Airport Docks and HarbourDocument21 pagesRailway Airport Docks and HarbourvalarmathibalanNo ratings yet
- De Thi HSG Tinh Binh PhuocDocument9 pagesDe Thi HSG Tinh Binh PhuocDat Do TienNo ratings yet
- ML AiDocument2 pagesML AiSUYASH SHARTHINo ratings yet
- WL 318 PDFDocument199 pagesWL 318 PDFBeckty Ahmad100% (1)
- Hyperbaric WeldingDocument17 pagesHyperbaric WeldingRam KasturiNo ratings yet