0% found this document useful (0 votes)
19 views66 pagesHeart Failure
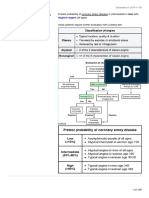
The document provides a comprehensive overview of heart failure, including its definitions, classifications, causes, and clinical features. It emphasizes the distinction between systolic and diastolic heart failure, the importance of ejection fraction, and the various diagnostic investigations and treatment options available. Additionally, it outlines the learning objectives for understanding heart failure and its management in different patient populations.
Uploaded by
Obinna AnakwueCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
19 views66 pagesHeart Failure
The document provides a comprehensive overview of heart failure, including its definitions, classifications, causes, and clinical features. It emphasizes the distinction between systolic and diastolic heart failure, the importance of ejection fraction, and the various diagnostic investigations and treatment options available. Additionally, it outlines the learning objectives for understanding heart failure and its management in different patient populations.
Uploaded by
Obinna AnakwueCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd