0% found this document useful (0 votes)
119 views9 pagesOverview of RNA Viruses and Diseases
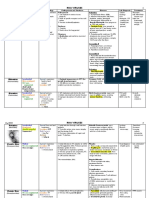
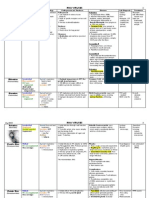
1. The document summarizes several families of RNA viruses including their characteristics, transmission, diseases caused, diagnosis, treatment and prevention. It covers double-stranded RNA viruses like Reoviridae, single-stranded RNA viruses including Arenaviridae, Bunyaviridae, Calciviridae, Coronaviridae, Filoviridae, Flaviviridae and Orthomyxoviridae.
2. The viruses are transmitted via various routes like fecal-oral, rodents, arthropod vectors, respiratory droplets and body fluids. They cause diseases ranging from gastroenteritis to hemorrhagic fever. Diagnosis involves techniques like serology, PCR, electron microscopy and
Uploaded by
baihern24Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
119 views9 pagesOverview of RNA Viruses and Diseases
1. The document summarizes several families of RNA viruses including their characteristics, transmission, diseases caused, diagnosis, treatment and prevention. It covers double-stranded RNA viruses like Reoviridae, single-stranded RNA viruses including Arenaviridae, Bunyaviridae, Calciviridae, Coronaviridae, Filoviridae, Flaviviridae and Orthomyxoviridae.
2. The viruses are transmitted via various routes like fecal-oral, rodents, arthropod vectors, respiratory droplets and body fluids. They cause diseases ranging from gastroenteritis to hemorrhagic fever. Diagnosis involves techniques like serology, PCR, electron microscopy and
Uploaded by
baihern24Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd