100% found this document useful (4 votes)
14K views61 pagesACLS
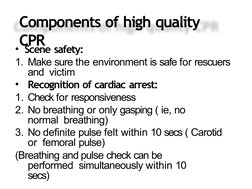
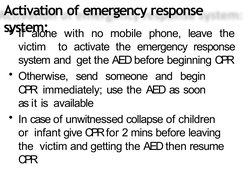
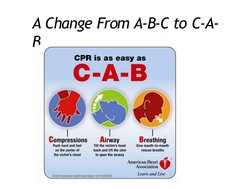
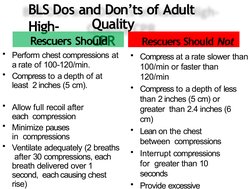
The document outlines guidelines for adult advanced cardiovascular life support, including the importance of high-quality CPR, use of adjuncts like supplemental oxygen and advanced airways, defibrillating shockable rhythms like ventricular fibrillation, and treating cardiac arrest based on the underlying rhythm. It emphasizes defibrillation for ventricular fibrillation/pulseless ventricular tachycardia and chest compressions for non-shockable rhythms like pulseless electrical activity and asystole.
Uploaded by
mgthida935Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
100% found this document useful (4 votes)
14K views61 pagesACLS
The document outlines guidelines for adult advanced cardiovascular life support, including the importance of high-quality CPR, use of adjuncts like supplemental oxygen and advanced airways, defibrillating shockable rhythms like ventricular fibrillation, and treating cardiac arrest based on the underlying rhythm. It emphasizes defibrillation for ventricular fibrillation/pulseless ventricular tachycardia and chest compressions for non-shockable rhythms like pulseless electrical activity and asystole.
Uploaded by
mgthida935Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
![Adult Advanced Cardiovascular Life Support
Circulation. 2015;132[suppl 2]:S444–S464](https://screenshots.scribd.com/Scribd/252_100_85/189/685302175/1.jpeg)