100% found this document useful (1 vote)
186 views69 pagesTLS Final
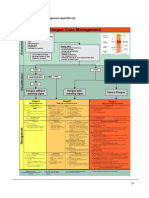
The document discusses tumour lysis syndrome, including its causes, signs and symptoms, risk factors, classification, investigations, and management. It causes metabolic abnormalities when tumour cells are lysed, releasing potassium, phosphates and nucleic acids. The mainstays of prevention and treatment are intravenous hydration, hypouricemic agents like allopurinol or rasburicase, close monitoring, and management of any electrolyte abnormalities or acute kidney injury.
Uploaded by
Grace ArthurCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
100% found this document useful (1 vote)
186 views69 pagesTLS Final
The document discusses tumour lysis syndrome, including its causes, signs and symptoms, risk factors, classification, investigations, and management. It causes metabolic abnormalities when tumour cells are lysed, releasing potassium, phosphates and nucleic acids. The mainstays of prevention and treatment are intravenous hydration, hypouricemic agents like allopurinol or rasburicase, close monitoring, and management of any electrolyte abnormalities or acute kidney injury.
Uploaded by
Grace ArthurCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd