0% found this document useful (0 votes)
40 views7 pagesReducing ICU Patient Anxiety: Effective Interventions
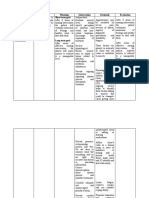
The document discusses anxiety in hospitalized patients in the ICU and explores various nursing interventions to alleviate this anxiety. It highlights the importance of understanding patients' emotional needs and presents research on effective strategies such as transition nursing programs, the presence of care companions, improving sleep quality, and music therapy. The conclusion emphasizes that nurses can significantly impact patients' anxiety levels through active listening and supportive care beyond medication.
Uploaded by
gf97fjyq4kCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
40 views7 pagesReducing ICU Patient Anxiety: Effective Interventions
The document discusses anxiety in hospitalized patients in the ICU and explores various nursing interventions to alleviate this anxiety. It highlights the importance of understanding patients' emotional needs and presents research on effective strategies such as transition nursing programs, the presence of care companions, improving sleep quality, and music therapy. The conclusion emphasizes that nurses can significantly impact patients' anxiety levels through active listening and supportive care beyond medication.
Uploaded by
gf97fjyq4kCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd