83% found this document useful (6 votes)
9K views53 pagesMacular Function Tests Overview
My 2nd PG presentation.Its colourful...purpose to stimulate all ur cones and the 1rst picture u would find beautiful if ur MFT is normal!
Uploaded by
pushpanjali ramtekeCopyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
83% found this document useful (6 votes)
9K views53 pagesMacular Function Tests Overview
My 2nd PG presentation.Its colourful...purpose to stimulate all ur cones and the 1rst picture u would find beautiful if ur MFT is normal!
Uploaded by
pushpanjali ramtekeCopyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
- Macular Function Test: The cover page provides the title of the presentation, indicating the focus on macular function testing.
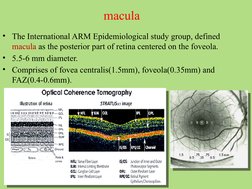
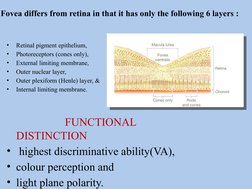
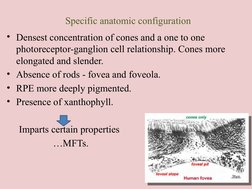
- Macular Anatomy: Discusses the macula's definition, size, and composition with images of retinal structure.
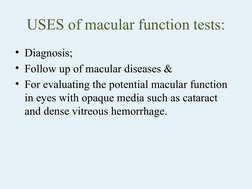
- Uses of Macular Function Tests: Explains the diagnostic and evaluative purposes of macular function tests for conditions like cataracts.
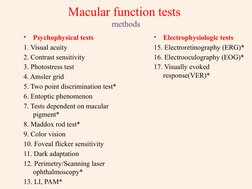
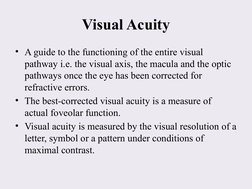
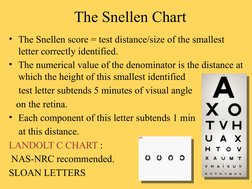
- Macular Function Test Methods: Lists various types of macular function tests, including psychophysical and electrophysiologic methods.
- Clinical Electrophysiologic Tests: Explores tests like ERG, EOG, and the VER related to retinal and visual response to stimuli.
- Thank You: Concludes the presentation, marking the end of the document.