Post Traumatic Sizure
Uploaded by
spiritPost Traumatic Sizure
Uploaded by
spirit| 24.07.
19 - 07:12
480 Seizures
common before or during adolescence). A CT or MRI (without and with enhancement) should be
performed. A systemic work-up should be done to identify the presence of any factors listed previ-
ously (see above). If all this is negative, then an MRI should be performed if not already done. If this
is negative also, a repeat study (CT or MRI) should be done in ≈ 6 months and at 1 and possibly 2
years to rule out a tumor which might not be evident on the initial study.
Pediatrics
Among pediatric patients with first-time seizures, laboratory and radiologic evaluations were often
costly and not helpful.4 A detailed history and physical exam were more helpful.
Management
Management of an adult with the new onset of idiopathic seizures (i.e., no abnormality found on CT
or MRI, no evidence of drug withdrawal) is controversial. In one study, an EEG was performed,
which, if normal, was followed by a sleep deprived EEG with the following observations6:
1. there is substantial interobserver variation in interpreting such EEGs
2. if both EEGs were normal, the 2-yr recurrence rate of seizures was 12%
27 3. if one or both EEGs showed epileptic discharges, the 2-yr recurrence rate was 83%
4. the presence of nonepileptic abnormalities in one or both EEGs had a 41% 2-yr recurrence rate
5. the recurrence rate with focal epileptic discharges (87%) was slightly higher than for generalized
epileptic discharges (78%)
The conclusion is that EEGs thus obtained have moderate predictive value, and may be factored into
the decision of whether or not to treat such seizures with AEDs.
27.2 Posttraumatic seizures
27.2.1 General information
Key concepts
● 2 categories: early (≤ 7 days) and late (> 7 days) after head trauma
● anticonvulsants (AEDs) may be used to prevent early posttraumatic seizures (PTS) in patients at
high risk for seizures
● prophylactic AEDs do NOT reduce the frequency of late PTS
● discontinue AEDs after 1 week except for cases meeting specific criteria (see text)
Posttraumatic seizures (PTS) are often divided (arbitrarily) into: early (occurring within 1 week of
injury) and late (thereafter).7 There may be justification for a third category: “immediate,” i.e., within
minutes to an hour or so.
27.2.2 Early PTS (≤ 7 days after head trauma)
30% incidence in severe head injury (“severe” defined as: LOC > 24 hrs, amnesia > 24 hrs, focal neuro
deficit, documented contusion, or intracranial hematoma) and ≈ 1% in mild to moderate injuries.
Occurs in 2.6% of children < 15 yrs of age with head injury causing at least brief LOC or amnesia.8
Early PTS may precipitate adverse events as a result of elevation of ICP, alterations in BP, changes
in oxygenation, and excess neurotransmitter release.9
27.2.3 Late onset PTS (< 7 days after head trauma)
Estimated incidence 10–13% within 2 yrs after “significant” head trauma (includes LOC > 2 mins,
GCS < 8 on admission, epidural hematoma…) for all age groups.10,11 Relative risk: 3.6 times control
population. Incidence in severe head injury > moderate > mild.8
The incidence of early PTS is higher in children than adults, but late seizures are much less fre-
quent in children (in children who have PTS, 94.5% develop them within 24 hrs of the injury12). Most
patients who have not had a seizure within 3 yrs of penetrating head injury will not develop
| 24.07.19 - 07:12
Special Types of Seizures 481
seizures.13 Risk of late PTS in children does not appear related to the occurrence of early PTS (in
adults: only true for mild injuries). Risk of developing late PTS may be higher after repeated head
injuries.
27.2.4 Penetrating trauma
The incidence of PTS is higher with penetrating head injuries than with closed head injuries (occurs
in 50% of penetrating trauma cases followed 15 yrs14).
27.2.5 Treatment
General information
Some early retrospective studies suggested that early administration of PHT prevents early PTS, and
reduces the risk of late PTS even after discontinuation of the drug. Later prospective studies disputed
this but were criticized for not maintaining satisfactory levels and for lacking statistical power.7,11 A
prospective double blind study of patients at high risk of PTS (excluding penetrating trauma) showed
a 73% reduction of risk of early PTS by administering 20 mg/kg loading dose of PHT within 24 hrs of
injury and maintaining high therapeutic levels; but after 1 week there was no benefit in continuing 27
the drug (based on intention to treat).15 Carbamazepine (Tegretol®) has also been shown to be effec-
tive in reducing the risk of early PTS.
Phenytoin has adverse cognitive effects when given long-term as prophylaxis against PTS.16
Treatment guidelines
Based on available information (see above) it appears that:
1. no treatment studied effectively impedes epileptogenesis (i.e., neuronal changes that ultimately
lead to late PTS)
2. in high-risk patients (▶ Table 27.1), AEDS reduce the incidence of early PTS
3. however, no study has shown that reducing early PTS improves outcome17
4. once epilepsy has developed, continued AEDs reduce the recurrence of further seizures
The following are therefore offered as guidelines.
Initiation of AEDs
AEDs may be considered for short term use, especially if a seizure could be detrimental. Early post-
traumatic seizures were effectively reduced when phenytoin was used for 2 weeks following head
injury with no significant increased risk of adverse effects.18
Acutely, seizures may elevate ICP, and may adversely affect blood pressure and oxygen delivery,
and may worsen other injuries (e.g. spinal cord injury in the setting of an unstable cervical spine).
There may also be negative psychological effects on the family, loss of driving privileges, and possibly
deleterious effects of excess neurotransmitters.9
Option: begin AEDs (usually levetiracetam, phenytoin or carbamazepine) within 24 hrs of injury
in the presence of any of the high risk criteria shown in ▶ Table 27.1 (modified9,12,15,19). When using
PHT, load with 20 mg/kg and maintain high therapeutic levels. Switch to phenobarbital if PHT is not
tolerated.
Discontinuation of AEDs
1. taper AEDs after 1 week of therapy except in the following cases:
a) penetrating brain injury
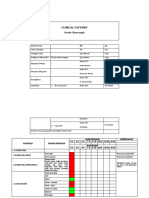
Table 27.1 High risk criteria for PTS
1. acute subdural, epidural, or intracerebral hematoma (SDH, EDH or ICH)
2. open-depressed skull fracture with parenchymal injury
3. seizure within the first 2 4 hrs after injury
4. Glasgow Coma Scale score < 1 0
5. penetrating brain injury
6. history of significant alcohol abuse
7. ± cortical (hemorrhagic) contusion on CT
| 24.07.19 - 07:12
482 Seizures
b) development of late PTS (i.e., a seizure > 7 days following head trauma)
c) prior seizure history
d) patients undergoing craniotomy20
2. for patients not meeting the criteria to discontinue AEDs after 1 week (see above):
a) maintain ≈ 6–12 mos of therapeutic AED levels
b) recommend EEG to rule out presence of a seizure focus before discontinuing AEDs (shown to
have poor predictive value, but probably advisable for legal purposes) for the following:
● repeated seizures
● presence of high risk criteria shown in ▶ Table 27.1.
27.3 Alcohol withdrawal seizures
27.3 .1 General information
Also, see Alcohol withdrawal syndrome (p. 219). The withdrawal syndrome may begin hours after
the EtOH peak; see also prevention and treatment (p. 220). Ethanol withdrawal seizures are classi-
cally seen in up to 33% (some say 75%) of habituated drinkers within 7–30 hours of cessation or
reduction of ethanol intake. They typically consist of 1–6 tonic-clonic generalized seizures without
27 focality within a 6 hour period.21 Seizures usually occur before delirium develops. They may also
occur during intoxication (without withdrawal).
The seizure risk persists for 48 hrs (risk of delirium tremens (DTs) continues beyond that); thus a
single loading dose of PHT is frequently adequate for prophylaxis. However, since most EtOH with-
drawal seizures are single, brief, and self-limited, PHT has not been shown to be of benefit in uncom-
plicated cases and is thus usually not indicated. Chlordiazepoxide (Librium®) or other
benzodiazepines (p. 220) administered during detoxification reduces the risk withdrawal seizures.22
27.3 .2 Evaluation
The following patients should have a CT scan of the brain, and should be admitted for further evalua-
tion as well as for observation for additional seizures or for DTs:
1. those with their first EtOH withdrawal seizure
2. those with focal findings
3. those having more than 6 seizures in 6 hrs
4. those with evidence of trauma
Other causes of seizure should also be considered, e.g. a febrile patient may require an LP to rule out
meningitis.
27.3 .3 Treatment
A brief single seizure may not warrant treatment, except as outlined below. A seizure that continues
beyond 3–4 minutes may be treated with diazepam or lorazepam, with further measures used as in
status epilepticus (p. 486) if seizures persist. Loading with phenytoin (18 mg/kg = 1200 mg/70 kg)
and long-term treatment is indicated for:
1. a history of previous alcohol withdrawal seizures
2. recurrent seizures after admission
3. history of a prior seizure disorder unrelated to alcohol
4. presence of other risk factors for seizure (e.g. subdural hematoma)
27.4 Nonepileptic seizures
27.4.1 General information
AKA pseudoseizures (some prefer not to use this term since it may connote voluntary feigning of
seizures), with the term psychogenic seizures being preferred for nonepileptic seizures (NES) with a
psychologic etiology (psychogenic seizures are real events and may not be under voluntary
control).23
One of the hazards of NES is that patients may end up needlessly taking AEDs, which in some
cases may worsen NES. Possible etiologies of NES are given in ▶ Table 27.2. Most NES are
psychogenic.
DDx for seizures:
You might also like
- As Treatment Options For Shunt Migration To Scrotum: Case Report" by JanuarmanNo ratings yetAs Treatment Options For Shunt Migration To Scrotum: Case Report" by Januarman1 page
- Clinical Pathway Avm - Embolisasi - TrepanasiNo ratings yetClinical Pathway Avm - Embolisasi - Trepanasi5 pages