0% found this document useful (0 votes)
169 views37 pagesFluid Volume Impairment Lecture
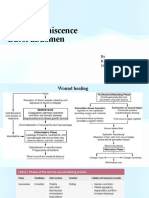
This document discusses fluid volume deficit (FVD), which occurs when there is a decrease in intravascular, interstitial, and/or intracellular fluid in the body. FVD can be caused by excessive fluid losses, insufficient intake, or regulatory issues. There are three types of FVD based on electrolyte losses: isotonic, hypertonic, and hypotonic. Manifestations include weight loss, decreased skin turgor, orthostatic hypotension, and multi-system effects. Diagnostics include labs to check electrolytes, hematocrit, urine specific gravity, and central venous pressure. Treatment aims to replace fluid and electrolyte losses based on the severity of the deficit.
Uploaded by
ajCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
169 views37 pagesFluid Volume Impairment Lecture
This document discusses fluid volume deficit (FVD), which occurs when there is a decrease in intravascular, interstitial, and/or intracellular fluid in the body. FVD can be caused by excessive fluid losses, insufficient intake, or regulatory issues. There are three types of FVD based on electrolyte losses: isotonic, hypertonic, and hypotonic. Manifestations include weight loss, decreased skin turgor, orthostatic hypotension, and multi-system effects. Diagnostics include labs to check electrolytes, hematocrit, urine specific gravity, and central venous pressure. Treatment aims to replace fluid and electrolyte losses based on the severity of the deficit.
Uploaded by
ajCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd