Pediatric Advanced Life
Support
2020 AHA GUIDELINES
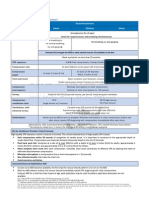
� BLS Assessment:
Minimize delay by checking the breathing & Pulse simultaneously no more than 10-
seconds.
To perform Pulse check:
o For infants check brachial pulse by placing two fingers under upper arm &
shoulder.
o For children check femoral pulse. (Diagram below)
o
o When checking pulses no longer than 10-seconds but at least 5-seconds.
CPR in Infants & Children with an Advanced
Airway:
Target a respiratory rate range of 1-breath every 2-3 seconds.
20-30 breaths per minute
CUFFED VS UNCUFFED ENDOTRACHEAL TUBES:
The attention should be paid to the ETT size, position, & Cuff inflation
pressure.
Intubation with a Cuffed Endotracheal Tube:
− Improves capnography and ventilation.
− Decreases the need for endotracheal tube changes.
− Decreases the need for reintubation.
− Improves successful ventilation and accuracy of capnography.
− Decreases the risk of aspiration.
PAGE 1
� CRICOIDE PRESSURE DURING INTUBATION:
Routine Use of Cricoid Pressure:
Reduces the rate of first attempt intubation success.
Impedes the visualization during laryngoscopy and chest rise with
bag-mask ventilation.
Routine use of cricoid pressure is NOT recommended during
endotracheal intubation of pediatric patients.
Early Epinephrine During CPR:
Optimizes coronary perfusion pressure.
− Maintains cerebral perfusion pressure.
− Increases survival to discharge rates.
− For pediatric patients in any setting, it is reasonable to administer the
initial dose of epinephrine with in 5-minutes after the start of chest
compressions.
DIASTOLIC BLOOD PRESSURE TO GUIDE CPR:
It is reasonable for providers to use diastolic blood pressure to assess
CPR quality.
Diastolic Blood Pressure is a marker of adequate blood flow during
CPR, and it may be used if an arterial line is in place.
Seizures after Cardiac Arrest:
Continuous electroencephalography monitoring is recommended for
detecting seizures after cardiac arrest in patients with persistent
EEG.
It is recommended to treat clinical seizures that follow cardiac arrest.
SEPTIC SHOCK:
It is reasonable to administer fluid boluses in aliquots of 10 o 20
mL/kg with frequent reassessment.
PAGE 2
� After fluid bolus, providers should reassess the patient for fluid
responsiveness & signs of volume overload.
In infants and children with fluid-refractory septic shock, it’s
reasonable to use either epinephrine or norepinephrine as an initial
vasoactive infusion.
Opioid Overdose:
Pediatric opioid overdose management is the same as it is for adults.
For a patient with suspected opioid overdose who has a definite pulse
but no normal breathing or is only gasping, administer intramuscular
or intranasal naloxone along with standard basic life support care.
BASIC LIFE SUPPORT:
In Hospital Cardiac Arrest (IHCA):
o Early Recognition
o Activation of the emergency response
o High-Quality CPR
o Advanced Resuscitation
o Post Cardiac Arrest Care
o Recovery
Out-of-Hospital Cardiac Arrest (OHCA)
o Prevention
o Activation of the Emergency Response
o High-Quality CPR
o Advanced Resuscitation
o Post Cardiac Arrest Care
o Recovery
Instruction CPR- Child:
Verify Scene Safety
Check Responsiveness
Shout for help/Activate emergency response system.
Check breathing and pulse (at least 5 seconds but no more than 10-
seconds)
Start Compressions
C-A-B:
PAGE 3
� o Compressions
o Airway
o Breathing
Compressions:
o BLS Guidelines define anyone from age 1 year to puberty as a
child.
o For infants and prepubescent children, depress the chest at
least 1/3 of the AP diameter of the chest.
o For Children, depress approximately 2-inches, or 5cm
o Allow a complete recoil.
o 1-rescuer CPR:
30:2 Compression to ventilation ratio.
o 2-rescuer CPR:
15:2 Compression-to-ventilation ratio
PEDIATRIC BLS- BAG-MASK DEVICE:
Instruction:
o Deliver one breath over 1 second.
100-120 compressions per minute.
During CPR with an advanced airway, give one breath every 2-3
seconds.
Don’t pause compressions to give breaths.
AED:
Make Sure you attach the pads appropriately.
Turn on the AED
Attach the Pads to the patient
Analyze the heart rhythm.
Deliver a shock.
o If someone is lying In water, move them to a dry area.
o If someone is lying in snow or a small puddle, you may use the
AED.
o If chest is covered with water or sweat, wipe the chest dry
before attaching the pads.
o Side Note:
If you DO NOT witness the arrest, are alone, and do not
have a mobile phone, shout for help, but perform 5-cycles
of CPR before you leave to activate the emergency
response system.
PAGE 4
� If you DO witness the arrest and are alone, & don’t have
a mobile phone, leave the child, activate the emergency
response system, get the AED, and return to perform
CPR.
If there are multiple rescuers, the first rescuer should
remain with the child and begin CPR. The other rescuers
should activate the emergency response system and
retrieve the AED.
CPR INSTRUCTIONS INFANT:
o Check for pulse for at least 5-seconds and no more than 10-
seconds.
o Compress to a depth of at least one third the depth of the chest.
(1.5 inches or 4 cm )
o Compress at a rate of 100 to 120 compressions per minute.
o Allow the chest to recoil completely.
o 2-Rescuer:
Compress to a depth of 1/3 depth of chest.
15:2 compression to ventilation ratio.
CPR INSTRUCTIONS CHILDREN:
o Check for pulse for at least 5-seconds and no more than 10-
seconds.
o Compress to a depth of at least one third the depth of the chest.
(2- inches 1/3 of AP Diameter )
o Compress at a rate of 100 to 120 compressions per minute.
o Allow the chest to recoil completely.
o 2-Rescuer:
Compress to a depth of 1/3 depth of chest.
15:2 compression to ventilation ratio.
Choking Child Relief:
Signs:
Silent cough
Inability to speak or breathe.
Cyanosis (Turning Blue)
o If attempts are unsuccessful and the child becomes unresponsive,
activate the emergency response system, and begin CPR.
o Do not perform a blind finger sweep, because this may cause the
object to become lodged further back in the airway.
Infant Choking Relief:
PAGE 5
� o Do not perform a blind finger sweep.
o If you are alone, After 2-minutes or 5-cycles of CPR, activate the
emergency response system.
SYSTEMIC APPROACH:
Evaluate:
o Initial assessment, primary assessment, & secondary
assessment.
Identify and Intervene as appropriate.
Managemen Signs of Instability with arrhythmia:
t of
Respiratory distress or failure.
Arrhythmia
Shock with poor end-organ perfusion with or without
Emergencie
hypotension.
s:
Irritability or a decreased level of consciousness
Chest pain or vague feeling of discomfort
Sudden Collapse.
Most common Pediatric arrhythmia’s:
Sinus Bradycardia
Atrioventricular Block (AV)
Sinus Tachycardia
Supraventricular Tachycardia (SVT)
Sinus Bradycardia:
Initial Treatment of Sinus bradycardia is bag mask
ventilation with 100% oxygen.
If heart rate is less than 60 BPM with poor perfusion,
start CPR.
Consider atropine or epinephrine.
AV Block:
AV-Block is a delay in the conduction of the electrical
impulse through the heart caused by the AV node.
Sinus Tachycardia:
Sinus tachycardia is a rapid heart rate that develops
PAGE 6
� when high cardiac output is needed.
Sinus Ventricular Tachycardia (SVT):
SVT is an abrupt increase in heart rate that does not
vary with activity.
Ventricular Tachycardia:
ABC:
Airway, Breathing, Circulation.
Vagal Maneuver:
Obtain a 12-lead ECG before and after the maneuver.
Don’t delay definitive treatment to perform vagal
maneuvers.
A rapid bolus of the drug immediately flushed with 5-10
mL of Normal saline bolus.
Synchronized Cardioversion:
Synchronized Cardioversion is an electrical therapy
used to convert tachyarrhythmias with a pulse to a
sinus rhythm.
Failure to synchronize the defibrillator may cause
ventricular fibrillation.
Establish vascular access, and provide procedural
analgesia and sedation.
Initial energy dose between 05. And 1 J/kg
Increase to 2 J/kg for subsequent shocks.
If Ventricular fibrillation or pulselessness ventricular
tachycardia develop, begin CPR and unsynchronized
shock.
Cardiac Cardiac Arrest:
Arrest:
Cardiac arrest is the cessation of blood circulation
resulting from absent or ineffective cardiac mechanical
activity.
Cardiac Arrest Rhythms:
PAGE 7
� Asystole
Pulselessness Electrical Activity (PEA)
Ventricular fibrillation
Pulselessness ventricular tachycardia
PEA:
Organized electrical activity is present on the cardiac
monitor, but the patient remains pulseless.
Asystole, V-fib, and V-tach:
Are not organized electrical activity.
H’s and T’s:
Hypoglycemia
Hypovolemia
Hypoxia
Hydrogen Ion (Acidosis)
Hyperkalemia
Hypokalemia
Hypothermia
Tension Pneumothorax
Cardiac Tamponade
Toxins
Pulmonary Thrombosis
Coronary Thrombosis
Defibrillation:
Energy levels are higher for this.
Appropriate Energy Dose:
First Defibrillation: 2-4 J/kg
Second Defibrillation: 4 J/kg
Subsequent Defibrillations: 4-10 J/kg
2,4,6,8: That’s the dose to defibrillate.
Each shock should not exceed the starting or
subsequent adult defibrillation dose for that specific
defibrillator model.
PAGE 8
� Managing Evaluate:
Respiratory
Evaluate: Primary assessment, Secondary Assessment,
Emergencie
Diagnostic Tests.
s:
Identify
Intervene
Types of Respiratory Problems:
Upper airway obstruction
Lower Airway obstruction
Lung Tissue Disease
Disordered control of Breathing.
Signs of Increased Effort:
Retractions and Nasal Flaring
Upper Airway Obstruction:
Inspiratory Stridor
Hoarseness
Barking Cough
Drooling
Snoring
Gurgling Sounds
Decreased Air Movement:
Prolonged Exhalation
Expiratory Wheezes
Lung Tissue Disease:
Grunting
Crackles
Decreased air movement
Disordered Control of Breathing:
Slow respiratory rate
Shallow Breathing
PAGE 9
� Normal or Decreased Air Movement
Oxygen Concentration Delivery is Determined By:
Childs Size
Oxygen Flow Rate
Breathing Volume
Respiratory Rate
The lower the oxygen flow, the lower the inspired
oxygen concentration.
Nasal Cannula: Used with flow rates of ¼ to 4 LPM
Face Mask: Requires at least 6-LPM
High Flow Systems:
Tightly Sealed against the face.
1-way valve (Allows exhalation, but no entrainment of
room air)
Reservoir Bag
Consistently deliver a high concentration of oxygen
Flow rate must be 10-15 LPM
Complications from Suctioning:
Hypoxia
Vagal Stimulation
Bradycardia
Gagging and vomiting
Soft tissue injury
Agitation
During Suctioning:
Monitor:
Heart Rate
Oxygen Saturation
Clinical Appearance
Oropharyng Insertion of Advanced Airway:
eal Airway
Difficulty providing effective bag-mask ventilation.
Actual or Potential airway compromise.
Protection of the airway.
Advantages of Advanced Airways:
PAGE 10
� Reducing the risk of aspiration and gastric insufflation.
Eliminating need to interrupt chest compressions
during CPR.
During CPR deliver 1-Breathe Q 6 seconds asynchronously.
Endotracheal Tube Complications:
Trauma to oropharynx
Incorrect Placement
Esophagus or Bronchus
PAGE 11
� Side Notes
If pt doesn’t have normal breathing and has a pulse of 64-BPM provide rescue breathing.
If unwitnessed cardiac arrest occurs, do 2-minutes of CPR and then call for help.
Compression vs Ventilation Ratio:
Universal rate for compressions is 100-120 BPM
Single-Rescuer is 30:2
2-Rescuers is 15:2
Most children use two-hands to compress chest.
You can use one hand if child’s chest/body is small enough to.
Small children use 1-hand compress 1/3 of child’s chest approximately 2-inches or 5-cm
each compression.
ABNORMAL BREATH SOUNDS
• Upper airway obstruction (foreign
STRIDOR
body)
• Upper airway obstruction
(Swollen airway)
GRUNTING
• Pneumonia (grunting to recruit
alveoli)
• Lower airway obstruction
WHEEZING
(Asthma)
• Fluid in lungs (Wet), Atelectasis
CRACKLES
(Dry)
PAGE 12
�ABSENT/DECREASED • Collapsed lung (air, blood)
BREATH SOUNDS • Lung tissue disease (pneumonia)
Primary Assessment: Breathing:
Nasal Flaring:
o Dilation of the nostrils with each inhalation to maximize airflow. Most observed
in infants/younger children. Sign of respiratory distress.
Retractions:
o Enter
Retractions:
o Enter
Retractions:
o Enter
CPR in Infants & Children With an Advanced
Airway:
Target a respiratory rate range of 1-breath every 2-3 seconds.
20-30 breaths per minute
Notes from pre-test/Post test:
1. The most common cause of cardiac arrest in pediatric patients is:
a. Respiratory failure
b. Respiratory failure is the most common cause of respiratory
failure and cardiac arrest. If the intervention is not done early
and aggressively, the outcome for the child is usually very poor.
2. After stabilizing a patient in respiratory failure, the most important
clinical goal is:
a. Identify and treat the disease that is causing the respiratory
failure
b. After establishing clinical stabilization of the patient in
respiratory failure, it is essential to determine the cause of the
respiratory failure and begin aggressive treatment. Simply
PAGE 13
� maintaining adequate minute ventilation with a ventilator will
do nothing to treat an underlying condition such as bacterial
pneumonia. Obviously, antibiotic therapy is the proper
treatment, not the mechanical ventilator.
3. Where should you check for a peripheral pulse?
a. Upper arm (brachial)
b. The brachial artery is a major blood vessel located in the upper
arm.
4. Remembering which of the following acronyms will help you assess a
child’s mental status?
a. AVPU
5. Which of the following drugs should you consider using to treat a
child showing supraventricular tachycardia (SVT)?
a. Adenosine
b. Pediatric patients should be given adenosine for the treatment
of SVT. The first recommended dose is 0.1 mg/kg up to a
maximum of 6 mg. The second recommended dose is 0.2 mg/kg
up to a maximum of 12 mg.
6. After establishing an advanced airway (i.e. endotracheal tube, etc.),
there is no need to provide CPR in cycles. CPR should continue at 100
compressions/minute with 8-10 ventilations provided.
a. True
b. CPR should continue at 100 compressions/minute with 8-10
ventilations provided.
7. Which of the following arrhythmias are/or may be life threatening for
pediatric patients?
a. Ventricular tachycardia, Torsades de pointes, Ventricular
fibrillation
b. All three arrhythmias listed are/can be life threatening if left
untreated.
8. If treating a 10-kg infant with oxygen refractory unstable bradycardia,
how much epinephrine should be administered?
a. 1.0 ml of 1:10,000 solution
PAGE 14
� b. The recommended dose of epinephrine is 0.1 ml/kg of the
1:10,000 solution. Expressed in mg: 0.01 mg/kg. The 1:1,000
solution can be used diluted for administration down the ET
tube, or it can be administered by subcutaneous injection.
Epinephrine can also be given via the intraosseous route.
9. Pediatric patients who develop “unstable” supraventricular or
ventricular tachycardia should immediately receive electrical
cardioversion.
a. True
b. When an arrhythmia reduces cardiac output, and signs of shock
and deterioration can be seen, electrical cardioversion should
be undertaken immediately. Left untreated, a patient with an
unstable tachycardia could end up in cardiac arrest.
10.A young trauma patient is brought into your emergency department,
barely responsive, pale, with an 8 second capillary refill. The abdomen
is distended and rigid. Stat hemoglobin comes back 5.1 gm. What
would be the ideal fluid to treat this patient’s hypovolemic shock?
a. Whole blood or packed cells
b. Although normal saline or Lactated Ringer’s Solution are
commonly used in hypovolemia caused by hemorrhage, it is
only because blood is not immediately available. Crystaloid
solutions contain no red blood cells. Because red blood cells
carry the majority of oxygen to tissues, it is essential to replete
lost red blood cells as soon as possible.
PAGE 15