0% found this document useful (0 votes)
74 views51 pagesProblem Solving Exercises
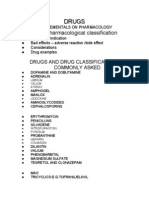
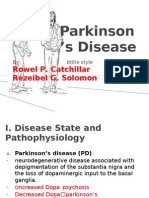
The document discusses various clinical scenarios involving drug interactions and side effects, particularly focusing on patients with conditions like alcoholism, hypertension, myasthenia gravis, angina pectoris, and depressive psychosis. It highlights the importance of understanding drug mechanisms, potential adverse reactions, and appropriate management strategies. Additionally, it emphasizes the need for careful monitoring and adjustment of treatments to prevent complications and ensure patient safety.
Uploaded by
vishnupriya21012005Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
74 views51 pagesProblem Solving Exercises
The document discusses various clinical scenarios involving drug interactions and side effects, particularly focusing on patients with conditions like alcoholism, hypertension, myasthenia gravis, angina pectoris, and depressive psychosis. It highlights the importance of understanding drug mechanisms, potential adverse reactions, and appropriate management strategies. Additionally, it emphasizes the need for careful monitoring and adjustment of treatments to prevent complications and ensure patient safety.
Uploaded by
vishnupriya21012005Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd