0% found this document useful (0 votes)
143 views10 pagesAmiodacore: Usage, Warnings, and Dosage
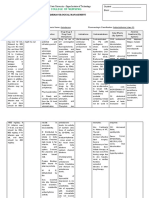
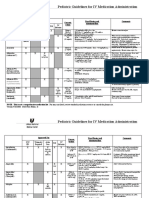
This document summarizes the product characteristics of the medicinal product AMIODACORE, which contains 200 mg of amiodarone hydrochloride per tablet. It is indicated for coronary insufficiency arrhythmias resistant to other treatments. The initial dosage is 3 tablets per day for 8-10 days, with maintenance between 1/2 to 2 tablets daily. Adverse reactions can affect the eyes, heart, lungs, liver, thyroid and skin. Regular monitoring of ECG and thyroid function is required during treatment.
Uploaded by
ddandan_2Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
143 views10 pagesAmiodacore: Usage, Warnings, and Dosage
This document summarizes the product characteristics of the medicinal product AMIODACORE, which contains 200 mg of amiodarone hydrochloride per tablet. It is indicated for coronary insufficiency arrhythmias resistant to other treatments. The initial dosage is 3 tablets per day for 8-10 days, with maintenance between 1/2 to 2 tablets daily. Adverse reactions can affect the eyes, heart, lungs, liver, thyroid and skin. Regular monitoring of ECG and thyroid function is required during treatment.
Uploaded by
ddandan_2Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd