0% found this document useful (0 votes)
56 views1 pageNewborn Resuscitation for COVID-19
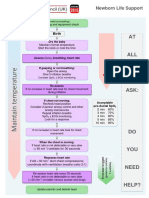
Newborn Life Support for COVID-19 patients outlines guidelines for resuscitation of newborns born to mothers with suspected or confirmed COVID-19. The approach is unchanged, but additional precautions are recommended including consideration of team composition, aerosol PPE, and resuscitation location. If the newborn is not breathing or heart rate is slow, providers should open the airway, give inflation breaths, and monitor oxygen levels, reassessing every 30 seconds. If there is no increase in heart rate despite effective ventilation, chest compressions should be started and coordinated with breaths at a 3:1 ratio. The newborn's care and potential transfer to the NICU also requires planning for adequate protection of staff
Uploaded by
Hubert AnusCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
56 views1 pageNewborn Resuscitation for COVID-19
Newborn Life Support for COVID-19 patients outlines guidelines for resuscitation of newborns born to mothers with suspected or confirmed COVID-19. The approach is unchanged, but additional precautions are recommended including consideration of team composition, aerosol PPE, and resuscitation location. If the newborn is not breathing or heart rate is slow, providers should open the airway, give inflation breaths, and monitor oxygen levels, reassessing every 30 seconds. If there is no increase in heart rate despite effective ventilation, chest compressions should be started and coordinated with breaths at a 3:1 ratio. The newborn's care and potential transfer to the NICU also requires planning for adequate protection of staff
Uploaded by
Hubert AnusCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd