0% found this document useful (0 votes)
298 views34 pagesUnderstanding Acid-Base Disorders
This document discusses acid-base disorders and provides information on:
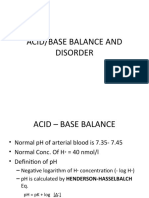
1. The body aims to maintain a narrow pH range of 7.35-7.45 through buffering mechanisms involving the lungs and kidneys.
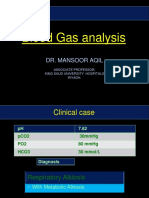
2. Blood gas analysis is used to measure pH, PaCO2, PaO2 and HCO3 levels to assess a patient's acid-base status.
3. Respiratory and renal systems work to balance acids and bases in the body through regulating carbon dioxide and bicarbonate levels respectively.
4. Disturbances can cause metabolic acidosis, alkalosis or respiratory acidosis, alkalosis - each with defining blood gas patterns and clinical impacts.
Uploaded by
anon-252165Copyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPT, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
298 views34 pagesUnderstanding Acid-Base Disorders
This document discusses acid-base disorders and provides information on:
1. The body aims to maintain a narrow pH range of 7.35-7.45 through buffering mechanisms involving the lungs and kidneys.
2. Blood gas analysis is used to measure pH, PaCO2, PaO2 and HCO3 levels to assess a patient's acid-base status.
3. Respiratory and renal systems work to balance acids and bases in the body through regulating carbon dioxide and bicarbonate levels respectively.
4. Disturbances can cause metabolic acidosis, alkalosis or respiratory acidosis, alkalosis - each with defining blood gas patterns and clinical impacts.
Uploaded by
anon-252165Copyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPT, PDF, TXT or read online on Scribd