Intestinal Obstruction
Basics
DESCRIPTION
Pathologic blockage of progression of intestinal contents:
1. May be partial or complete
2. May arise from intrinsic abnormalities (e.g., meconium ileus or intestinal atresia) or extrinsic
abnormalities (e.g., adhesions and volvulus).
Paralytic ileus: Failure of intestinal motor function without mechanical obstruction:
1. Very common after abdominal operations.
2. Common causes:
Infection (pneumonia, gastroenteritis, peritonitis, systemic sepsis)
Drugs (i.e., opiates, loperamide, vincristine)
Metabolic abnormalities (hypokalemia, uremia, myxedema, and diabetic ketoacidosis)
Chronic intestinal pseudo-obstruction: A severe intestinal motility disorder described in diverse diseases including
muscular, endocrine, metabolic and autoimmune disorders. Examples include Duchenne and diabetes mellitus.
EPIDEMIOLOGY
The different causes have their own identified epidemiologic patterns:
Postoperatve adhesions occur very often after all laparotomies
Small bowel obstruction secondary to Ascaris lumbricoides in tropical and subtropical countries
Colonic volvulus secondary to aerophagia and constipation in mentally retarded children
Meconium ileus equivalent in children with cystic fibrosis
Incidence
Occurs in ~1 in 1,500 live births
BASICS-EPIDEMIOLOGY-Prevalence
Down syndrome (with a high prevalence, 2030%, of duodenal atresia)
PATHOPHYSIOLOGY
Mechanical obstruction:
1. Intestinal contents accumulate proximal to the site of obstruction.
2. The bowel distends with swallowed air, ingested food, secretions, and gases from intestinal reactions and
bacterial fermentation.
3. Retrograde flow of intestinal contents and reflex gut distention cause vomiting.
4. Internal and external losses result in hypovolemia, oliguria, and azotemia.
5. Bacteria proliferate in the small bowel and its contents become feculent.
Strangulation obstruction (impaired blood flow to the intestine in addition to intestinal content obstruction):
1. Loss of plasma into the bowel, leading more rapidly to shock
2. When strangulation progresses, gangrene, peritonitis, and perforation may ensue.
3. Damage to the normal gut barrier may enable bacteria, bacterial toxins, and inflammatory mediators to
enter the circulation causing sepsis
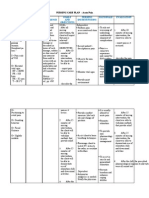
ETIOLOGY
Neonates:
1. Atresia of the intestine (33% of all neonatal obstructions, 1:2700 newborns)
2. Meconium ileus (30% of all neonatal obstructions, almost all caused by cystic fibrosis) and meconium
plug
3. Anorectal malformation: Anal atresia and stenosis (1 in 4,0008,000 newborns)
4. Necrotizing enterocolitis
5. Hirschsprung disease
Infants:
1. The most common cause of intestinal obstruction is pyloric stenosis.
2. The 2nd most common is intussusception (the most common cause between 3 months and 6 years of age,
with 60% of cases occurring before 1 year of age).
3. Other, less common causes:
Postoperative intestinal obstruction and adhesion
Incarcerated or strangulated inguinal hernia. Inguinal hernias have 1028% risk for incarceration
Hirschsprung disease
Duplications
Meckel diverticulum
Older children:
1. Malrotation
2. Annular pancreas
3. Meckel diverticulum
4. Cancer-related intestinal obstruction, and radiotherapy induced adhesions
5. Superior mesenteric artery syndrome
6. Corrosive injury-induced gastric outlet obstruction
7. Esophageal injury or foreign body ingestion (e.g., coin in esophagus)
8. Postoperative intestinal obstruction and adhesions
9. Juvenile polyposis and related syndromes (e.g., Peutz-Jeghers)
�10. Inflammatory bowel disease
11. Meconium ileus equivalent (occurs only in patients with cystic fibrosis)
12. Roundworm (A. lumbricoides)
13. Gastric and intestinal bezoars
Diagnosis
CLINICAL:
There is no spontaneous resolution of inguinal hernia. Surgery should be scheduled before incarceration occurs.
SIGNS AND SYMPTOMS
Presentation may be acute and obvious or chronic and subtle. The latter and partial obstruction could be difficult to
diagnose.
Careful history, physical examination, and consideration of age related etiology most often will identify the specific
cause.
History
The classic symptoms of intestinal obstruction include vomiting (often bile stained), abdominal distention, colicky
abdominal pain, and failure to pass stool.
In neonates:
1. History of maternal polyhydramnios and aspiration of >20 mL gastric fluid after birth are suggestive of
high intestinal obstruction.
2. Most healthy full-term children should pass meconium within 48 hours of birth. If no meconium at 48
hours, suspect obstruction
Older children:
1. Pain is one of the cardinal manifestations can be poorly localizedcolicky visceral pain or sharp peritoneal
pain.
2. Nausea and vomiting: High obstruction causes bilious emesis; distal obstruction may lead feculent emesis;
in colonic obstruction vomiting may be absent or late.
3. No passage of stool in low obstruction or bloody stool with mucus in strangulation (associated with
intussusception and volvulus).
CLINICAL:
Neonates, more so than older children, with unrecognized intestinal obstruction deteriorate rapidly, with increased
morbidity, mortality, and surgical complications.
Physical Exam
General assessment and vital signs, as the patient could be dehydrated, septic, or malnourished
Palpation may reveal the presence of a hernia, a mass suggestive of feces, or intussusception. Tenderness and
rigidity result from peritonitis.
Bowel sounds may be initially increased, but later on are decreased, occasional or absent.
Anal inspection excludes anal atresia and stenosis. Rectal examination reveals, at times, a palpable polyp or
intussusceptum and blood (overt, occult, the currant jelly typical of intussusception).
Strangulation is suspected when there is fever, tachycardia, signs of peritonitis, and severe pain that persists after
nasogastric decompression.
TESTS
LABORATORY
No laboratory studies are diagnostic.
Electrolyte abnormalities, including sodium, chloride, bicarbonate, and potassium, are necessary to identify for the
proper assessment of hydration and 3rd spacing of fluids.
High obstruction may lead to hypochloremic, hyperkalemic metabolic alkalosis.
Bowel infarction may lead to marked leukocytosis, thrombocytopenia, and metabolic acidosis.
Serum amylase and lipase should be determined to rule out pancreatitis, but they might be mildly elevated in
intestinal obstruction.
IMAGING
Plain abdominal x-rays in the supine and erect or decubitus views will identify the classic features of a gasless
abdomen, with air-fluid levels and distended loops of intestine. However, high small bowel obstruction or
strangulation obstruction may present with normal or nearly normal x-rays.
1. In small bowel obstruction: Dilated bowel, air-fluid levels without gas in the colon, and multiple dilated
loops in distal obstruction
2. Paralytic ileus may present with dilation of the small and large intestines.
3. Duodenal obstruction with double-bubble gas shadow
4. Target sign in intussusception
5. Pneumoperitoneum in perforation
6. Peritoneal calcifications in meconium peritonitis
7. Obstruction with intraluminal calcifications in rectourinary fistula, colonic aganglionosis, or intestinal
atresia
8. Right lower quadrant ground-glass appearance in meconium ileus
Ultrasonography: To identify a mass (i.e., perforated appendix), pyloric stenosis, malrotation, volvulus, or
intussusception (in which it can replace the contrast examination in combination with air enema)
CT: Small and large bowel obstruction, diagnosis of strangulation; helpful in postoperative obstruction, Crohn
disease, and neoplasms. High cost and radiation exposure make it a subject of debate in general and in younger
patients in particular
Contrast examinations:
1. Barium enema to confirm intussusception or Hirschsprung disease
2. Upper GI series to exclude malrotation or volvulus
3. Water-soluble, low osmolarity materials should be preferred (risk of perforation).
Evaluation for other associated congenital anomalies (the most frequent are cardiac and renal abnormalities) is
mandatory, as some are life threatening. Associated malformations are frequently associated with duodenal atresia
and to a lesser extent with jejunoileal atresia.
DIFFERENTIAL DIAGNOSIS
Other causes of abdominal pain and vomiting should be considered:
Appendicitis, torsion of testis or ovary, lower lobe pneumonia: Must be ruled out by history and physical
examination
Pancreatitis
Sickle cell crisis
Henoch-Schnlein purpura
Biliary colic
Lead poisoning
Acute adrenal insufficiency
Diabetic ketoacidosis
Acute intermittent porphyria
Treatment
INITIAL STABILIZATION
Hold oral intake.
Decompress the stomach by nasogastric tube.
Administer IV hydration, correct electrolyte imbalance, and ensure adequate urine output.
Identify etiology of obstruction and establish definitive repair.
Cultures and broad-spectrum antibiotics (such as cefoxitin or gentamicin and clindamycin or metronidazole in
combination) according to patients age and status
GENERAL MEASURES
In intussusception, hydrostatic or air reduction is successful in 90% of cases.
Nasogastric decompression or anti-inflammatory medication for adhesions or inflammatory strictures
Contrast-material enemas, manipulation, and direct enteral irrigation with N-acetylcysteine for uncomplicated
meconium ileus
Manual reduction of incarcerated inguinal hernia
Colonic volvulus may be treated with endoscopic decompression followed by elective bowel resection.
Endoscopic removal of foreign bodies
Paralytic ileus is usually self-limiting and resolves with conservative therapy and medication such as prokinetic
agents (metoclopramide and erythromycin).
�SPECIAL THERAPY
Conservative management with decompression by nasogastric tube and IV fluids should be initiated 1st rather than
operating in:
1. Early postoperative, partial, and recurrent adhesive obstructions
2. Necrotizing enterocolitis
3. Intussusception
4. Meconium ileus
5. Duodenal hematomas
6. Superior mesenteric artery syndrome
7. Crohn disease
Successful treatment of adhesive small bowel obstruction with gastrografin and oral medications (laxatives) has
been reported in adults.
SURGERY
Definitive treatment requires an urgent operation.
Exceptions to this rule include are the above mentioned conditions managed conservatively. However, if no
improvement within 1224 hours, surgery is advisable.
The surgical procedure is individualized according to the specific type, site, anatomy of the obstruction, and
associated conditions.
MEDICATIONS
First-Line
Pain relief
Different medications for specific disorders.
Follow-up Recommendations
EXPECTED COURSE/PROGNOSIS
Varies with different causes of intestinal obstruction, age of the patient, presence of prematurity, and associated
anomalies
Associated complications and the institution of prompt treatment influence outcome.
Short bowel syndrome continues to be a major impediment to improved survival rate; permanent parenteral
nutrition is associated with morbidity and mortality.
POSSIBLE COMPLICATIONS
May result from delayed operation:
Dehydration
Intestinal ischemia with sepsis and shock
Bowel perforation and peritonitis
Short-gut syndrome after extensive necrosis and/or resection.
Frequently Asked Questions
Q: Will my child need surgery for this problem?
A: Most likely; surgical treatment is necessary to correct the cause of intestinal obstruction, except in a few cases,
such as intussusception, pseudo-obstruction, and paralytic ileus.
Q: What is the most common cause of this problem in my 3-day-old son?
A: In an infant, the most common causes are atresias of the intestine, which are absences of the normal amount of
large or small intestine in the abdomen.